Reoperative Parathyroidectomy
Barnard J. A. Palmer
William B. Inabnet III
DEFINITIONS
Reoperative parathyroid surgery occurs in multiple clinical settings but is most frequently performed as the result of failed exploration, recurrent, or persistent hyperparathyroidism.
Persistent hyperparathyroidism is defined as hypercalcemia that remains or recurs within 6 months of an initial parathyroid operation.
Recurrent hyperparathyroidism is the reappearance of hypercalcemia after a period of 6 months of postoperative normocalcemia following successful surgery.
PATIENT HISTORY AND PHYSICAL FINDINGS
A detailed history of the patient’s disease should be performed, focusing on the management to date.
Biochemical confirmation of persistent or recurrent hyperparathyroidism is the initial step in management. A 24-hour collection for calcium is recommended.1,2
The benefits of reoperation must be weighed against the risks of continued hyperparathyroidism and the surgical complications for each individual patient. Nonsurgical management can be considered if the sequela of continued parathyroid disease is relatively low risk or the risk of operation is high.
Surgical history is an essential component of reoperative parathyroid surgery. The surgeon must understand reasons for initial operative failure.3
Operative and pathology reports should be carefully reviewed, focusing on the extent of exploration, glands identified and removed, whether confirmed by biopsy, if marked, and if reimplanted.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Extensive preoperative planning is key to successful reoperative surgery.
Previous operative reports, imaging, and pathology results should be obtained and reviewed to understand the cause of failure.2
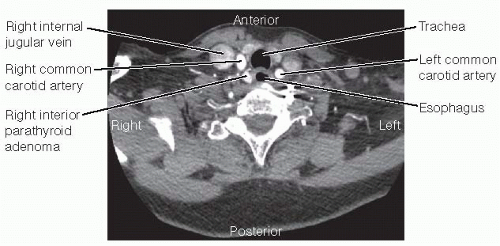
Localization studies are an essential portion of preoperative planning and should be performed in all reoperative parathyroid patients. Ultrasound, sestamibi, computed tomography (CT) (parathyroid protocol, 4-D) (FIG 1), single-photon emission computed tomography-computed tomography (SPECT/CT), and fluorodeoxyglucose-positron emission tomography (FDG-PET) can be used for localization and to rule out multigland disease. Preoperative location of abnormal glands can significantly alter the operative approach particularly if aberrant glands lie in the mediastinum.
Fine needle aspiration (FNA) with measurement of parathyroid hormone (PTH) can confirm parathyroid tissue in questionable lesions or parathyroid adenomatosis identified by ultrasound.
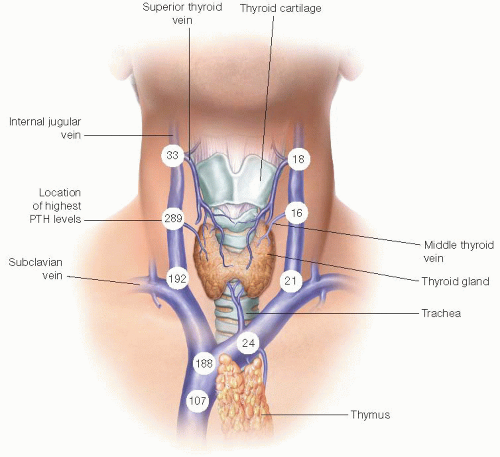
Invasive localization studies such as selective venous sampling (FIG 2) or arteriography should be reserved for when noninvasive studies fail to localize pathology.
SURGICAL MANAGEMENT
Preoperative Planning
The imaging must be thoroughly reviewed to plan the operative approach.
Prior operative notes are reviewed and operative steps clearly determined prior to reexploration.
Positively localized lesions lend themselves to focused reexplorations, whereas more extensive exploration is required for multigland or nonlocalized diseases.
Preoperative flexible laryngoscopy is recommended prior to reoperative surgery to document vocal cord function and guide the extent of surgery.
Frozen section and intraoperative PTH assays are useful adjuncts to confirm parathyroid identification and biochemical cure.
Positioning
The patient is positioned either supine or in the semi-Fowler position. Both arms are tucked and neck extension is achieved with a shoulder roll (FIG 3).
Surgical prep must be wide enough to allow access superiorly to angle of mandible and inferiorly to xiphoid in the instance that sternotomy is necessary.
General endotracheal anesthesia permits the use of intraoperative nerve monitoring.
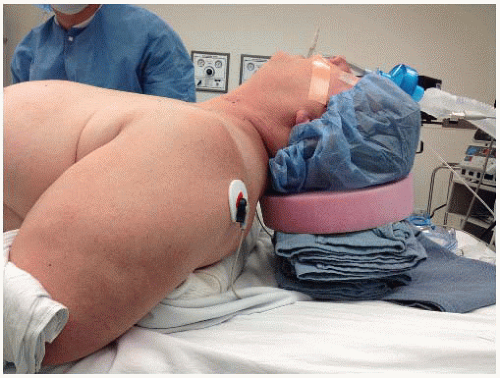 FIG 3 • The patient is placed supine with both arms tucked. A shoulder roll provides additional neck extension, which elevates the trachea anteriorly and superior mediastinal structures cephalad. |
TECHNIQUES
CERVICAL REEXPLORATION
Incision and Flap Elevation
Skin incisions are placed as indicated by the preoperative localizing studies, preferably in a natural cervical skin crease or the old incision (unless the scar is too low or high). Width of incision is dependent on depth of neck but is large enough to allow access superiorly to the level of the hyoid bone and inferiorly to the anterior mediastinum (FIG 4).
Incisions may be placed over the site of pathology for a directed approach if preoperatively localized.
Skin and platysma are divided and subplatysmal flaps superficial to the anterior jugular veins are elevated superiorly to the thyroid notch, inferiorly to the sternal notch, and laterally to anterior borders of the sternocleidomastoid muscles (SCM).
Cervical Approach3
Surgical approach to the reoperative neck is done via focused exploration or by classic midline, posterolateral, or thyrothymic ligament approaches.
Focused explorations for preoperatively localized ectopic glands not accessible via prior cervicotomy should be adjusted to location and surgeon experience with incisions placed according to imaging.
Revision cervicotomy is indicated when multigland disease is suspected or when abnormal glands are not localized preoperatively. The previous incision is used and the cervical scar revised prior to opening the midline raphe by vertical separation of strap muscles (see Part 5, Chapters 45 and 48).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree