Right Hemicolectomy: Hand-Assisted Laparoscopic Surgery Technique
Matthew Albert
Harsha Polavarapu
DEFINITION
Hand-assisted laparoscopic surgery (HALS) is a hybrid technique, which allows the surgeon to insert his or her hand into the abdominal cavity through a relatively small incision while preserving the ability to work under pneumoperitoneum. This approach aids in tactile feedback, retraction, and dissection by hand assistance in turn eliminating the technical challenges of conventional laparoscopy while maintaining nearly all of its benefits.1,2
INDICATIONS
Colon cancer
Colon polyps not amenable to colonoscopic removal
Inflammatory bowel disease
Angiodysplasia
Recurrent right colonic diverticulitis
PATIENT HISTORY AND PHYSICAL FINDINGS
A thorough history should be taken, including a detailed past medical history, past surgical history, present medications and allergies, and a personal and family history of colon and rectal cancer.
A detailed family history to assess the risk of hereditary polyposis syndromes is critical in selecting the optimal procedure for the patient. Suspected patients should be offered genetic counseling and testing.
A detailed physical examination of the patient should be performed to identify any prior surgical incisions and palpable masses to plan for the operation.
The location, histopathology, and the clinical stage of the lesion is crucial prior to any planned procedure.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Colonoscopy remains the investigation of choice for localizing the target lesion, for obtaining tissue for histopathology, and for tattooing for intraoperative localization. This is also helpful in identifying synchronous lesions in the remaining colon.
Computed tomography (CT) scan of the chest/abdomen/pelvis with IV and oral contrast is recommended as the primary staging tool to assess for local organ invasion and for distant metastasis.3
Serum carcinoembryonic antigen (CEA) level is a valuable marker for postoperative surveillance.
Bone scan and brain imaging should be reserved for symptomatic patients only.
SURGICAL MANAGEMENT
The goal of surgery is an en bloc resection of the involved segment of bowel and to perform a high ligation of the vascular pedicle permitting adequate removal of associated lymphatics and lymph nodes.
At least 12 lymph nodes must be harvested to adequately stage the patient and to avoid risk of understaging.3
Preoperative Planning
Routine use of mechanical bowel preparation is not recommended.4
Deep vein thrombosis prophylaxis with sequential compression devices and subcutaneous heparin dosing before induction of anesthesia is administered.
A Foley catheter is placed prior to the operation.
Nasogastric/orogastric tube is placed prior to the operation.
Preoperative antibiotics covering skin and bowel flora are administered prior to induction of anesthesia.
Positioning
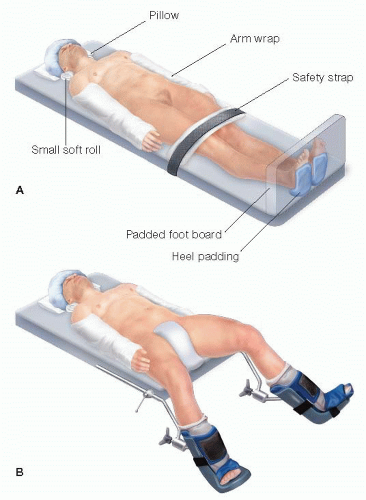
Patient is positioned in a supine position. In order to prevent the patient from sliding during the case, the arms are tucked to the sides, the feet are placed against a padded footboard, and a strap is placed over the thighs (FIG 1).
Alternatively, the patient can be placed in the low lithotomy position to avoid instrument conflict with the lower extremities. The knees should be slightly flexed and the feet firmly planted on the stirrups to prevent undue pressure on the calves and on the lateral peroneal nerves.
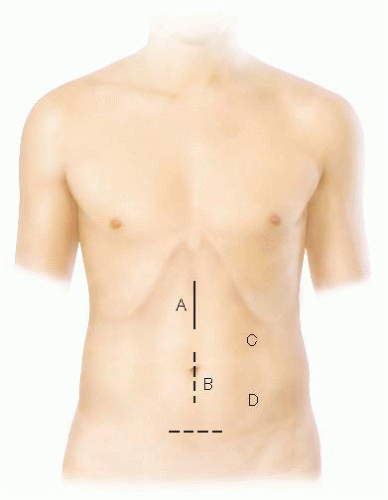
Depending on the location of pathology and body habitus, a 5- to 7-cm incision is made for the hand port in an epigastric, periumbilical, or Pfannenstiel location (FIG 2).
Location of the trocars can be variable based on surgeon’s preference. In general, it is best to triangulate all ports to enhance visualization and to prevent instrument conflict inside the abdomen.
A traditional port placement includes (FIG 2)
A GelPort hand port through a 6-cm epigastric incision
A 5-mm infraumbilical camera port
A 5-mm left lower quadrant instrument port
A 5-mm left upper quadrant/left anterior flank
TECHNIQUES
EXPOSURE
After placement of the hand port, the abdomen is explored to locate the lesion, to assess the extent of spread, and to palpate the liver and peritoneal cavity for distant metastatic spread.
In female patients, the ovaries should be examined for metastatic spread or primary neoplasms.
Pneumoperitoneum is created with carbon dioxide (CO2) and additional trocars are inserted.
Patient is placed in a left lateral tilt and slight Trendelenburg position. The small bowel is fanned out along its mesentery to aid in the exposure of the right colon.
The greater omentum along with the transverse colon is retracted cephalad.
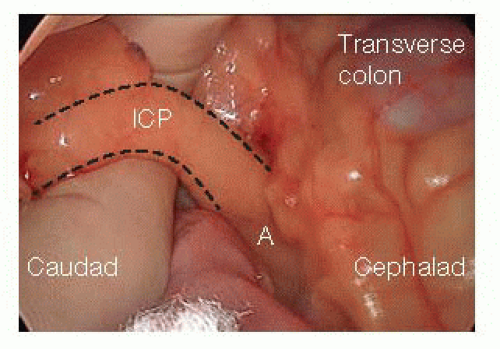
The cecum is grasped with the hand and retracted toward the anterior abdominal wall using gentle traction to identify the ileocolic vessels.
The ileocolic pedicle is grasped and retracted toward the anterior abdominal wall (FIG 3).
DIVISION OF ILEOCOLIC PEDICLE
With the ileocolic pedicle on stretch, a parallel incision is made on the peritoneal layer underneath the pedicle (FIG 4) extending to the root of the mesentery and the superior mesenteric vein, using monopolar electrocautery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree