|
Clinical Features |
Microscopic Features |
Ancillary Investigations |
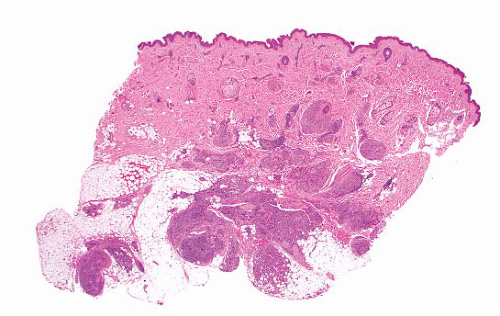
Plexiform fibrohistiocytic tumor |
Young adults, mostly upper limb, head and neck
One-third recur, rare cases metastasize |
Nodules based on dermal-subcutaneous junction
Rounded cells, multinucleated cells, lymphocytes
Some have branching bundles of fibroblasts
Rarely myxoid or atypical |
SMA+, CD68+, CD34−, S100 protein− |
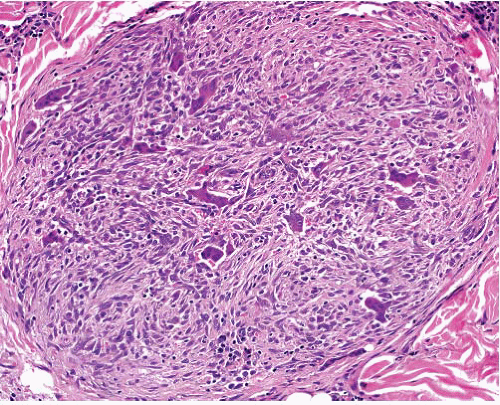
Giant cell tumor of soft parts of low malignant potential |
Mostly upper limb
Subcutaneous or subfascial
Multinodular or circumscribed
Can recur, rarely metastasizes |
Uniformly distributed large osteoclast-like giant cells, bland mononuclear cells
Hemorrhage, peripheral osteoid, or bone formation
Vascular invasion |
CD68+ in giant cells |
Cellular neurothekeoma |
Young adults, upper extremity, head and neck
Recurrence rare, no metastases |
Dermal
Rounded nodules of uniform rounded cells
Multinucleated cells rare
Often myxoid
Can show focal nuclear atypia |
SMA+, NKIC3+, MITF+, S100 protein−, HMB45− |
Dermal nerve sheath myxoma |
Circumscribed multilobulated myxoid lesion, low cellularity |
Spindle cells can show focal pleomorphism or multinucleation |
S100 protein+ in myxoid areas, EMA+ at periphery of nodules |
Plexiform schwannoma |
Young adults, extremities, head and neck, gastrointestinal tract
Deep variant mostly in females |
Dermal or subcutis, rarely deeper
Variably sized nodules of Schwann cells
Mostly Antoni A pattern
Nuclear pleomorphism can be seen, but necrosis rare
Cellular variant has hypercellular fascicles, mitoses |
S100 protein+, EMA+ at periphery of nodule |
Plexiform neurofibroma |
Associated with neurofibromatosis type 1
Can involve large nerves in deep locations or more superficial ones
Can undergo malignant change
Can extend extraneurally as diffuse neurofibroma |
Transitions from normal nerve
Nerve expanded by variable myxoid stroma and increased cellularity
Atypical variant has nuclear crowding, pleomorphism
Diffuse extraneural component in some |
S100 protein+ focally |
Diffuse neurofibroma |
Some associated with neurofibromatosis type 1
Children and young adults
Head and neck, subcutaneous infiltrative plaque
Associated with plexiform neurofibroma—extends outside nerve bundles into soft tissue |
Sheets of short spindle cells in loose fibrous stroma, infiltrating between normal structures
Wagner Meissner bodies |
S100 protein+ diffusely in nuclei |
Plexiform xanthoma |
Adult males, solitary or rarely multiple
Knee, elbow
Hypercholesterolemia rare |
Irregularly sized nodule in dermis and subcutis
Sheets of vacuolated macrophages
Occasional giant cells |
CD68+ |
Plexiform ossifying fibromyxoid tumor |
Young adults, limbs, head and neck |
Subcutaneous
Each nodule encapsulated
Glomus-like cells with small rounded nuclei and clear cytoplasm |
S100 protein+, GFAP+, desmin+ focally. EP400-PHF1 fusion transcripts |
Plexiform leiomyoma |
Subcutaneous or female genital tract
No specific clinical features |
Nonencapsulated nodules without atypia, mitoses, or necrosis |
SMA+, desmin+, h-caldesmon+ |