Pyogenic Abscess
Joseph Misdraji, MD
Key Facts
Etiology/Pathogenesis
Most commonly isolated organisms are Escherichia coli, Klebsiella pneumonia, Enterococcus spp., Streptococcus spp., and Pseudomonas spp.
Anaerobes are isolated in up to 25% of cases
Fungi, such as Candida and Aspergillus, are found in 15% of cases
At least 1/3 of cases are polymicrobial
Clinical Issues
Major causes include biliary disease and intraabdominal infection
Risk factors: Diabetes mellitus, malignancy, alcohol abuse, cirrhosis, hypertension, recent surgery, and immunosuppression
Percutaneous drainage and antibiotics are mainstay of therapy
Main risk factors for metastatic infection are diabetes mellitus and infection with K. pneumonia
Mortality ranges from 5-31%
Macroscopic Features
Most abscesses are solitary; multiple abscesses occur in 25-45% of cases
Right lobe most frequent site
Microscopic Pathology
Abundant neutrophils, fibrin, and bile
Aerobic and anaerobic culture of abscess contents and histochemical stains for organisms are required to determine cause
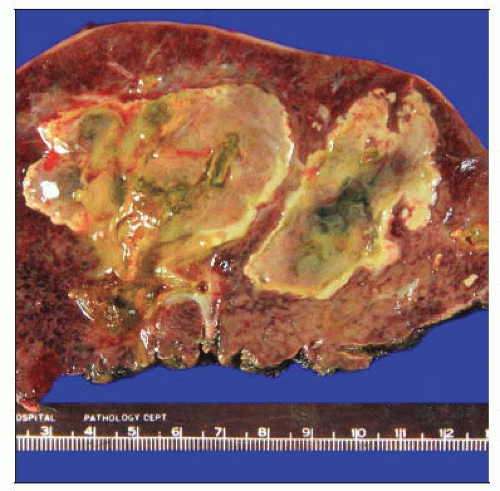 Gross photograph of a hepatectomy specimen shows large, irregular, yellow-tan soft abscesses with central green bile-stained necrosis. |
TERMINOLOGY
Definitions
Localized accumulation of pus in liver with surrounding inflammation
ETIOLOGY/PATHOGENESIS
Infectious Agents
Most commonly isolated organisms: Escherichia coli, Klebsiella pneumonia, Enterococcus spp., Streptococcus spp., and Pseudomonas spp.
Organisms that produce formic hydrogenylase (Klebsiella spp. and E. coli) can convert acids in abscess into carbon dioxide and hydrogen gas
Gas-forming pyogenic abscess carries higher risk of septic shock, bacteremia, and death
Anaerobes are isolated in up to 25% of cases
Most commonly microaerophilic Streptococci, Bacteroides fragilis, Fusobacterium necrophorum, and Clostridia spp.
Actinomyces spp. can be associated with formation of sinus tracts
Rare isolates include Francisella tularensis, Burkholderia pseudomallei (cause of melioidosis), Brucella spp. (particularly B. suis), and Listeria monocytogenes
Fungi, such as Candida and Aspergillus, are found in 15% of cases
At least 1/3 of cases are polymicrobial
Predisposing Conditions
Historically associated with acute appendicitis or intraabdominal infection, particularly in children
Biliary disease has emerged as most common etiology
CLINICAL ISSUES
Epidemiology
Age
55-60 years old
Gender
Males affected more often than females
Site
Most abscesses occur in right lobe (70%); left lobe or bilateral disease is less common
Presentation
Symptoms include fever, chills, right upper quadrant pain, and elevated alkaline phosphatase