Radical Hysterectomy
Young Bae Kim
Introduction
Radical hysterectomy and bilateral pelvic lymphadenectomy is the standard operation for early cervical cancer. Wertheim developed the modern technique for radical hysterectomy in the early 20th century, and in the 1940s Meigs added routine pelvic lymphadenectomy to the procedure, thereby increasing its curative potential. Initially described as a very morbid operation, radical hysterectomy can now be performed with an acceptably low rate of serious complications. Advances in modern surgical technique, as well as those in anesthesia, transfusion, and antibiotics, now allow the operation to be performed with a rate of serious morbidity approaching 1%. As a result, radical hysterectomy and bilateral pelvic lymphadenectomy is a viable alternative to radiation for the definitive treatment of some patients with FIGO stage Ia, Ib, and IIa cervical cancer.
A randomized study has shown that radical hysterectomy and radiation both result in 5-year survival rates of 85% in early cervical cancer. Therefore, the choice of treatment for a given patient rests with other considerations. Radical surgery has a number of potential advantages over radiation. It allows preservation of ovarian function. It also allows better preservation of sexual function relative to radiation. It is associated with fewer long-term complications than radiation, particularly with respect to chronic diarrhea, tenesmus, and urinary tract and bowel fistulas. Radical hysterectomy does have the disadvantage that it is not as widely applicable as radiation. Poor surgical candidates, such as those who are medically compromised or morbidly obese, may be better served with radiation. Radical hysterectomy is also associated with more acute complications compared to radiation, such as infection, thromboembolism, and ureteral injury.
Radical hysterectomy differs from simple (or total) hysterectomy in that the tissues surrounding the cervix are removed along with the uterus and cervix. This includes the cardinal ligaments, uterosacral ligaments, and upper vagina. While these tissues do not appear very impressive in the final specimen, the additional work necessary to remove them is considerable. During the operation, more time is spent in mobilizing the surrounding organs, namely the bladder, ureters, and rectum, than in removing the specimen. In addition, pelvic lymphadenectomy, while not strictly speaking a part of radical hysterectomy, is almost always performed in conjunction with radical hysterectomy when treating cervical cancer. The final result of radical hysterectomy and pelvic lymphadenectomy is a classic Halstedian operation, with radical resection of the primary tumor and resection of the draining lymph nodes.
Early cervical cancer is by the far the most common indication for radical hysterectomy and pelvic lymphadenectomy. However, a number of other indications exist for which this operation is suited. These include stage I vaginal cancers limited to the upper vagina and stage II endometrial cancers with gross cervical involvement. Somewhat more controversial
is the use of radical hysterectomy for small, centrally recurrent cervical cancers occurring after previous treatment with radiation. Many surgeons feel that these patients have a better chance of long-term survival with pelvic exenteration.
is the use of radical hysterectomy for small, centrally recurrent cervical cancers occurring after previous treatment with radiation. Many surgeons feel that these patients have a better chance of long-term survival with pelvic exenteration.
There has been a long-term trend toward decreasing the radicality of radical hysterectomy in the hopes of decreasing morbidity while at the same time preserving curative potential. The most important example of this is the adoption of the Wertheim method over more radical operations. Going a step further, many surgeons now routinely perform an even less radical procedure, termed modified radical hysterectomy. A randomized clinical trial demonstrated that modified radical hysterectomy is associated with less morbidity and similar rates of cure in patients with stage Ib and IIa cervical cancer. One limitation of this study was the high rate of adjuvant radiation, which may have negated the effects of any differences in surgical technique between the treatment arms. Nevertheless, many surgeons advocate modified radical hysterectomy for patients with smaller tumors (<1 to 2 cm). The purpose of this chapter is to describe both radical hysterectomy and modified radical hysterectomy in detail, highlighting important points that allow these inherently difficult operations to be performed with success. Other recent developments include a resurgence of interest in vaginal approaches to radical hysterectomy, the incorporation of laparoscopy, and radical trachelectomy. These procedures are beyond the scope of this chapter, but they do offer the possibility of minimally invasive treatment and sparing of fertility without compromising the chance for cure.
Although radical hysterectomy is intended to be definitive treatment for early cervical cancer, some patients are at significant risk for recurrence with surgery alone and benefit from adjuvant therapy. Patients with positive pelvic lymph nodes, parametrial involvement, and positive surgical margins should be offered pelvic radiation with concurrent platinum-based chemotherapy. Adjuvant therapy may also be considered for other high-risk patients such as those with large tumors, deep stromal invasion, or lymphovascular space invasion, although the data supporting treatment of these patients are not as strong. The management of patients with large (stage Ib2) cervical tumors is controversial, with some surgeons favoring a primary surgical approach with or without adjuvant chemoradiation and others favoring chemoradiation alone. This question is currently being addressed by a randomized clinical trial.
Initial Steps
General anesthesia is induced. A single dose of antibiotic administered before incision is usually sufficient for prophylaxis, although a repeat dose may be given if the operation exceeds 4 hours. Pneumatic compression stockings, minidose heparin, or both may be used for thromboembolism prophylaxis.
The patient is placed in dorsal supine or low lithotomy position. Examination under anesthesia is performed to exclude the presence of disease beyond the cervix and upper vagina. Rectal examination is particularly important in order to exclude disease extension into the cardinal ligaments. Cystoscopy and proctosigmoidoscopy may also be performed at the discretion of the surgeon to exclude disease extension into the bladder or rectum. Any findings suspicious for disease extension beyond the cervix and upper vagina should prompt abandonment of the operation in favor of radiation.
A Foley catheter is placed (some surgeons favor a suprapubic catheter). A vertical midline or low transverse incision may be used. Two transverse incisions, the Maylard and Cherney, provide excellent pelvic exposure. A vertical incision is preferable when the surgeon plans to sample the para-aortic lymph nodes. Once inside the peritoneal cavity, the abdomen and pelvis are thoroughly explored manually and visually. Any evidence of metastatic disease should prompt abandonment of the procedure if confirmed histologically. Particular attention is paid to the area around the cervix, including the posterior cervix and cul-de-sac. A formal para-aortic lymph node sampling, while favored by some surgeons, is associated with low yield and is therefore not standard. Peritoneal washings are sometimes performed, but the significance of positive washings in this setting remains unclear.
Radical Hysterectomy
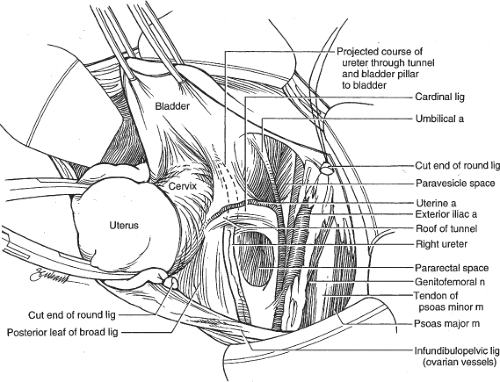
A Buchwalter or similar self-retaining retractor may be placed to expose the pelvis. Femoral neuropathy is a risk of using such retractors, but this risk can almost be eliminated by ensuring that there is room between the bottoms of the blades and the psoas muscles. The bowel is displaced cephalad using moist laparotomy packs. The uterus is grasped with a triple hook or Kelly clamps and placed on cephalad tension. The round ligaments are suture-ligated and divided. Absorbable suture, commonly 0 Vicryl, is used throughout the operation. The broad ligaments are opened in a cephalad and caudad direction lateral to the gonadal vessels, and the ureters are identified along the medial leaves of the broad
ligament (Fig. 1). They are most readily identified as they enter the true pelvis and cross over the bifurcation of the common iliac arteries.
ligament (Fig. 1). They are most readily identified as they enter the true pelvis and cross over the bifurcation of the common iliac arteries.
The pararectal and paravesical spaces are then developed. These are avascular potential spaces that allow the peritoneum over the pelvic sidewall to be mobilized safely, thus exposing the pelvic sidewall vessels and the course of the ureters. The pararectal space is bounded by the external and internal iliac vessels laterally, the ureter medially, and the cardinal ligament anteriorly. Using either a single finger or a dissecting instrument, the common iliac artery bifurcation is identified and the space just medial to this is opened, resulting in displacement of the ureter medially. Care is taken to ensure that the dissection remains medial to the internal iliac artery. The dissection follows the hollow of the sacrum caudad and curves slightly medially toward the rectum. The space may be opened to the level of the levator plate.
The paravesical space is bounded by the external iliac vessels laterally, the bladder and superior vesical artery medially, and the cardinal ligament posteriorly. Again using either a finger or a dissecting instrument, the space just medial to the most distal aspect of the external iliac vein is developed, displacing the bladder medially. The space is followed medially and caudad along the pubic symphysis toward the levator plate. Once the space is open, the superior vesical artery is readily apparent as it enters the lateral dome of the bladder. Care must be taken to avoid bleeding in the prevesical space just medial to the paravesical space.
Now the surgeon must make the final assessments for resectability prior to completing the planned operation. The vesicouterine fold of peritoneum is incised and the bladder is dissected down the anterior cervix and upper vagina in an avascular plane. This is best accomplished with sharp dissection or electrocautery to minimize bleeding and trauma to the bladder. Any tumor extension through the anterior cervix will be evident at this point. Such a finding indicates unresectability. The cardinal ligaments are then palpated with two fingers, one in the paravesical space and one in the pararectal space. This “web” of tissue comprises the condensation of fibrovascular tissue lateral to the cervix constituting the cardinal ligament (the term parametrium is often used synonymously). Any palpable disease in the cardinal ligaments also indicates unresectability. Finally, the pelvic lymph nodes are assessed, and any grossly suspicious nodes are sent for frozen section. Most surgeons abandon the radical hysterectomy if grossly positive lymph nodes are encountered. There is some evidence that debulking such nodes prior to closing improves the chances for cure.
Some surgeons now proceed with pelvic lymphadenectomy, the rationale being that the finding of microscopically positive pelvic lymph nodes would result in abandonment of the operation. However, the yield is low if the nodes are grossly normal, and the technique of intraoperative frozen section is inaccurate and cumbersome. Furthermore, many surgeons would complete the radical hysterectomy with microscopically positive pelvic nodes and recommend adjuvant chemoradiation afterwards. This approach may allow for improved sexual function compared with radiation alone, as the latter necessarily includes a very high dose of vaginal brachytherapy. We generally perform the pelvic lymphadenectomy after radical hysterectomy.
The cardinal ligament is dissected down to the uterine artery, which is then ligated at its origin from the internal iliac artery (Fig. 2). The uterine artery is reflected above the ureter. The ureteral dissection, the most critical part of the operation, then commences. The ureter is dissected off the peritoneum near the uterosacral ligament, taking care to preserve its surrounding adventitial blood supply. A small wavy vessel is often seen adjacent to the ureter and should be preserved. The ureter is then freed of its peritoneal attachments. This is facilitated by cephalad traction on the uterus and posterior traction on the ureter’s adventitia. The ureter should not be handled directly. The “tunnel,” through which the ureter courses lateral and anterior to the cervix, is then dissected, freeing the ureter (Fig. 2). It is crucial that the dissecting instrument remain in close proximity to the ureter in order to avoid significant bleeding that can ensue and obscure the field. The instrument is best placed just superolateral to the ureter. Once a pedicle is established, it may be ligated directly or after transection between clamps. The latter method is facilitated by specialized clamps developed by Casey.
The last part of the tunnel is composed of the bladder pillars, which are fibrovascular attachments of the bladder to the lateral aspects of the cervix. The pillars are exposed initially with the bladder dissection. Further anterior dissection of the pillars can facilitate the ureteral dissection, but care must be taken to avoid injuring the numerous small vessels within. The ureteral dissection is completed to the insertion into the bladder (Fig. 3). The surgeon must be careful to end the tunnel dissection once the bladder is reached, as the ureterovesical junction is not always obvious. The ureter, having been unroofed from its tunnel, is now dissected out of its cardinal ligament bed completely.
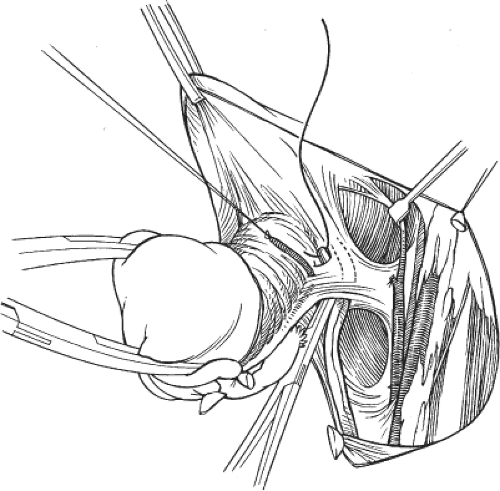
If the adnexa are to be removed, the gonadal vessels are now isolated above the ureters and ligated. If the adnexa are to be conserved, the utero-ovarian pedicles are isolated and ligated. The posterior dissection
then commences (Fig. 4). The rectovaginal fold of peritoneum is incised, taking care to avoid the ureters. The incision crosses both uterosacral ligaments and the upper cul-de-sac. The rectum is dissected down the posterior vagina in an avascular plane. This can often be accomplished with gentle blunt dissection, with care taken to avoid direct pressure on the rectum. Excessive force can result in unintentional entry into the posterior vaginal wall, which is quite thin. The uterosacral ligaments are cleared of the rectum. Some bleeding from the rectal pillars may ensue, but this is generally not problematic.
then commences (Fig. 4). The rectovaginal fold of peritoneum is incised, taking care to avoid the ureters. The incision crosses both uterosacral ligaments and the upper cul-de-sac. The rectum is dissected down the posterior vagina in an avascular plane. This can often be accomplished with gentle blunt dissection, with care taken to avoid direct pressure on the rectum. Excessive force can result in unintentional entry into the posterior vaginal wall, which is quite thin. The uterosacral ligaments are cleared of the rectum. Some bleeding from the rectal pillars may ensue, but this is generally not problematic.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree