Pulmonary BALT Lymphoma
Key Facts
Clinical Issues
Most common presentation is solitary mass on routine imaging studies
Most patients are asymptomatic
Favorable prognosis; 5-year survival in approximately 85-95%
Image Findings
May present as single, solitary nodule or as diffuse bilateral disease mimicking diffuse interstitial pneumonia
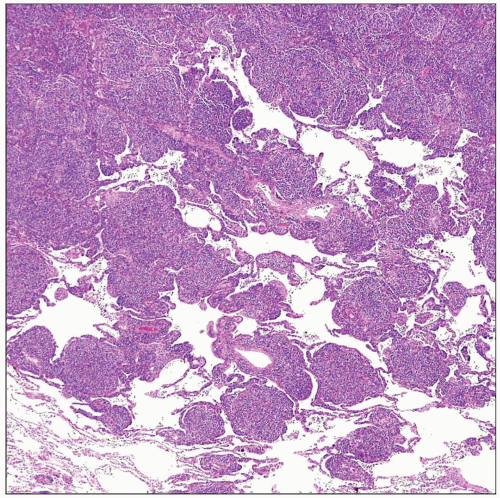
Microscopic Pathology
Diffuse lymphoid infiltrates composed of small lymphocytes admixed with reactive lymphoid follicles
Reactive lymphoid follicles may show extensive infiltration by marginal zone lymphocytes (follicular colonization)
Infiltration of underlying epithelial structures forming “lymphoepithelial” lesions is characteristic
Cytomorphology of neoplastic small lymphocytes is variable and includes centrocytic cells, plasmacytoid cells, and monocytoid cells
Ancillary Tests
Neoplastic cells are positive for CD19, CD20, CD79a, and Bcl-2
Tumor cells are negative for CD5, CD10, CD23, Bcl-1, and Bcl-6
t(11;18)(q21;q21) is most common genetic abnormality (encountered in about 50% of cases)
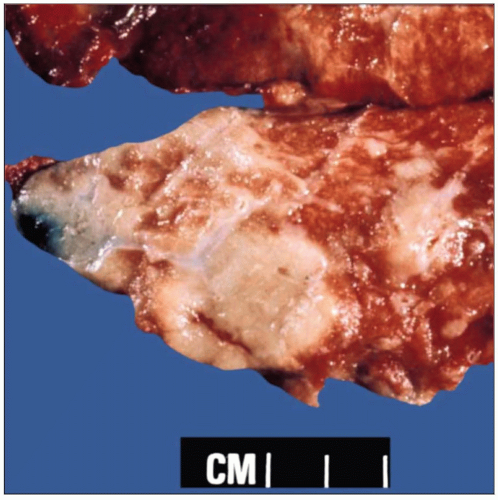 Gross appearance of BALT lymphoma of the lung shows nodular, ill-defined, coalescent areas of lung parenchyma replaced by tan-white, homogeneous, rubbery tissue. |
TERMINOLOGY
Synonyms
Marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT) type
Definitions
Monoclonal proliferation of small lymphocytes arising from marginal zone of B-cell follicles
ETIOLOGY/PATHOGENESIS
Etiology
Thought to arise secondary to inflammatory and autoimmune processes
CLINICAL ISSUES
Epidemiology
Incidence
Accounts for approximately 80% of primary lung lymphomas
Accounts for < 0.5% of all primary lung neoplasms
Age
Most common from 50-70 years of age
Can occur in younger patients with underlying immunosuppression
Presentation
Most common presentation is solitary mass on routine imaging studies
May be localized or diffuse
Most patients are asymptomatic
Some patients may present with symptoms of cough, dyspnea, and chest pain
Treatment
Surgical approaches
Surgical excision achieves excellent results in localized, resectable tumors
Adjuvant therapy
Indicated in patients with diffuse or bilateral involvement
Other options
Elderly patients with asymptomatic lesions may be clinically followed without therapy
Prognosis
Favorable prognosis; 5-year survival in approximately 85-95%
Small proportion of cases may progress to diffuse large B-cell lymphoma
IMAGE FINDINGS
General Features
Location
Tumors are typically peripheral in location
Morphology
May present as single, solitary nodule or as diffuse bilateral disease mimicking diffuse interstitial pneumonia
CT Findings
High-resolution computerized tomographs (HRCT) show multiple solitary masses or alveolar opacities
HRCT may also show airway dilatation, positive angiogram signs, and ground-glass shadowing at margins
MACROSCOPIC FEATURES
Cut Surface
Tan-white, fleshy, homogeneous rubbery tissue
Involved area of lung parenchyma can be nodular and well circumscribed or diffuse
MICROSCOPIC PATHOLOGY
Histologic Features
Diffuse lymphoid infiltrates composed of small lymphocytes admixed with reactive lymphoid follicles
Reactive lymphoid follicles may show extensive infiltration by marginal zone lymphocytes (follicular colonization)
Infiltration of underlying epithelial structures forming “lymphoepithelial” lesions is characteristic
Scattered larger, immunoblastic cells may be seen admixed with small lymphoid cell infiltrate
Lymphangitic distribution characteristically observed at edges of lesions
Stromal hyalinization and fibrosis may be seen in advanced lesions
Cytologic Features
Cytomorphology of neoplastic small lymphocytes is variable and includes
Small lymphocytes with minimal nuclear irregularities resembling germinal center centrocytes
Plasmacytoid small lymphocytes
“Monocytoid” B-lymphocytes showing clear perinuclear hues and ample cytoplasm
ANCILLARY TESTS
Immunohistochemistry
Neoplastic cells are positive for CD19, CD20, CD79a, Bcl-2, and Bcl-10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree