Primary Melanocytic Neoplasms
Elisabeth J. Rushing, MD
Key Facts
Terminology
Spectrum from low-grade melanocytoma to malignant melanoma
No consensus grading system
Clinical Issues
Sites
Posterior fossa, spinal cord, supratentorial
Prognosis
Good for melanocytoma
Guarded for intermediate lesions
Poor for melanoma, but better than for metastatic melanoma to CNS
Image Findings
Heavily pigmented cases are dark on T2WI and bright on pre-contrast T1WI
Microscopic Pathology
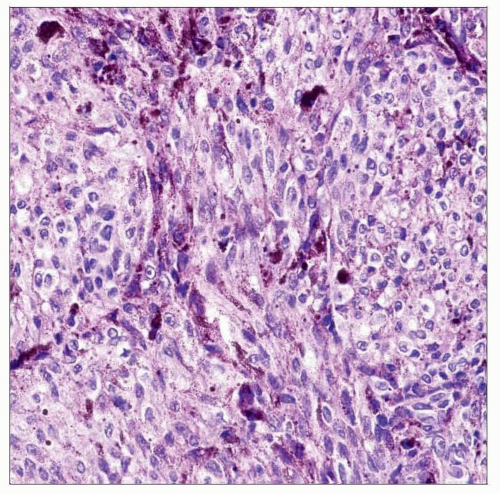
Mitotic activity minimal or absent in melanocytoma
Nested architecture, in some cases, especially lower grade
Meningioma-like, sheet-like, or lobular architecture in some cases
Spindled or epithelioid cells more likely in melanoma
Nucleoli small in most melanocytomas; large, eosinophilic in melanomas, but also in some melanocytomas and intermediate lesions
Necrosis and invasion in melanoma
Ill-defined intermediate category
Top Differential Diagnoses
Melanotic schwannoma, meningioma
TERMINOLOGY
Definitions
Uncommon neoplasms derived from normal leptomeningeal melanocytes
Nodular mass
Morphologic spectrum from low-grade melanocytoma to melanocytic tumor of intermediate differentiation to malignant melanoma
No consensus on precise criteria distinguishing these subdivisions
Diffuse leptomeningeal infiltrate
Meningeal melanocytosis/melanomatosis (neurocutaneous melanosis) (rare)
ETIOLOGY/PATHOGENESIS
Developmental Anomaly
Neurocutaneous melanosis
Aberrant expression of hepatocyte growth factor/scatter factor (HGF) implicated
CLINICAL ISSUES
Epidemiology
Incidence
Rare
Age
Mostly adults
5th decade for focal malignant melanoma
4th decade for diffuse melanomatosis
Children with neurocutaneous melanosis syndrome
Symptomatic by 2 years of age
Gender
Primary CNS nodular melanoma more common in males
No preference for neurocutaneous melanosis
Ethnicity
Caucasians > other races
Site
Posterior fossa
Base of skull
Cerebellopontine angle
Meckel cave
Melanocytoma in this site associated with nevus of Ota
Spinal cord
Intradural extramedullary
Most melanocytomas arise at cervical and thoracic levels
Largely intramedullary (rare)
Supratentorial
Leptomeninges
Intraventricular (rare)
Presentation
Nodular mass
Site-dependent deficits
Diffuse leptomeningeal infiltrate
Seizures
Signs/symptoms of increased intracranial pressure
Myelopathy with spinal cord involvement
Treatment
Complete surgical resection for melanocytoma
No effective therapy for others
Prognosis
Good for melanocytoma
Rarely undergo malignant transformation
Guarded for melanocytic tumors of intermediate differentiation
Poor for melanoma, but
Better prognosis for primary CNS than metastatic melanoma
Poor for neurocutaneous melanosis
Majority undergo malignant transformation with death by 4 years of age
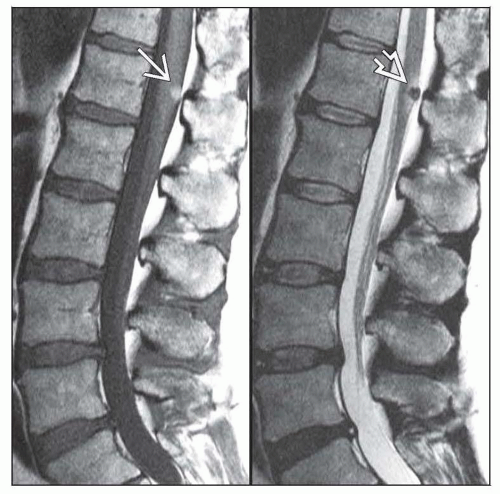
IMAGE FINDINGS
MR Findings
Nodular mass
Extraaxial and well circumscribed
Iso-, hypointense on T2WI and hyperintense on pre-contrast T1WI
Homogeneous enhancement
T1 and T2 signal characteristics dependent on melanin content
Highly pigmented lesions bright on pre-contrast T1WI and dark on T2WI
Most lesions not sufficiently pigmented to generate these signal characteristics • Diffuse leptomeningeal infiltrate
T1 shortening within brain parenchyma & meninges
Leptomeningeal or intraparenchymal enhancement heralds malignant transformation
MACROSCOPIC FEATURES
General Features
Nodular mass
Solitary mass lesions, pigmented or nonpigmented
Hemorrhage or necrosis in some cases
Diffuse leptomeningeal infiltrate
Dense, black subarachnoid staining
MICROSCOPIC PATHOLOGY
Histologic Features
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree