Proximal to the Wrist: Upper Extremity Reconstruction/Revascularization
Mohamed A. Zayed
Ronald L. Dalman
DEFINITION
The content discussed in the following text assumes the reader has familiarity with standard upper extremity arterial anatomy and its most common variations. For additional information, the reader may refer to excellent existing references.1,2
Various occlusive and/or aneurysmal disease processes in the upper extremity arterial system may necessitate revascularization or reconstruction (Table 1).
Acute upper extremity ischemia is less common than in the lower extremity due to the rich preexisting collateral circulation in both the upper arm and forearm. The majority (˜ 50%) of acute ischemic complications in the upper extremity occur in elderly females as a result of embolic phenomenon rather than primary vessel thrombosis (which accounts for ˜25% of acute ischemic events).3 The differential diagnosis for embolic sources includes intracardiac sources, proximal arterial atherosclerotic plaque, proximal arterial aneurysm thrombus, endocarditis, or paradoxical embolus from venous circulation.
Chronic arterial occlusive disease is rarely symptomatic. Associated comorbid conditions include diabetes, chronic atherosclerotic occlusive disease, subclavian or arteriovenous steal syndromes, or failure of prior arterial repair or grafting.4,5
Venous occlusive disorders in the upper extremity are common and are usually associated with iatrogenic injury, indwelling catheters, or thoracic outlet pathology. For further information regarding venous thoracic outlet disorders. Distal to the thoracic outlet, venous occlusive disorders are for the most part managed expectantly with anticoagulation therapy. Open surgical and endovascular therapies are rarely used and, due to high recurrence and failure rates, are not enthusiastically recommended. For further recommendations regarding upper extremity venous disease management, please refer to additional references.6,7
Table 1: Upper Extremity Vascular Disease | ||||||||
|---|---|---|---|---|---|---|---|---|
|
PATIENT HISTORY AND PHYSICAL FINDINGS
Initial evaluation should include an assessment of associated comorbidities, including cardiac pathologies (myocardial infarction, arrhythmia, heart failure, or prior coronary artery revascularization), hypertension, hyperlipidemia, diabetes, hypercoagulability, smoking, prior upper or lower extremity arterial intervention, or index extremity trauma.
Symptoms and signs of acute arterial ischemia include pain, paresthesia, pulselessness, paralysis, and/or poikilothermia. A thorough vascular, sensory, and motor examination will help assess the severity of arterial insufficiency. Although dated, the Rutherford classification system remains useful for prognostic determinations.8 For classes 5 and 6 ischemia, urgent or emergent intervention may be necessary to preserve limb function and viability. Prompt removal of embolic debris in limbs with sufficient residual viability produces excellent long-term results.3
Chronic limb ischemia may also present with symptoms of rest pain, pain with extremity use, paresthesia, pulselessness, poikilothermia, and/or ulcerations/wounds/gangrene of fingers or fingertips. Subjects should be asked to describe what, if any, activities exacerbate these potential symptoms (i.e., lifting or carrying material with affected arm/hand, arm raising, or repetitive arm/hand movement). Patients with vocational or recreational activities that require regular or frequent use of their upper extremities should describe convincing symptoms they experience in relation to these activities. More commonly, chronic upper extremity arterial ischemia is asymptomatic, particularly in older and less physically active individuals. In general, revascularization is not necessarily indicated in these circumstances. Discrepancy in upper extremity pulses, or brachial blood pressure differential of more than 15 mmHg, is a hallmark of chronic upper extremity arterial insufficiency with or without accompanying symptoms.
Traumatic or iatrogenic injury accounts for 25% of patients presenting with acute upper extremity arterial insufficiency. Consideration of the mechanism of injury (blunt, penetrating, hyperextension, or avulsion) will help delineate the likely nature of the resulting arterial disruption (transection, dissection, or thrombosis, with or without ongoing extravasation). Following completion of the trauma primary survey, determination of extremity arterial continuity should be performed following reduction of obvious ipsilateral upper extremity fractures and dislocations. In complex injuries, including avulsions and crush injuries, baseline sensory and motor status should be documented early to formulate the most appropriate course of therapy. When severe arterial injury is associated with transection or avulsion of the brachial plexus and compound long bone fractures, meaningful functional recovery, despite ultimately successful revascularization, may not be possible.9
More commonly, upper extremity arterial injuries can be more subtle and are frequently missed on primary or secondary surveys. The extensive collateral network present around the elbow often masks the presence of brachial artery thrombosis following posterior elbow dislocation, or dissection and thrombosis following brachial artery catheterization. When physical signs suggest asymmetric or reduced upper extremity arterial perfusion, objective imaging should be obtained promptly to direct therapy and maximize long-term function. Depending on hand perfusion and viability, occasionally, immediate revascularization can be at least temporarily deferred to allow for more urgent resuscitation and stabilization procedures to proceed. Similarly, non-flow-limiting dissections may be monitored without immediate intervention, particularly when the patient’s overall condition merits observational management.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Depending on clinical circumstances, revascularization may be undertaken on the basis of clinically apparent injuries and limb ischemia. More commonly, physiologic assessment is indicated and necessary to determine the most efficacious method of revascularization. Arteriography, typically performed during or immediately prior to revascularization, remains an essential tool to guide intervention and confirm procedural success. As a general observation, physiologic testing helps determine when intervention is necessary, whereas arteriography provides the necessary anatomic information to ensure procedural and functional success.
Computed tomography (CT) arteriography can potentially add useful information to surgical planning for upper extremity revascularization. However, unlike in the abdomen and lower extremities, significant insight into disease localization and severity in the upper extremities can be gleaned from physical examination and nonionizing imaging modalities such as ultrasound. The potential additional diagnostic benefit associated with CT angiography needs to be balanced with the not insignificant radiation dosage delivered with this imaging modality, particularly in regard to the longer life expectancy of younger patients. When vascular disease is known to be limited to the extrathoracic upper extremity arterial system, CT angiography provides little additional, useful information over diagnostic arteriography alone, especially when the latter can be paired with a therapeutic intervention.
Noninvasive vascular testing for evaluation of the upper extremities includes segmental systolic pressure measurements using a Doppler flow detector, digital plethysmography, and arterial duplex scanning.
Serologic tests are the basis for the workup of patients with suspected vasculitic pathologies (e.g., Takayasu’s arteritis, giant cell arteritis, Buerger’s disease, and/or scleroderma). Customary tests include baseline complete blood count, platelets, fibrinogen, C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR).10,11 In certain circumstances, color duplex evaluation may also provide additional clues to aid in the diagnosis.12 Additional serial serologies and rheumatologic consultation may be necessary depending on the severity and progression of the suspected vasculitic disease process.
Young patients with acute primary arterial thrombosis, patients with recurrent arterial thrombosis, or patients with a prior history of unprovoked deep venous thrombosis preceding an arterial event should be considered for a hypercoagulability workup and hematology consultation. Initial testing may include protein C function, free protein S, antithrombin III activity, anticardiolipin antibodies, factor V Leiden mutation, prothrombin mutation, and homocysteine level.13
SURGICAL MANAGEMENT
Preoperative Planning
Prior to attempted upper extremity arterial repair or revascularization, a clear understanding of the extent and location of arterial pathology is essential. This knowledge guides the location of arterial exposure or optimal method of arterial access, the identification of optimal inflow sources and outflow targets, and the most effective and efficient methods of reconstruction. When uncertainty persists, intraoperative arteriography provides essential and timely guidance.
As in all methods of peripheral arterial reconstruction, heparin is typically administered when an interventional sheath is first placed, or arterial control is anticipated. Typically, 100 units/kg of intravenous heparin is administered, with additional anticoagulation guided by the activated clotting time monitored during the course of the procedure.
As discussed in Part 6, Chapter 2, the preferred extrathoracic method of innominate or proximal left subclavian artery surgical reconstruction is carotid subclavian bypass. Frequently, however, endovascular options are available and preferable in patients who cannot tolerate the risks or morbidity associated with open reconstruction. For example, in the setting of uncontrolled, life-threatening hemorrhage from penetrating or crush injuries or limb avulsion, bleeding may be controlled by insertion of covered, self-expanding stents across the area of injury in the subclavian or axillary arteries. However, with few other exceptions (such as lesions associated with giant cell or Takayasu’s arteritis), angioplasty and stenting of arterial lesions at or distal to the clavicle is poorly tolerated and ill advised. Stents placed in this area are at high risk for fragmentation and subsequent arterial thrombosis, pseudoaneurysm formation, or stent migration.
Surgical management of arterial pathology distal to the subclavian artery (surgical management of arterial disease of the arch vessels and subclavian artery are discussed in Part 6, Chapters 1, 2, and 9) and proximal to the wrist (surgical management of arterial disease distal to the wrist is discussed in Part 6, Chapter 11) will depend on acuity, cause/type of pathology (penetrating trauma, blunt trauma, occlusion, stenosis, or aneurysm), severity of patient symptoms, patient comorbidities, and required durability of the planned repair.
Axillary artery exposure is guided by the nature of the planned reconstruction. The proximal artery is most easily exposed via a transverse infraclavicular incision. Exposure of the second and third portions requires deltopectoral or axillary approaches, respectively.1
Acute symptomatic embolic occlusion of the axillary or brachial arteries are best managed by open, preferably image-guided, balloon catheter or direct thromboembolectomy.1,2 Essential elements required for thromboembolectomy include (1) determination of the optimal treatment environment (operating room [OR] with portable vs. fixed imaging), (2) arterial access (level of incision), (3) acquisition of catheters and guidewires
required to transverse the embolus and accumulated luminal thrombus, (4) availability of balloon and over-the-wire embolectomy catheters, (5) need for adjuncts such as aspiration catheters (Export™ catheter, Medtronic, Minneapolis, MN) and thrombolytic agents (tissue plasminogen activator [tPA]), (6) options for managing postischemic hyperemia and elevated compartment pressures, and (7) consideration of treatment alternatives should preexisting atherosclerotic occlusive disease preclude or complicate catheter-directed thromboembolectomy.
For symptomatic axillary or brachial artery thrombosis not amenable to direct or catheter-based, image-guided thromboembolectomy, open surgical bypass or interposition grafting is the preferred method of repair. When considering open bypass or interposition grafting distal to the clavicle, key planning elements include (1) determination of optimal inflow and outflow, (2) conduit (almost exclusively autogenous vein), and (3) assessment of distal compartment pressures and potential need for fascial release. Commonly, more vasospasm is engendered by injury and surgical manipulation in the upper extremity arteries as compared to those of the lower extremities, and accommodations may need to be made to ensure graft and bypass patency in this context.
Branch vessel injuries and aneurysms, particularly those arising from the axillary and brachial arteries, are best treated with ligation and excision.14 Preoperative planning of these procedures involves selection of an appropriate exposure through the muscles of the upper extremity that will facilitate rapid recovery and minimize risk of disability in a usually young and active patient cohort.
The relatively superficial location of the brachial artery in the antecubital fossa increases its vulnerability to traumatic and iatrogenic injury.15 Most brachial injuries are associated with penetrating trauma; however, blunt injuries also occur, particularly in the distal brachial artery, following posterior elbow dislocations and supracondylar fractures (the latter more commonly in children).16 In these situations, key elements for repair will include inspection of injured arterial segment on preoperative imaging for possible intimal disruption, short segment thrombosis, or thrombosis extending distally into the forearm.
An increasing number of cardiac catheterizations and coronary interventions are performed via radial or brachial access.17 Cannulation site complications, including thrombosis or pseudoaneurysm formation, often necessitate operative repair.17,18 For these patients, preoperative planning will include identifying the extent of injury, options for graft conduit (smaller diameter vein), and alternative management options including arterial ligation in extenuating circumstances.
The ulnar artery at the wrist is the dominant hand artery in the majority of patients. Achieving or maintaining sufficient arterial outflow at the wrist is essential to the hemodynamic and clinical success of forearm revascularization procedures. The status of the radial and ulnar arteries at the wrist should be confirmed in the course of evaluating all patients for upper extremity revascularization options.
Operating Room Setup
The majority of upper extremity revascularization procedures are suited for a hybrid operating environment, or an OR equipped with a radiolucent, floating-point carbon fiber operating table and fluoroscopy radiation source and image intensification system, preferably equipped with digital subtraction angiography and last-image hold capabilities. When optimal x-ray penetration and resolution is not available, or in circumstances when diagnostic angiography alone is anticipated, less sophisticated portable imaging systems may suffice.
Elective and emergent upper extremity surgical revascularization procedures may be performed with either regional or general anesthesia. Considerations include the overall status of the patient, ability to tolerate the specific challenges associated with either anesthetic techniques, and the abilities of the anesthesiologist responsible for anesthetic management.
For the majority of upper extremity procedures, the operative limb is typically extended at 90 degrees. For optimal surgical exposure, we prefer arm positioning systems that move freely with the OR table rather than those with separate floor extensions. To avoid exacerbation of potential brachial plexus injuries in appropriate clinical settings, care should be taken to avoid hyperabduction and extension of the limb. The operative field should include, at a minimum, the ipsilateral axilla, chest, and neck, with the head rotated and extended to the contralateral side. A shoulder roll may be positioned under the ipsilateral shoulder to aid with neck and shoulder extension (FIG 1A). Alternatively, for optimal deltopectoral exposure of the axillary artery, the arm can be externally rotated and abducted at 30 degrees relative to the lateral chest.
In situations where venous interposition conduit may be needed, a lower extremity should also be prepared into the surgical field to allow for greater or lesser saphenous vein harvest as indicated by the estimated diameter of the target artery. In the setting of extensive traumatic injuries, vein should be harvested from the least affected lower extremity.
TECHNIQUES
Systemic anticoagulation should be considered whenever major open or endovascular revascularizations are undertaken. Exceptions include profound systemic coagulopathy or concern related to concomitant risks such as occult intracranial hemorrhage. Sufficient intravenous unfractionated heparin should be administered to achieve an activated clotting time of more than 250 seconds.
Open surgical revascularization and repair techniques are described in the sections in the following text relative to upper extremity anatomic location.
The last section describes general endovascular techniques used for upper extremity interventions.
PROXIMAL AXILLARY ARTERY
First Step
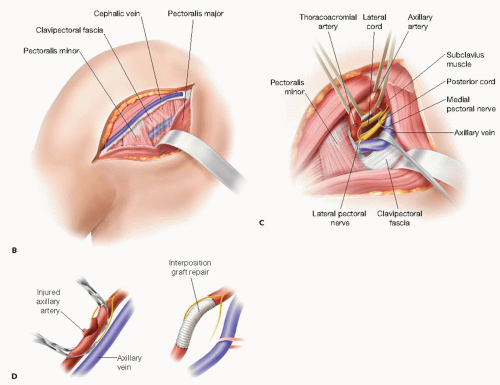
Exposure of the proximal (first) portion of the axillary artery is best achieved through an incision placed one fingerbreadth below the middle third of the clavicle (FIG 1B). Deep to the subcutaneous tissue, the pectoral fascia is opened longitudinally. The pectoralis major muscle is divided with a muscle-splitting incision. The underlying clavipectoral fascia is then sharply incised to expose the proximal axillary sheath. Additional exposure is aided by lateral retraction or division of the pectoralis minor muscle.
Second Step
Fine dissection should be used to expose and control the axillary artery deep to the clavipectoral fascia. Careful dissection and retraction minimizes injury to the cords of the brachial plexus surrounding the artery. The lateral pectoral nerve and proximal cephalic vein are also prone to injury during dissection or traction from misplaced self-retaining retraction devices.
Third Step
The axillary vein lies anterior and caudal to the artery within the axillary sheath. Mobility of the vein is achieved with gentle dissection, ligation of associated venous tributaries, and mild caudal retraction with a circumferential vessel loop or small handheld retractor (FIG 1C).
In smaller patients, division of the thoracoacromial artery and vein may be required to facilitate proximal axillary exposure. Once again, injury to the lateral pectoral nerve is avoided by gentle, deliberate dissection.
Fourth Step
Once circumferential dissection and exposure of the proximal axillary artery is complete, the artery is optimally controlled with silastic vessel loops (FIG 1C).
Familiar anatomic relationships may be less recognizable during redo or complex exposures, or in the setting of traumatic injuries, ongoing extravasation, and hematoma formation. The risk of associated brachial plexopathy is heightened in these situations. Extending exposure through the deltopectoral groove may help delineate otherwise indistinct tissue planes. Repositioning the arm throughout the range of available abduction may also reduce position-related anatomic distortion.