Renal Medullary Carcinoma
Satish K. Tickoo, MD
Victor E. Reuter, MD
Key Facts
Terminology
Distinctive clinicopathologic entity in patients with sickle cell hemoglobinopathies
Etiology/Pathogenesis
Presence of HbS in virtually all cases suggesting some cause-effect relationship between hemoglobinopathy and this tumor
Loss of immunohistochemical nuclear expression of INI1 (SNF5) protein, similar to pediatric rhabdoid tumor of kidney, is consistent finding
Clinical Issues
Usually male and African-American
Medullary region of kidney
Patients with sickle cell trait (Hb-AS), Hb-SC, and rarely Hb-SS
Very aggressive tumor with metastases at presentation in almost all, and mean survival of 4 months
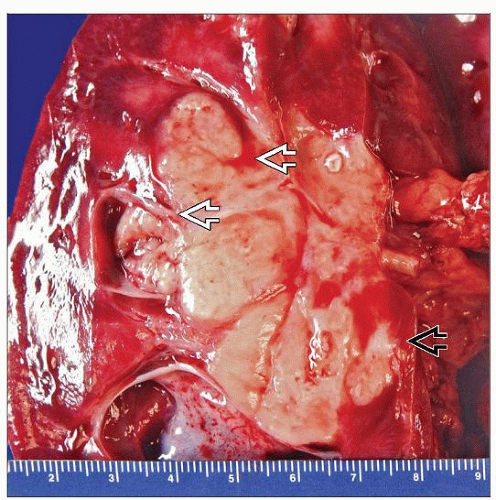
Macroscopic Features
Gray-white, possessing infiltrative borders and extending into perihilar fat
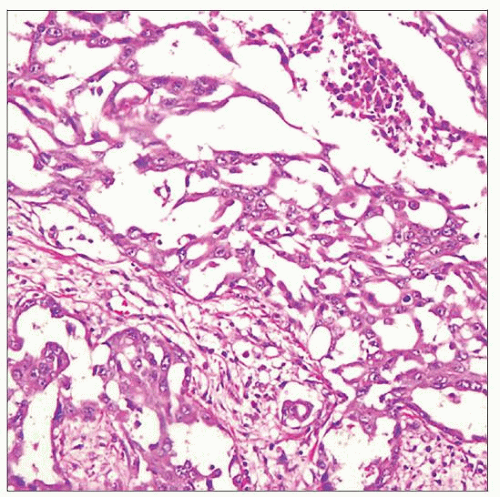
Microscopic Pathology
Reticular, cribriform, solid, tubular, or adenoid cystic-like growth patterns
Marked desmoplastic stroma and intratumoral inflammatory infiltrate, usually neutrophilic
Sickled RBCs frequently observed, both within tumor and surrounding parenchymal vessels
Top Differential Diagnoses
Collecting duct carcinoma
Urothelial carcinoma
TERMINOLOGY
Abbreviations
Renal medullary carcinoma (RMC)
Synonyms
Medullary renal cell carcinoma (RCC)
Definitions
Distinctive clinicopathologic entity occurring almost exclusively in patients with sickle cell trait
Rare cases in patients with hemoglobin SC disease and very occasionally in sickle cell disease (SS)
ETIOLOGY/PATHOGENESIS
Sickle Cell Hemoglobinopathies
Presence of HbS in virtually all cases, suggesting some cause-effect relationship between hemoglobinopathy and this tumor
Exact mechanism unknown; role of tissue hypoxia and hypoxia-inducible factor (HIF) in tumorigenesis or tumor viability/tumor progression is suggested
INI1(hSNF5/BAF47)
Loss of immunohistochemical nuclear expression of SNF5 (INI1) protein, similar to pediatric rhabdoid tumor of kidney, is consistent finding
Molecular mechanism, i.e., mutations/loss of gene or others, for this absent SNF5 expression is not known
ABL-BCR Amplifications
Amplification of both ABL and BCR genes described in few cases
ABL-BCR translocation described in 1 case but not in 3 others tested
Relationship to Collecting Duct Carcinoma
Some consider RMC to be a particularly aggressive form of collecting duct carcinoma
CLINICAL ISSUES
Epidemiology
Incidence
Very uncommon tumor
Age
Range: 5-39 years; only occasionally in older patients
Gender
Predominantly male, especially in patients < 25 years old
Ethnicity
Mostly African-American; occasionally of Mediterranean ancestry, rarely others
Presentation
Often with hematuria or flank pain, and many presenting with symptoms related to metastases
Laboratory Tests
Most with sickle cell trait (Hb-AS) or Hb-SC on hemoglobin electrophoresis
Rarely with homozygous sickle cell anemia (Hb-SS)
Prognosis
Biologic behavior very aggressive; mean survival approximately 4 months; most cases with metastases at presentation
MACROSCOPIC FEATURES
MICROSCOPIC PATHOLOGY
Histologic Features
Most common architectural features: Reticular or cribriform glands
Other patterns include yolk sac-like, glandular, solid nests, and tubules; undifferentiated sheet-like or adenoid cystic-like
Stroma almost always fibrotic or desmoplastic, and intratumoral inflammatory infiltrate, mostly neutrophils, is very frequent
Tumor margins always infiltrative
Cytoplasmic mucin is commonly observed
Cytology usually high grade, with moderate to marked nuclear atypia
Occasional cases with rhabdoid features
Sickled RBCs frequently observed, both within tumor and surrounding renal parenchymal vessels
Often with high pT and pN stage and satellite tumor nodules due to very frequent vascular spread
Predominant Pattern/Injury Type
Neoplastic
Predominant Cell/Compartment Type
Epithelial
DIFFERENTIAL DIAGNOSIS
Collecting Duct Carcinoma
Medullary carcinoma believed by some to be particularly virulent variant of collecting duct carcinoma
No hemoglobinopathy
Usually HMCK(34βE12) positive
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree