Retroperitoneal Aortic Exposure
Matthew Mell
IMAGING AND OTHER DIAGNOSTIC STUDIES
General Considerations
Retroperitoneal aortic exposure may be desirable for a variety of vascular conditions, including abdominal aortic aneurysms, aortoiliac occlusive disease, and mesenteric or left renal artery occlusive disease.
Retroperitoneal exposure may be preferred for patients with a hostile abdomen from previous intraabdominal infection, surgery, or radiation.
Compared with transabdominal aortic exposure, retroperitoneal exposure may be associated with shorter postoperative ileus, decreased pulmonary complications, decreased pain, and lower incidence of late complications including small bowel obstruction or aortoenteric fistulae.1
Retroperitoneal aortic exposure can be converted, when necessary, to thoracoabdominal exposure with excellent visualization of the superior mesenteric artery (SMA), left renal artery, celiac axis, and descending thoracic aorta.2
Examination of intraabdominal contents is possible through a retroperitoneal approach by simply opening a peritoneal window as necessary.
Preoperative Imaging
Prior to aortic reconstruction, detailed anatomic imaging derived from modern, multirow detector computed tomographic arteriography (CTA) will greatly facilitate surgical planning. Image acquisition should extend from the normal proximal aorta to the common femoral artery bifurcations bilaterally. Runoff imaging may also aid decision making depending on clinical circumstances.
Data derived from submillimeter imaging slices may be readily reformatted into multiplanar and 3-D reconstructions, with excellent resolution of the peripheral mesenteric and renal vasculature.
Noncontrast images should also be obtained to help assess the degree of mural calcification present in diseased proximal aorta. Recognition of extensive mural calcification may modify the location chosen for clamp placement, or prohibit safe clamping entirely in diseased segments.
CTA may require larger contrast dose than that required for catheter-based contrast aortography. Contrast volumes required for CTA may be reduced significantly by modifying the field of view or imaging parameters required for the procedure. Consultation with the responsible radiologist will ensure optimal imaging of the necessary arterial anatomy with minimal contrast and radiation exposure.
Contrast-based aortography, either CT or catheter-based, may be contraindicated for patients with reduced creatinine clearance or an anaphylactic reaction to contrast. Milder allergic responses (hives, rash) may be successfully tempered by premedication with steroids and antihistamines, depending on the relative indication for contrast administration and the patient’s overall medical condition. Adverse effects of intravenous or intraarterial contrast administration on creatinine clearance may be partially ameliorated by preprocedural oral or intravenous hydration and administration of N- acetylcysteine (Mucomyst). Although sometimes considered a reasonable alternative under these circumstances, gadolinium-based contrast administration for magnetic resonance arteriographic indications is also contraindicated in patients with a creatinine clearance less than 60 mL per minute. When contrast administration is absolutely out of the question, CT images acquired without contrast may provide adequate anatomic imaging to proceed with surgery, with the caveat that anomalies such as a retroaortic left renal vein may be present and unrecognized until exposed at surgery.
SURGICAL MANAGEMENT
Instrumentation
In addition to standard vascular instrumentation, additional equipment may aid in exposure of the aorta and its visceral branches from the retroperitoneal approach:
Beanbag and airplane for positioning
A fully articulated operative table, capable of flex and reflex at the level of the umbilicus
Self-retaining, table-mounted retractor (e.g., Bookwalter, Omni, or other)
Finochietto chest retractor
Nos. 3, 4, and 5 Fogarty occlusion balloons
Cold renal perfusion
Arterial cannulas for renal perfusion
Positioning
The patient is placed supine on a beanbag and all lines and tubes are placed. For exposure of the infrarenal aorta and iliac arteries, the left shoulder is lifted and protected with the beanbag and padding. The left arm can be abducted or rotated to the patient’s right with a padded airplane retractor for support. The table break and the kidney bar are used to open up the retroperitoneal space between the 12th rib and the iliac crest as the incision is developed. For this reason, it is essential that the patient be positioned with the umbilicus on the table break. An oblique incision is made from below the umbilicus to the tip of the 11th rib. With this location, the incision can be extended into the 10th intercostal space and the chest entered if additional proximal exposure is required (FIG 1). When additional iliac artery or pelvic exposure is anticipated, the incision should be initiated distal to the umbilicus. Either way, in patients with considerable
abdominal girth and redundant pannus, landmarks should be confirmed to ensure that the incision is not placed too far distally on the abdomen, as juxtarenal aortic control can be extremely difficult when the incision is placed too far distally on the abdomen.
For thoracoabdominal exposure, the patient is placed in the right lateral decubitus position using a beanbag and axillary role for support. The left arm is protected with adequate padding and an airplane-type retractor. It is important to secure the left arm such that the scapula rolls anteriorly, providing exposure of the posterior lateral chest. The incision will be made overlying the 8th intercostal space and extended toward the umbilicus.
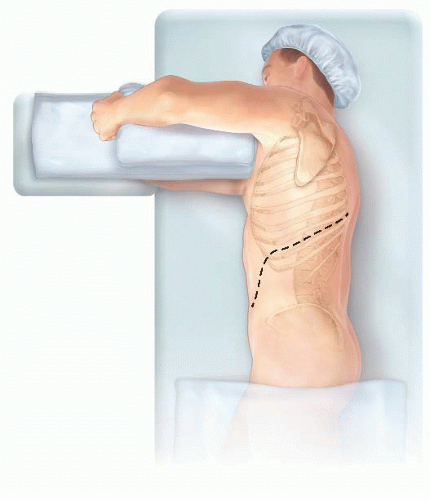 FIG 1 • Patient position for thoracoabdominal exposure with incision in the 8th intercostal space (dotted line). Positioning is supported with a beanbag and right axillary roll. |
TECHNIQUES
The incision is carried through the external oblique, internal oblique, and transversus abdominis muscles. The retroperitoneal space is then entered laterally near the tip of the 11th rib by identifying the characteristic yellow preperitoneal fat. The retroperitoneal space is then developed from lateral to medial using a sponge stick or hands for blunt dissection. Anteriorly, the peritoneum tends to be more adherent at the level of the rectus sheath; care should be taken to avoid entering the peritoneal cavity in this area. The psoas fascia is encountered as the dissection is developed posteriorly in the course of this dissection, which leads directly to the left iliac vessels and ureter. Dissection is continued proximally anterior to the ureter; the ureter is either left in situ to limit injury or gently retracted medially with silastic slings as the retroperitoneal space is developed.
Superiorly, the kidney is identified as the dissection is continued anterior to Gerota’s fascia—a potential space exists between descending colon and Gerota’s fascia in the retroperitoneum, which is progressively developed in a cephalad direction from the psoas muscle, adjacent to the aorta. Once the renal vein is visualized in this space, the superior margin of the dissection is complete. If suprarenal aortic control and exposure is required, this same dissection plane should be developed posterior to the kidney, elevating the kidney and ureters along with the peritoneal contents and retracting all to the right to expose the subdiaphragmatic visceral aorta.
Self-retaining retractor systems are best deployed either after the psoas muscle is identified or following exposure of the renal vein or elevation of the left kidney. Deploying the retractor system earlier will interfere with the dissection necessary to access the appropriate retrocolic space. Following placement of the initial padded retractor blade along the medial margin of the wound, circumferential retraction is secured by placement of additional blades, typically opposite each other to prevent undue tension on the retraction system, with sequential replacement with deeper blades and additional retraction until the entire periaortic retroperitoneum is exposed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


