Right and Left Colon Resections
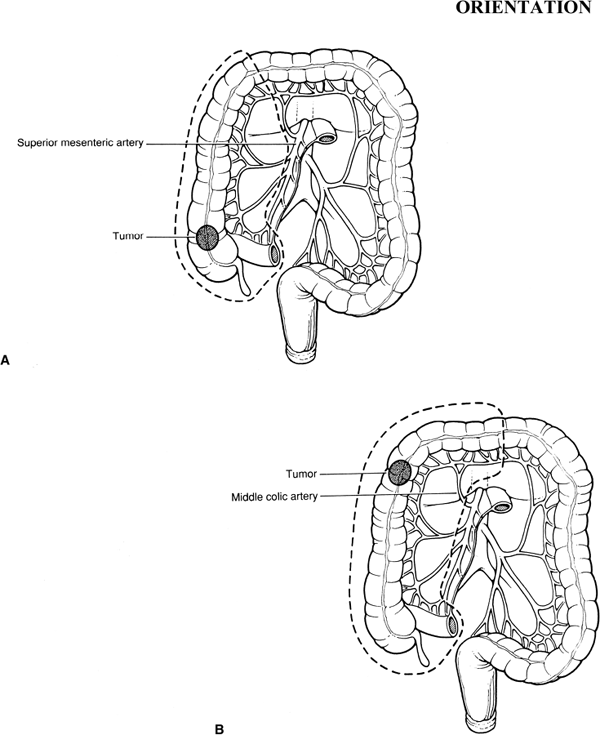
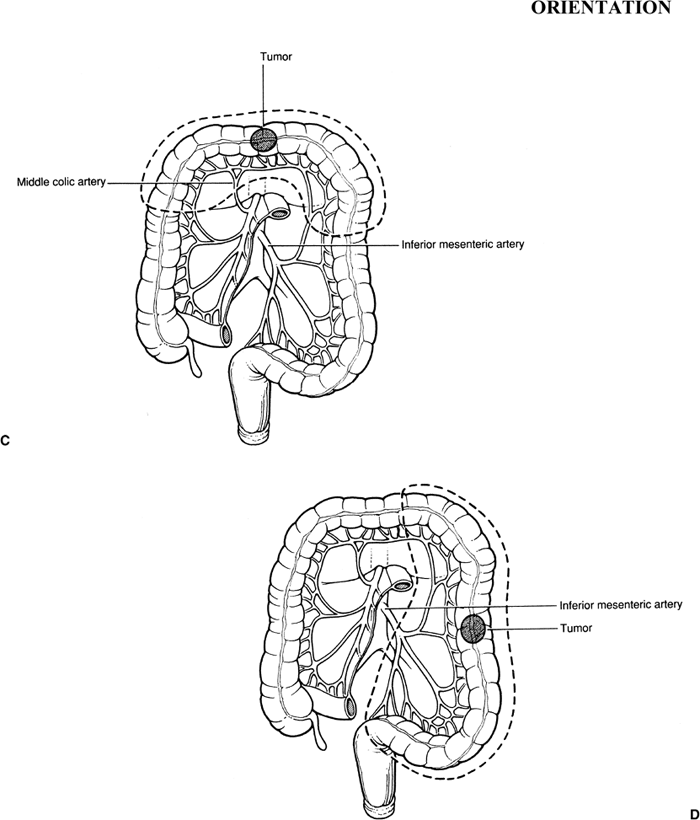
Resections of the colon are planned according to arterial supply and venous and lymphatic drainage. For lesions of the cecum or ascending colon up to and including the hepatic flexure, the standard resection is a right hemicolectomy. This includes resection of the terminal ileum, ascending colon, and right transverse colon. An end-to-end anastomosis is then performed between the ileum and transverse colon.
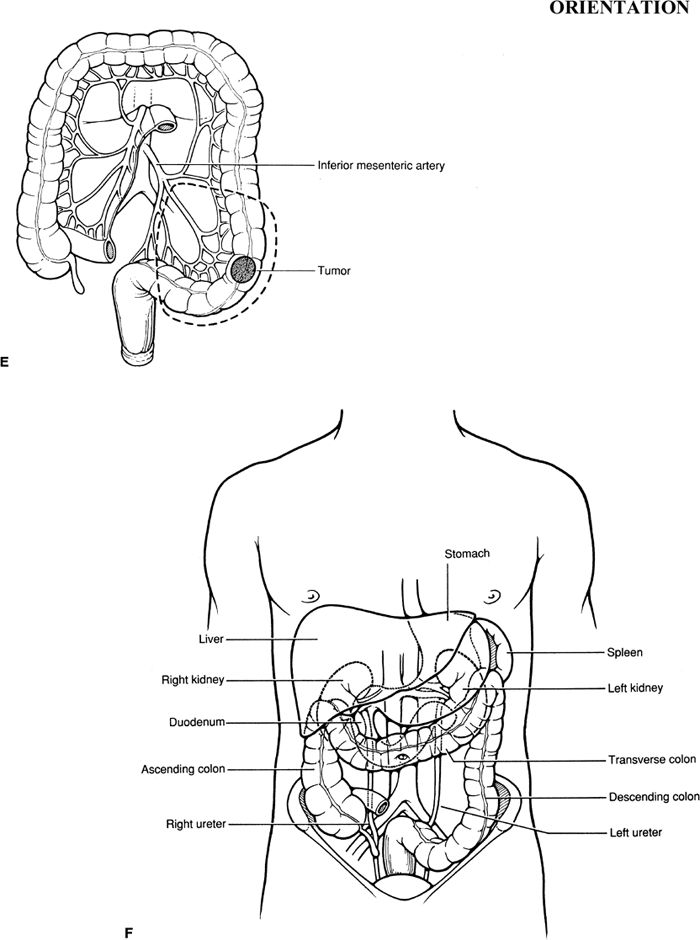
Left hemicolectomy is performed for lesions in the sigmoid or descending colon. The colon is resected from the middle of the transverse colon to the peritoneal reflection. This wide field of resection is needed when the inferior mesenteric vein and artery are ligated at their origin in order to resect lymph nodes along the inferior mesenteric artery. An end-to-end anastomosis is then performed between the middle of the transverse colon and the rectosigmoid.
Lesions involving the transverse colon can be managed by transverse colon resection, whereby the transverse colon, including both flexures, is removed and the ends are reanastomosed. In this chapter, right and left hemicolectomy is discussed, and transverse colon resection is mentioned briefly. In each case, the arterial and venous drainage of the segment determines the extent of resection.
More limited resections are occasionally performed for localized perforations or trauma. These are done in much the same manner but require a less extensive dissection. Chapter 82 describes laparoscopic colon resection. References at the end of this chapter give additional information on specialized procedures, including sentinel node biopsy, which is controversial at this time.
Steps in Procedure
Right Hemicolectomy
Right transverse or midline incision
Thoroughly explore abdomen
Mobilize right colon by incising along white line of Toldt
Elevate right colon in retrocolic plane
Identify and preserve duodenum and both ureters
At hepatic flexure, take greater omentum with specimen
Extent of resection is determined by location of tumor, but will generally include terminal ileum and transverse colon to middle colic artery
Preserve middle colic artery unless extended right hemicolectomy is planned
Score peritoneum overlying mesenteric vessels down to origin of ileocolic and right colic arteries, but preserving the superior mesenteric artery
Divide mesentery between clamps and ties
Divide bowel and create anastomosis by suturing or stapling
Close mesenteric defect
Place omentum over anastomosis
Close abdomen in usual fashion without drains
Left Hemicolectomy
Midline or left paramedian incision
Thorough abdominal exploration
Mobilize left colon by incision along white line of Toldt
At splenic flexure, take omentum off colon (unless tumor is in proximity to this region)
Identify and protect both ureters
Determine extent of resection, generally preserving middle colic artery unless extended left hemicolectomy is planned
Score peritoneum over vessels, taking mesenteric resection to origin of inferior mesenteric artery
Divide peritoneum with clamps and ties
Divide bowel and create anastomosis by suturing or stapling
Place omentum over anastomosis
Close abdomen in usual fashion without drains
Hallmark Anatomic Complications
Injury to ureters
Injury to superior mesenteric artery (right colon resections)
Injury to duodenum (right colon resections)
Injury to spleen (left colon resections)
List of Structures
Ascending (Right) Colon
Cecum
Ileocecal valve
Hepatic flexure
Transverse colon
Descending (Left) Colon
Splenic flexure
Sigmoid colon
Rectum
White line of Toldt
Celiac artery
Superior Mesenteric Artery
Middle colic artery
Jejunal arteries
Right colic artery
Ileocolic artery
Inferior Mesenteric Artery
Left colic artery
Sigmoid arteries
Superior rectal (hemorrhoidal) artery
Middle rectal (hemorrhoidal) arteries
Marginal artery (of Drummond)
Ileum
Duodenum
Spleen
Gastrocolic omentum
Ureter
Gonadal vessels
Iliac vessels
Genitofemoral nerve
Right Hemicolectomy
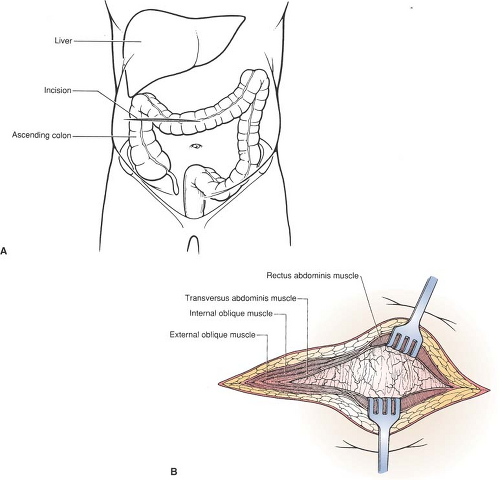
Incision and Exploration of the Abdomen (Fig. 81.1)
Technical Points
The hepatic flexure of the colon is quite close to the cecum, so that a right colon resection can conveniently be performed through a right transverse incision. Consider using this incision in patients who have not had previous subcostal or right lower quadrant incisions (which might compromise the vascularity of the transected rectus muscle). This incision is particularly good for obese patients. Alternatively, a midline or right paramedian incision may be chosen.
Outline a right transverse incision by palpating two landmarks: the costal margin at the anterior axillary line and the anterosuperior iliac spine. Divide the distance between these two points in half and mark it with a pen. Draw a straight transverse line from this point to a point just beyond the midline. Generally, this line will pass above the umbilicus, although occasionally, it will pass below. If it passes straight through the umbilicus, redraw it slightly above. Make the incision through skin and subcutaneous tissue and achieve hemostasis. Divide the muscular and fascial layers of the abdominal wall with electrocautery in a straight line with the skin incision. Enter the abdomen and explore it thoroughly.
A complete and thorough exploration of the abdomen is a necessary preamble to all abdominal surgery cases. In the case of colon cancer, special attention should be paid to possible sites of metastases: the liver, the lymph nodes draining the segment of colon to be resected, the pelvis, the ovaries (in women), and the peritoneal surfaces. Tumor extending beyond the field of resection does not preclude colectomy, but any such metastatic disease should be documented carefully by biopsy. Palpate the entire colon. Second primary lesions are common and may be missed on preoperative screening studies.
Anatomic Points
Transverse incisions were briefly discussed in Chapter 41. The transverse incision recommended here should not divide more than one segmental nerve and, thus, should not result in anesthesia, paresthesia, or paralysis of any part of the anterior abdominal wall, including the rectus abdominis muscle. This incision approximates the direction of the muscle fiber bundles laterally, but is more or less transverse to the direction of rectus abdominis muscle fibers. Often, one of the tendinous inscriptions (usually the lowest) occurs at the level of the umbilicus. The incision should pass either above or below the umbilicus, thereby avoiding cutting through this tendinous inscription because segmental vessels are invariably encountered in the inscriptions and may cause bleeding. If the incision is extended across the midline above the umbilicus, the falciform ligament and ligamentum teres hepatis must be divided. This should be done between clamps, and ligatures should be placed both proximally and distally owing to the paraumbilical veins that accompany the round ligament. These veins can be quite large if the portal system is obstructed and portal blood is shunted to the caval system.
Mobilization of the Colon (Fig. 81.2)
Technical Points
Place a self-retaining retractor, such as a Balfour, in the incision. Elevate the cecum and pull it medially. Incise the
peritoneum lateral to the cecum and pass your nondominant hand behind the colon. Pass the index finger of your nondominant hand laterally to display the peritoneal reflection, thinning it out along the edge of the right colon. Incise it, using scissors or electrocautery, from the cecum to the hepatic flexure. In the region of the hepatic flexure, the peritoneal attachments will become increasingly thick and vascularized. Generally, these can be divided with electrocautery, although some of these vascular adhesions may require clamping and tying or clipping.
peritoneum lateral to the cecum and pass your nondominant hand behind the colon. Pass the index finger of your nondominant hand laterally to display the peritoneal reflection, thinning it out along the edge of the right colon. Incise it, using scissors or electrocautery, from the cecum to the hepatic flexure. In the region of the hepatic flexure, the peritoneal attachments will become increasingly thick and vascularized. Generally, these can be divided with electrocautery, although some of these vascular adhesions may require clamping and tying or clipping.
 |
Sharply divide the filmy adhesions between the colon and retroperitoneum. Elevate the right colon up into the wound from the cecum to the hepatic flexure. As the colon is reflected medially and upward, the terminal ileum will come up as well. Identify the right ureter where it crosses the common iliac vessels just distal to their bifurcation. The colon will come up with minimal
dissection in the avascular retroperitoneal plane. As you proceed up toward the hepatic flexure, search for and identify the duodenum, which is adherent to the transverse mesocolon and frequently will be tented up by traction on the colon. Mobilize the colon off the duodenum with care, sharply incising filmy adhesions and pushing the duodenum down and back into the retroperitoneum. Then place laparotomy pads in the bed of the colon and turn your attention to the region of the hepatic flexure.
dissection in the avascular retroperitoneal plane. As you proceed up toward the hepatic flexure, search for and identify the duodenum, which is adherent to the transverse mesocolon and frequently will be tented up by traction on the colon. Mobilize the colon off the duodenum with care, sharply incising filmy adhesions and pushing the duodenum down and back into the retroperitoneum. Then place laparotomy pads in the bed of the colon and turn your attention to the region of the hepatic flexure.
 |
At the hepatic flexure, one must begin taking the greater omentum with the specimen. The greater omentum connects
the greater curvature of the stomach and the transverse colon.
the greater curvature of the stomach and the transverse colon.
 |
Identify the area of the middle transverse colon that is planned for anastomosis. Preserve the middle colic artery to ensure a good blood supply to the anastomosis. Elevate the transverse colon and palpate the middle colic artery in the mesocolon. Select an area just to the right of the middle colic artery. Divide the omentum from this point up to the greater curvature of the stomach using clamps and ties. Take the greater omentum off the greater curvature of the stomach from this point distally toward the pylorus using clamps and ties. It should then be possible to elevate the entire colon, including the hepatic flexure and middle transverse colon (which will be tethered only by its mesentery).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree