Pityriasis Lichenoides
Julie E. Jackson, MD
Chandra N. Smart, MD
Key Facts
Terminology
PLEVA
Mucha-Habermann disease, febrile ulceronecrotic Mucha-Habermann disease
Recurrent crops of erythematous papules of unknown etiology favoring children or young adults and spontaneously resolving over weeks
PLC
Guttate parapsoriasis
Chronic form of PLEVA also typically affecting children but can affect any age; predominantly truncal rash persists for years
Microscopic Pathology
PLEVA
Superficial perivascular brisk lymphocytic infiltrate with interface change at dermal-epidermal junction; infiltrate extends into reticular dermis in wedge-shaped fashion
Epidermis with overlying crust, foci of parakeratosis, acanthosis, and basal layer vacuolar change
PLC
Blunted features of PLEVA seen
Parakeratosis with less lymphocytic infiltrate in dermis and less interface change at dermal-epidermal junction with focal apoptotic keratinocytes
No atypical lymphocytes in either entity
TERMINOLOGY
Synonyms
Pityriasis lichenoides et varioliformis acuta (PLEVA), Mucha-Habermann disease, febrile ulceronecrotic Mucha-Habermann disease
Pityriasis lichenoides chronica (PLC), guttate parapsoriasis
ETIOLOGY/PATHOGENESIS
Unknown
Proposed hypersensitivity reaction to viruses, possible autoimmune association (rheumatoid arthritis, hypothyroidism, pernicious anemia), or drug induced
CLINICAL ISSUES
Presentation
PLEVA
More common in children with male predominance; asymptomatic recurrent crops of crusted erythematous papules or vesicles that self resolve over a period of weeks
In acute febrile ulceronecrotic variant, constitutional symptoms such as fever, malaise, arthritis, and lymphadenopathy are also present
Those with diffuse skin lesions appear to have shorter course than patients with peripheral skin lesions
PLC
Any age group can be affected but often seen in children as red brown papules with characteristic scale that slowly regress over months
Can take on a chronic relapsing course with prolonged periods of remission in between flares
Treatment
First line with topical corticosteroids, topical coal tar, phototherapy, antihistamines, or oral tetracycline or erythromycin for anti-inflammatory effects
Treat systemic symptoms with systemic corticosteroids and refractory cases with weekly methotrexate
Prognosis
PLEVA: Self resolving over weeks
Acute febrile ulceronecrotic PLEVA: Usually lasts several months with relapsing disease and eventually converts into classic PLEVA; rare reports of death typically in adult cases
PLC: Chronic relapsing course over months with eventual tendency for self resolution, though rare cases of progression to cutaneous T-cell lymphoma have been reported
MICROSCOPIC PATHOLOGY
Histologic Features
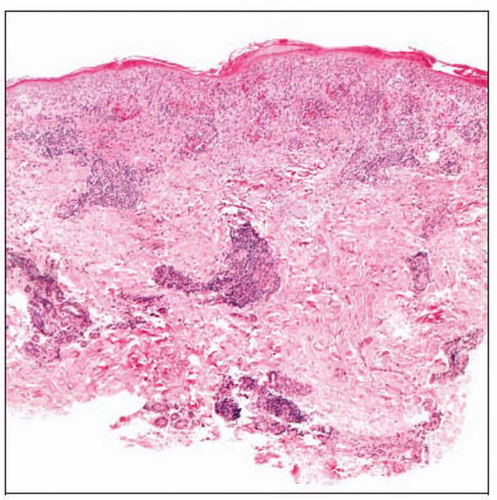
PLEVA
Superficial perivascular brisk lymphocytic infiltrate with interface change at dermal-epidermal junction; infiltrate extends into reticular dermis in wedge-shaped fashion
Prominent lymphocyte exocytosis with intraepidermal red blood cells
Epidermis with overlying crust, foci of parakeratosis, acanthosis, and basal layer vacuolar change
Depending on extent of infiltrate, edema and epidermal necrosis may also be present along with extravasation of red blood cells and lymphocytic vasculopathy
PLC
Blunted features of PLEVA are seen
Parakeratosis with less lymphocytic infiltrate in dermis and less interface change at dermal-epidermal
junction with focal apoptotic keratinocytes
Perivascular lymphocytic inflammation in superficial dermis ± extravasation of red blood cells
No atypical lymphocytes in either entity
DIFFERENTIAL DIAGNOSIS
Lymphomatoid Papulosis
Self-healing benign eruption with malignant-appearing histology
Dense atypical lymphocytic infiltrate distributed in wedge-shaped, lichenoid pattern or large cell variant often with overlying crust and necrotic keratinocytes
Drug Eruption
Wedge-shaped dermal lymphohistiocytic infiltrate with conspicuous eosinophils distinguishing this entity from PLEVA
Arthropod Reactions
Histologic spectrum, but classically wedge-shaped mixed dermal infiltrate with eosinophils, overlying epidermal spongiosis, crust, and occasional identifiable insect mouth parts
Guttate Psoriasis
Eruptive small scattered oval papules and plaques with overlying scale occurring in younger patients
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree