Restorative Proctocolectomy: Open Technique (Ileal Pouch-Anal Anastomosis)
Hasan T. Kirat
Feza H. Remzi
DEFINITION
Restorative proctocolectomy with ileal pouch-anal anastomosis (RP/IPAA) is defined as removal of entire colon and rectum and construction of an anastomosis of ileal pouch to the anal canal using stapled or hand-sewn technique.
DIFFERENTIAL DIAGNOSIS
When the patients with ulcerative colitis become refractory to medical therapy or steroid dependant, RP/IPAA has been the surgical choice.
RP/IPAA can be performed with good functional results and quality of life, and low pouch failure for indeterminate colitis.
Patients with Crohn’s disease have greater risk of pouch failure following RP/IPAA compared to those with ulcerative colitis.
In patients with familial adenomatous polyposis, the risk of colorectal cancer is eliminated by performing RP/IPAA.
PATIENT HISTORY AND PHYSICAL FINDINGS
A thorough history and physical examination should be obtained.
In inflammatory bowel disease, it is important to note previous and/or concurrent use of steroids, immunomodulators, and nonsteroidal antiinflammatory medications. Patients refractory to these medications are typically candidates for this procedure.
Previous surgeries, particularly in Crohn’s patients, need to be taken into consideration.
Anal and urinary sphincter function needs to be evaluated. Patients with poor anal sphincter function may not be good candidates for RP/IPAA and may need a proctocolectomy with end ileostomy instead.
A full nutritional assessment should be instituted.
Significant cardiac and/or pulmonary comorbidities may prevent the patient to have this procedure.
Family history of colorectal polyps, cancer, and/or inflammatory bowel disease should be elicited.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Preoperative colonoscopy is necessary.
Diagnosis of ulcerative colitis and exclusion Crohn’s disease by colonoscopic biopsy and by an experienced pathologist and/or with the assistance of other laboratory workup, such as Prometheus test, is necessary in order to establish the need for restorative proctocolectomy with ileoanal anastomosis.
Colonoscopic evidence of terminal ileitis by biopsy may assist in the diagnosis of Crohn’s disease.
Diagnosis of ulcerative colitis with proctitis and involvement of the anal canal by colonoscopy or rigid proctoscopy and biopsy may be necessary in order to establish the need for anal mucosectomy and hand-sewn ileal pouch anastomosis.
Contrast-enhanced computed axial tomography (CAT) scan may help evaluate cancer patients for locoregional extent of disease and metastases. CAT scan is also helpful in inflammatory bowel disease to evaluate for acute inflammatory processes (phlegmon, abscess, fistula, or obstruction).
Endorectal ultrasound or rectal protocol magnetic resonance imaging (MRI) may assist with the staging of rectal carcinoma and identification of the anal sphincter muscle involvement. The latter would be a contraindication of a restorative proctocolectomy. It may also delineate the anatomy of the anal sphincter in case of previous obstetric trauma or episiotomies.
Obtaining a Wexner fecal incontinence score preoperatively may assist with the diagnosis of fecal incontinence. Manometry studies may also be helpful in these patients. Preoperative fecal incontinence may lead to poor functional outcome following an ileoanal pouch anastomosis.
Preoperative barium enema or small bowel follow-through contrast study may assist with the diagnosis of Crohn’s disease.
SURGICAL MANAGEMENT
Preoperative Planning
The site for a diverting loop ileostomy is marked before surgery.
A complete bowel preparation is recommended.
Prophylaxis against deep venous thrombosis and prophylactic perioperative antibiotics should be administered.
The rectum is washed out with normal saline in the operating room.
Positioning
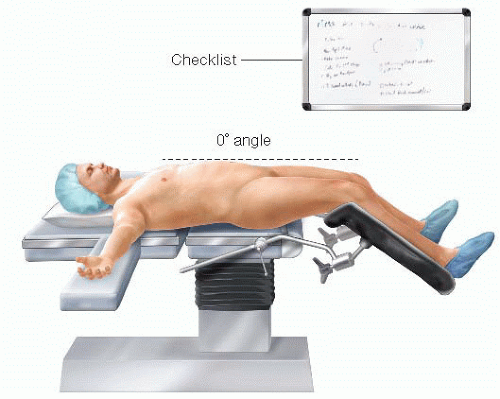
The procedure is performed with the patient in a Lloyd-Davies position (FIG 1).
This position is defined as Trendelenburg position with legs apart.
The thighs are level with the abdomen as this allows efficient placement of a self-retaining retractor without creating excessive pressure between the retractor and the patient’s thighs.
All pressure points are padded to avoid potential neurovascular injuries.
The perineum is positioned flush with the edge of the operating room table for easy access during the perineal phase of the operation.
The pelvis is supported with a folded sheet to lift the entire perineum and facilitate exposure during the perineal dissection.
The arms are placed in a neutral position and supported with suitable armrests or tucked to the side.
TECHNIQUES
PLACEMENT OF INCISION
A midline vertical incision is made.
A suitable laparotomy retractor is inserted.
After general inspection to see if there are any contraindications to performing RP/IPAA, the small bowel is packed with moist large swab packs into the upper abdominal cavity.
MOBILIZATION OF THE RIGHT COLON: PRESERVATION OF THE ILEOCOLIC VASCULAR PEDICLE
The surgeon stands to the patient’s left side. The patient is placed on a Trendelenburg position with the right side up to facilitate exposure.
A full Cattell-Braasch maneuver is performed to mobilize the right colon of its retroperitoneal attachments.
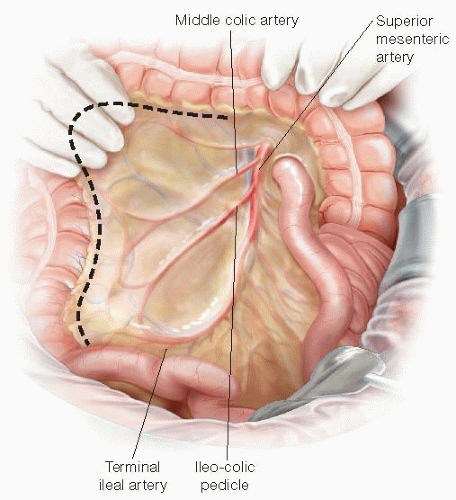
The cecum and ascending colon are freed from the peritoneal reflection by incising along the white line of Toldt (FIG 2). The terminal ileum is also freed from the retroperitoneum and mobilized by incising the peritoneum along the root of the mesentery.
As the colon and terminal ileum are reflected anteriorly and medially, the right gonadal vessels and right ureter should be identified in the retroperitoneum and not mobilized anteriorly so as to avoid injury.
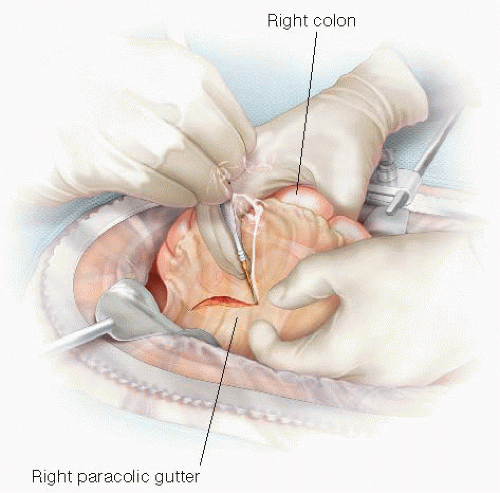
FIG 2 • Ascending colon mobilization. The surgeon retracts the ascending colon medially. Dissection proceeds along the right paracolic gutter.
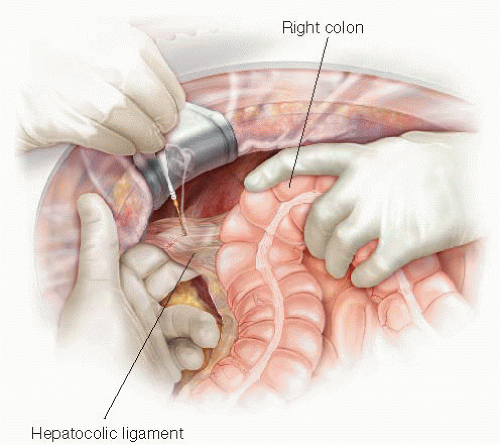
FIG 3 • Hepatic flexure mobilization. Gentle traction on the hepatic flexure of the colon exposes the hepatocolic ligament, which is then transected with electrocautery.
The lateral dissection is carried sharply up and around the hepatic flexure in the avascular, embryologic plane between the mesocolon and the duodenum. The second and third portions of the duodenum are identified near the hepatic flexure and injury to this structure must be avoided.
The hepatocolic ligament is transected (FIG 3).
Using an energy device, we hemostatically divide the ascending colon mesentery between the mesenteric vascular arcade and the colon wall (FIG 4) while protecting at all times the ileocolic vascular pedicle up to the mesenteric level of the ileocecal valve. This will allow excellent prograde blood supply to the pouch later on. Avoiding an ileocolic mesenteric bleeding or hematoma is crucial for preservation of the vascular supply to the ileal J-pouch.
The mesenteric division extends from the midtransverse colon down to the mesenteric border of the terminal ileum at the selected site of proximal intestinal division— just proximal to the ileocecal valve.
TRANSVERSE COLON MOBILIZATION
The gastrocolic ligament is exposed as the assistant retracts the greater omentum superiorly while the surgeon retracts the transverse colon anteroinferiorly.
Diathermy is used to separate the greater omentum from the anterior leaf of the transverse mesocolon.
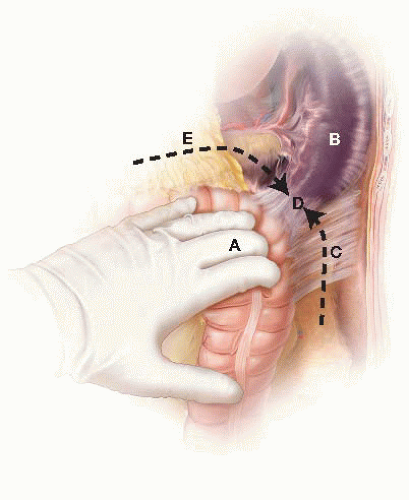
Mobilization of the spleen needs to be approached from both sides to facilitate ease of mobilization of the splenic flexure (FIG 5). The patient is placed on a reverse Trendelenburg position with the left side up to allow the spleen to come down into the surgical field.
Once the gastrocolic ligament has been completely transected, transection of the lateral peritoneal attachments (phrenocolic ligament) allows for lateral mobilization of the splenic flexure.
At this point and from the right side of the table, the surgeon hooks the splenocolic ligament anteriorly with his or her right index finger, exposing the ligament adequately for the assistant to transect it using electrocautery. The splenocolic ligament is divided as close to the colon as feasible, avoiding undue traction on the spleen.
DESCENDING COLON MOBILIZATION
The surgeon stays on the right side of the table. The patient is placed on Trendelenburg position with the left side up.
The descending colon is mobilized by medial traction and dissection along the left paracolic gutter using diathermy.
The colon is mobilized from the retroperitoneum using a lateral to medial approach.
Care is taken to identify, and avoid damage to, the left gonadal vessels and left ureter (FIG 6). In the lower abdomen, the left ureter is located medial to the gonadal vessels, close to the midline.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree