Popliteal Dissection
Glenda G. Callender
Kelly M. McMasters
DEFINITION
Popliteal dissection, or popliteal lymphadenectomy, is the removal of all lymph node-bearing tissue from the popliteal fossa. This procedure is most commonly performed for melanoma but may rarely be performed for other cutaneous cancers or for the limited number of sarcomas that have a propensity to metastasize to lymph nodes.
Popliteal dissection is indicated in patients with no evidence of distant metastatic disease who are found to have the following:
Positive popliteal sentinel lymph node biopsy (microscopic nodal disease)
Clinically positive popliteal lymph nodes (macroscopic nodal disease)
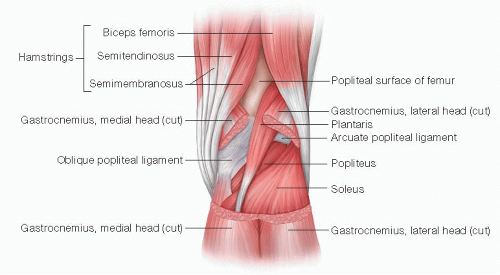
Boundaries of the popliteal fossa (FIG 1)
Superomedial: semitendinosus and semimembranosus muscles
Superolateral: biceps femoris muscle
Inferomedial: medial head of the gastrocnemius muscle
Inferolateral: lateral head of the gastrocnemius muscle and plantaris muscle
Roof: skin, superficial fascia, deep (popliteal) fascia
Floor: popliteal surface of femur, capsule of knee joint, oblique popliteal ligament, fascia overlying popliteus muscle
PATIENT HISTORY AND PHYSICAL FINDINGS
A thorough history should be elicited prior to treatment, including a detailed past medical and surgical history, present medications and allergies, and a personal and family history of cancer. A complete head-to-toe skin examination should be performed. All lymph node basins (cervical, supraclavicular, axillary, epitrochlear, inguinal, popliteal) should be evaluated for clinically positive lymph nodes.
Clinically positive lymph nodes typically present as a palpable mass. However, enlarged lymph nodes in the popliteal fossa may not be easily palpable because of the thick overlying fascia. Therefore, a careful examination of the popliteal fossa is essential.
Most patients undergo popliteal dissection because of a positive sentinel lymph node biopsy. Sentinel lymph node biopsy has now become the standard of care for evaluating regional lymph node basins in patients with cutaneous melanoma greater than 1 mm in Breslow thickness who have no evidence of distant metastatic disease (see Part 5, Chapter 27). Current standard of care for patients with positive sentinel lymph nodes includes completion lymphadenectomy of the involved lymph node basin; observation alone should be performed in the context of a clinical trial. Approximately 50% of patients with a positive popliteal sentinel lymph node biopsy will also have documented inguinal disease; therefore, popliteal and inguinal dissections are often performed concomitantly.1,2
IMAGING AND OTHER DIAGNOSTIC STUDIES
A clinically positive lymph node should be evaluated using fine needle aspiration biopsy. Popliteal dissection is performed for a positive biopsy.
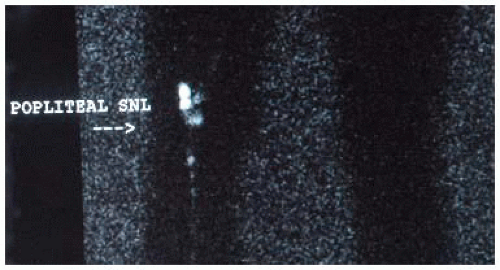
For patients with clinically negative lymph nodes, preoperative lymphoscintigraphy should be performed at the time of the initial sentinel lymph node biopsy even if the primary melanoma is located on an extremity. Lymphoscintigraphy will demonstrate drainage to popliteal lymph nodes in 1% to 9% of patients with distal lower extremity melanoma (i.e., below the knee; FIG 2).1, 2, 3, 4, 5 By far, the most common locations for primary melanomas that drain to the popliteal fossa are the posterolateral foot and posterior lower leg; however, primary melanomas of the anterior lower leg or
anteromedial aspect of the foot will also occasionally drain to the popliteal fossa.1, 2, 3, 4 The overall incidence of a positive popliteal lymph node is 0.3% to 2.8%.1, 2, 3,5
SURGICAL MANAGEMENT
Preoperative Planning
In the preoperative area, a focused history and physical examination should be repeated, and the patient’s prior pathology and imaging studies should be reviewed.
The patient should be marked to confirm laterality.
Although there are no data that specifically address the wound infection rate in popliteal dissection, we favor the administration of a dose of preoperative antibiotics, particularly if concomitant inguinal dissection is planned.
Positioning
The patient is placed prone, with pressure points padded, and the operative knee slightly flexed (FIG 3). The operative leg should be prepped circumferentially from above the midthigh to below the midcalf.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree