Pictorial Atlas
QUESTIONS
Each of the following questions or incomplete statements is followed by suggested answers or completions. Select the ONE BEST ANSWER in each case.
|
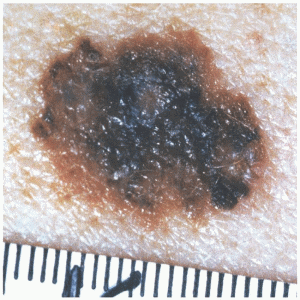
1. A 42-year-old woman presents with the lesion (shown at left) on the back of her calf. She has no significant medical problems and otherwise feels well. The lesion has not bled, but seems to have grown over the last few months. Appropriate initial management of this skin lesion should be
A) Observation and removal if bleeding or further change occurs
B) Complete excision with normal margins
C) Complete excision with wide margins
D) Shave biopsy
E) Electrodesiccation and curettage
View Answer
1. The answer is B. (Complete excision with normal margins) Even in the hands of experienced dermatologists, there is an approximately 15% false-negative rate in determining the presence of melanoma on the basis of examination alone; therefore, histologic confirmation is essential for both tumor diagnosis and staging. A complete excision with normal skin margins is preferable when possible as the first diagnostic step (e.g., excisional biopsy). An incisional biopsy can be performed for larger lesions when complete excision is not practical and when the suspicion of melanoma is low; incisional biopsy does not adversely affect survival. Shave biopsies should be avoided because they may not provide enough tissue for diagnosis and do not allow for accurate depth measurement. All biopsies of lesions suspected of being melanomas should provide a piece of full-thickness skin extending to the subcutaneous fat.
|
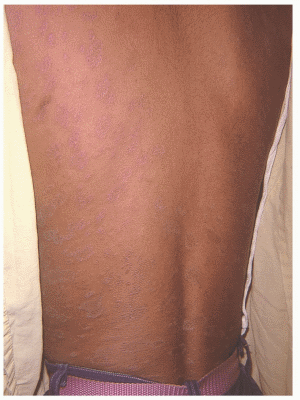
2. A 26-year-old woman presents with the above rash. She states the rash is minimally pruritic and developed over the last week. She has had some virus-like symptoms and reports the rash began as a large salmon-colored patch on her chest area. The most likely diagnosis is
A) Tinea versicolor
B) Pityriasis rosea
C) Varicella
D) Psoriasis
E) Coccidioidomycosis
View Answer
2. The answer is B. (Pityriasis rosea) Pityriasis rosea is a selflimited, exanthematous skin disease that develops acutely and is characterized by the appearance of slightly inflammatory, oval, papulosquamous lesions on the trunk and proximal areas of the extremities. Pityriasis rosea is largely a disease of older children and young adults. It is more common in women than in men. A prodrome of headache, malaise, and pharyngitis may occur in a small number of cases, but except for itching, the condition is usually asymptomatic. The eruption commonly begins with a “herald patch”: a single round or oval, sharply demarcated pink or salmon-colored lesion on the chest, neck, or back, 2 to 5 cm in diameter. The lesion soon becomes scaly and begins to clear centrally, leaving the free edge of the scaly lesion directed inward toward the center. A few days or a week or two later, oval lesions similar in appearance to the herald patch, but smaller, appear in crops on the trunk and proximal areas of the extremities. The long axes of these oval lesions tend to be oriented along the lines of cleavage of the skin. This characteristic Christmas-tree pattern is most evident on the back, where it is emphasized by the oblique direction of the cleavage lines in that location. Most cases of pityriasis rosea need no treatment other than reassurance and proper patient education. Topical steroids with moderate potency are helpful in the control of itching. They can be applied to the pruritic areas two or three times daily. Topical antipruritic lotions such as prax, pramagel, or sarna may also be helpful.
|
3. An 18-year-old man presents to your office complaining of a sandpaper-like rash that affects his upper outer arms. He is otherwise healthy and has no other symptoms. The most likely diagnosis is
A) Scarlet fever
B) Infectious mononucleosis
C) Keratosis pilaris
D) Seborrheic dermatitis
E) Psoriasis
View Answer
3. The answer is C. (Keratosis pilaris) Keratosis pilaris is defined as hyperkeratotic follicular papules on the extensor surface of the upper arms or upper anterior thighs and occasionally on the malar area of the face. It may be associated with atopy and dry skin. A sandpaperlike feel is noted in these isolated areas. The condition is considered benign and is treated with topical lactic acid cream or lotion. Lesions that are associated with the face typically resolve at puberty.
|
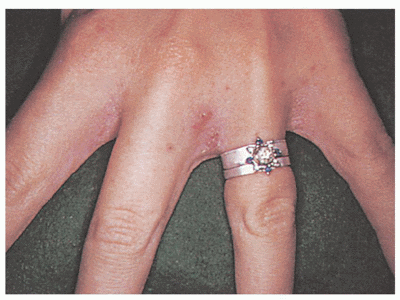
4. A 35-year-old woman presents with a pruritic rash that has been present over the last few weeks. The area affected is in the webs of the fingers, and symptoms are reported to be worse at night. Topical over-the-counter steroids have not been beneficial. The likely diagnosis is
A) Poison ivy
B) Dyshidrotic eczema
C) Scabies
D) Tinea corporis
E) Psoriasis
View Answer
4. The answer is C. (Scabies) The condition of scabies is associated with intense pruritus that is noted predominantly at night. The lesions are brownish in color and often form irregular burrow lines that may be marked with scaling at one end and a vesicle at the other end. The lesions are typically found in intertriginous areas and warm, protected areas such as the finger webs, inframammary areas, and axilla. The mite Sarcoptes scabei is responsible. Scrapings of the lesion are treated with 10% potassium hydroxide solution and studied under light microscopy. The mite is often identified. Treatment consists of permethrin cream 5% applied from head to toes and left in place for 12 hours before being washed off. Lindane can also be used as an alternative, but not in infants or in pregnant women.
|
5. A 72-year-old man presents to your office complaining of an area of redness associated with the perinasal region. He states that the rash is often worse in the summer, and he has noticed that sunlight exposure makes it worse. Appropriate treatment of this condition consists of
A) Hydrocortisone cream
B) Tretinoin gel
C) Metronidazole cream
D) Mupirocin ointment
E) Acyclovir ointment
View Answer
5. The answer is C. (Metronidazole cream) Rosacea is a common problem encountered by family physicians. The condition is associated with areas of erythema and telangiectasia on the face. It is exacerbated by sunlight, hot or spicy foods, and alcohol. Pronounced rosacea may appear as acneiform papules, pustules, or ruddiness. Northern Europeans and those of Celtic descent are most commonly affected. Treatment involves oral tetracycline or doxycycline. Topical metronidazole is also effective for milder cases.
|
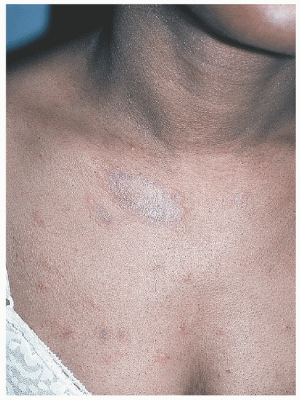
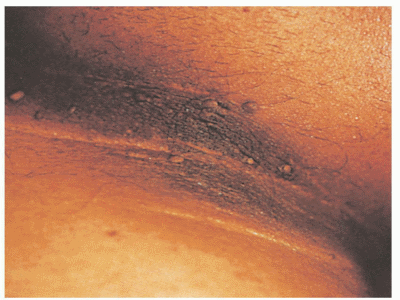
6. Which of the following malignancies is associated with the skin condition shown here?
A) Ovarian carcinoma
B) Gastric carcinoma
C) Malignant melanoma
D) Multiple myeloma
E) Hodgkin’s lymphoma
View Answer
6. The answer is B. (Gastric carcinoma) Acanthosis nigricans is associated with hyperpigmented areas that typically affect flexural folds (axilla). The two basic types of acanthosis nigricans are benign and malignant. The benign form is associated with obesity, diabetes, Stein-Leventhal syndrome, Cushing’s disease, Addison’s disease, pituitary disorders, and hyperandrogenic syndromes. Drugs, including glucocorticoids, nicotinic acid, diethylstilbestrol, and growth hormone therapy, have also caused acanthosis nigricans. Many cases are idiopathic. Malignant acanthosis nigricans is associated with an intestinal cancer such as gastric carcinoma.
|
7. A 45-year-old woman presents with a localized area of erythematous scaly patches that comes and goes and typically affects the elbows. The likely diagnosis is
A) Pityriasis rosacea
B) Mycosis fungoides
C) Tinea corpora
D) Nummular eczema
E) Psoriasis
View Answer
7. The answer is E. (Psoriasis) Psoriasis usually manifests itself as erythematous scaly patches that affect the knees or elbows. More severe cases can involve multiple areas over the entire body. Extensor surfaces are predominantly affected. Nail pitting may be present. The condition appears to be hereditary. Diagnosis is usually based on clinical findings. Skin biopsy may be helpful for definitive diagnosis. Treatment consists of topical steroids, intralesional steroids, tar preparations, anthralin, tazarotene, and calcipotriene.
|
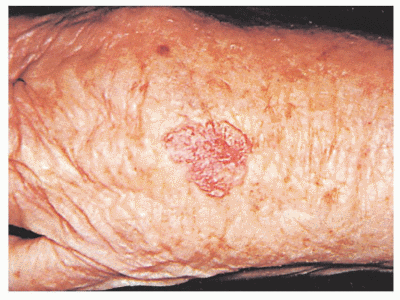
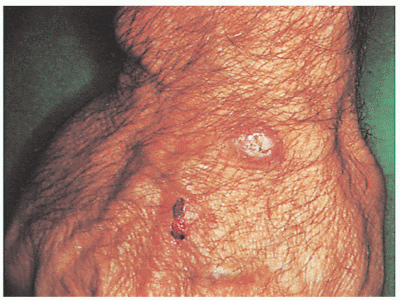
8. A 60-year-old retired construction worker presents with a nonhealing skin lesion on the back of his hand that occasionally bleeds when he gets out of the shower. The most likely diagnosis is
A) Basal cell carcinoma
B) Squamous cell carcinoma
C) Superficial spreading malignant melanoma
D) Actinic keratosis
E) Keratoacanthoma
View Answer
8. The answer is A. (Basal cell carcinoma) Basal cell carcinoma is the most common form of skin cancer. The lesions are induced by ultraviolet radiation in susceptible individuals. Risk factors include age older than 40, light complexion, positive family history, and male sex. The lesion has pearly, raised borders with telangiectasia and a central ulcer that may crust. Sun-exposed areas are most commonly affected. Diagnosis is achieved with shave or excisional biopsy. Treatment is accomplished with excision, electrodesiccation and curettage, liquid nitrogen application, Moh’s surgery, radiation treatment, and topical 5-fluorouracil cream. Almost 50% of patients with basal cell carcinoma will have another within 5 years.
|
9. You note the above skin disorder during a general medical evaluation. You explain to the patient they are at risk for the development of
A) Alzheimer’s disease
B) Tuberculosis
C) Diabetes mellitus
D) Graves’ disease
E) Melanoma
View Answer
9. The answer is C. (Diabetes mellitus) Although the majority of cases of acanthosis nigricans are benign and associated with obesity, the disease can represent the onset of malignancy as well as a variety of conditions related to insulin resistance. Acanthosis nigricans has been reported in association with a number of malignancies, particular gastrointestinal cancers (e.g., gastric, hepatocellular), and lung cancer. The suspicion for malignancy increases in patients with extensive or rapidly progressive lesions, when there is mucous membrane involvement, or when there is prominent sole and palm disease. The common finding in all nonmalignancy-associated cases of acanthosis nigricans is insulin resistance. This explains the relationship between this skin disorder and diseases such as diabetes mellitus, Cushing’s syndrome, and hypothyroidism (most likely due to weight gain and subsequent insulin resistance), and with obesity.
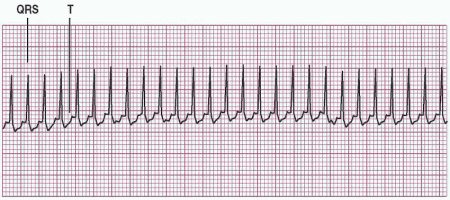
10. A 42-year-old woman presents to the emergency room complaining of shortness of breath and palpitations. An electrocardiogram shows the above tracing. Appropriate management at this time includes
A) Epinephrine
B) Metoprolol
C) Nitroglycerin
D) Adenosine
E) Lidocaine
View Answer
10. The answer is D. (Adenosine) The most important step to make when a narrow QRS tachycardia is noted is whether the patient is experiencing signs and symptoms related to the rapid heart rate. These symptoms include hypotension, shortness of breath, shock, decreased level of consciousness, or chest pain suggestive of coronary ischemia. Determining whether a patient’s symptoms are related to the tachycardia depends on several factors, including age and the presence of underlying cardiac disease. Paroxysmal supraventricular tachycardia (PSVT) with a heart rate of 200 bpm may be tolerated by a healthy young adult with no or few symptoms (e.g., palpitations). However, a heart rate of 120 bpm may precipitate angina in an elderly patient with significant coronary heart disease. Adenosine is approved by the Food and Drug Administration (FD A) in the United States only for the intravenous management of PSVT in which the atrioventricular (AV) node is involved. For intravenous adenosine administration, the patient should be supine and should have electrocardiographic and blood pressure monitoring. The drug is administered by rapid intravenous injection over 1 to 2 seconds at a peripheral site, followed by a normal saline flush. The usual initial dose is 6 mg, with a maximal single dose of 12 mg. The most common side effects of adenosine are facial flushing (18%), palpitations, chest pain, and hypotension. Transient asystole is a rare complication. Another important side effect of adenosine is that it may precipitate atrial fibrillation (AF). In patients with Wolff-Parkinson-White syndrome (WPW), AF can progress into ventricular fibrillation. As a result, caution should be used when giving adenosine if WPW is a possible mechanism, and emergency resuscitation equipment should be available.
|
|
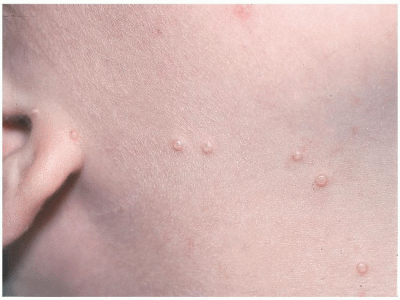
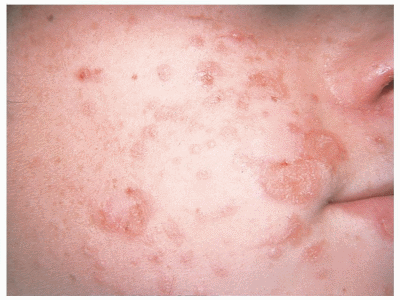
11. A 4-year-old preschooler presents with the skin lesions shown here. The area affected is just below the chin on the child’s right side. The lesions have been present over the last month, and the child has reported no symptoms associated with them. The most likely diagnosis is
A) Varicella
B) Herpes zoster
C) Rhus dermatitis
D) Molluscum contagiosum
E) Scabies
View Answer
11. The answer is D. (Molluscum contagiosum) Molluscum contagiosum is a common, superficial viral infection of the skin that typically occurs in infants and preschoolers. The incidence decreases after the age of 6 to 7 years. The condition can be spread via sexual contact in young adults. The lesions are dome-shaped, waxy, or pearly-white papules with a central white core and are 1 to 3 mm in diameter. Frequently, groups of lesions are found. The lesions may resolve spontaneously. Treatment involves removal with a sharp needle or curette, application of liquid nitrogen, antiwart preparations, electrodesiccation and curettage, or trichloroacetic peels for extensive areas. Typically, infants or young preschool-age children should not be treated aggressively.
|
12. A 16-year-old girl who just returned from a camping trip reports an intensely pruritic vesicular rash associated with the lower extremities. The most likely diagnosis is
A) Rhus dermatitis
B) Lyme disease
C) Chigger bite
D) Brown recluse spider bite
E) Black widow spider bite
View Answer
12. The answer is A. (Rhus dermatitis) Poison ivy or poison oak is also referred to as Rhus dermatitis. The condition is associated with intensely pruritic linear streaks of vesicles, papules, and blisters. The plants contain a resinous oil that gives rise to an allergic response approximately 2 days after exposure. Contrary to common belief, the fluid in the blisters can neither transfer the rash to others nor cause it to spread. Treatment involves topical steroid creams, Burow’s solution, calamine lotion, antihistamines, cool baths with colloidal oatmeal, and oral steroids (for 2 to 3 weeks to prevent rebound dermatitis) for more widespread cases.
|
13. An 82-year-old nursing home resident is seen on monthly rounds. The floor nurse points out the skin lesions shown here. The patient is asymptomatic. Appropriate management includes
A) Punch biopsy
B) Topical 5-fluorouracil cream
C) Cryotherapy
D) Hydrocortisone cream
E) Observation
View Answer
13. The answer is E. (Observation) Seborrheic keratoses are common skin lesions that affect the elderly. They tend to run in families. The average diameter is 1 cm, but they can grow to 3 cm in diameter. The lesions are brown or black, oval in shape, raised, and have a “stuck on” appearance. They most commonly occur on the face, back, neck, and scalp. They may appear suddenly and become pruritic and crusted. Numerous lesions that appear rapidly may signal the development of an underlying malignancy. Treatment is cosmetic and usually reserved for those that are inflamed or causing symptoms.
|
14. An 18-year-old sexually active woman presents with a single ulcer that is located on the lower lip and is painful. She is a smoker and has noticed that the ulcers have been recurrent and correlate with the onset of menses. The most likely diagnosis is
A) Kawasaki disease
B) Aphthous stomatitis
C) Squamous cell carcinoma of the lip
D) Syphilis
E) Koplik’s spot
View Answer
14. The answer is B. (Aphthous stomatitis) Aphthous stomatitis, also known as canker sores, are painful eruptions that affect the mucosal surface of the mouth. The cause is unknown. Lesions typically develop at the same time and resolve in 5 to 10 days. A viral cause has not been proved. A streptococcal bacterium has been implicated. The lesions recur at regular intervals and may correlate with the onset of menses in some women. Treatment consists of toothpaste swish therapy, triamcinolone acetonide (Kenalog in Orabase), or tetracycline solution swish and swallow. Severe cases may respond to systemic corticosteroids.
|
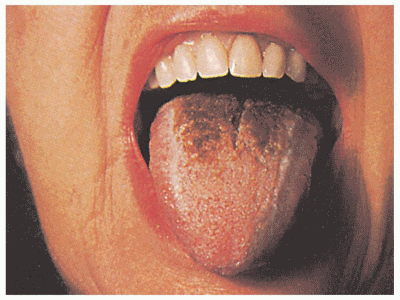
15. Which of the following conditions is the skin finding shown here associated with?
A) Prolonged antibiotic use
B) Sjogren’s syndrome
C) Addison’s disease
D) Chronic gastroesophageal reflux
E) Malignant melanoma
View Answer
15. The answer is A. (Prolonged antibiotic use) Black hairy tongue results from hyperplasia of the filiform papillae with deposition of keratin on the surface. The condition causes the tongue to have a dark, velvety, hairlike appearance. Associated conditions include smoking, consumption of coffee, prolonged use of antibiotics, and possibly acquired immunodeficiency syndrome. Treatment involves using a toothbrush to scrape off the excess keratin that forms on the tongue’s surface.
|
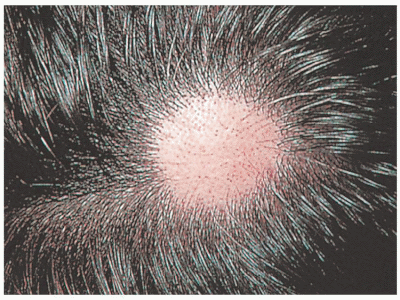
16. A 38-year-old man presents with rapid hair loss that has occurred over the last few weeks. He reports that his father had a similar condition. The most likely diagnosis is
A) Alopecia areata
B) Androgenic alopecia
C) Tinea capitis
D) Trichotillomania
E) Secondary syphilis
View Answer
16. The answer is A. (Alopecia areata) Alopecia areata is associated with sudden hair loss that occurs in round patches. The patches are well circumscribed and are not associated with scarring or inflammation. Patients have no other symptoms. The most common area affected is the scalp; however, the condition may also affect the eyebrows or beard. Alopecia areata usually affects children and young adults and is recurrent. A pathognomonic sign for alopecia areata is the “exclamation point” hair, which is wide distally and narrower at the base. These hairs are often found at the periphery of a patch of hair loss. Hair that regrows in the area of alopecia areata is in many cases white. Nail pitting may also be present. The treatment consists of injection of intralesional steroids and topical steroids. Most experience complete regrowth of hair.
|
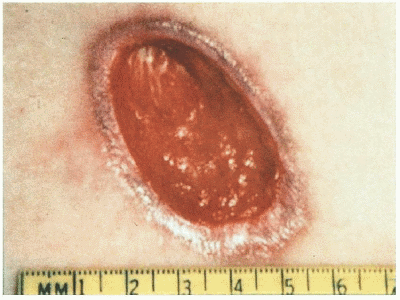
17. The condition shown here was noted associated with an 88-year-old debilitated nursing home resident. He has no evidence of bacteremia or osteomyelitis. Which of the following is an acceptable treatment?
A) Application of povidone-iodine gauze two times per day
B) Application of hydrogen peroxide 3 times per day
C) Systemic antibiotics for 7 to 10 days
D) Keeping the area clean and dry until granulation tissue forms
E) Surgical debridement
View Answer
17. The answer is E. (Surgical debridement) When treating pressure ulcers, it is important to maintain a moist environment while keeping the surrounding skin dry. This can be accomplished by loosely packing the ulcer with saline-moistened gauze. Topical antimicrobials such as silver sulfadiazine cream may be helpful in ulcers that appear infected. Topical antiseptics such as povidone-iodine or hydrogen peroxide should not be used in the treatment of pressure ulcers. Systemic antibiotics should be reserved for serious infections (e.g., bacteremia, osteomyelitis). A 2-week trial of topical antimicrobials may be considered for ulcers that do not appear infected but are not improving. Although most patients are successfully managed without surgery, procedures may be appropriate in patients whose quality of life would be markedly improved by rapid wound closure. Stage 3 and 4 ulcers with necrotic tissue should be debrided. Ulcers with minimal exudate that are not infected can be covered with an occlusive dressing to promote autolytic debridement. Ulcers with thick exudate, slough, or loose necrotic tissue should undergo mechanical debridement. Options include wet-to-dry dressings, hydrotherapy, wound irrigation, and scrubbing the wound with gauze. Ulcers with evidence of cellulitis or deep infection should undergo sharp debridement with a scalpel or scissors. Ulcers with a thick eschar or extensive necrotic tissue should undergo sharp debridement as well. However, a thick, dry eschar covering a heel ulcer should generally be left intact. Patients without access to surgical interventions (such as in a long-term care setting) or those who may not be acceptable surgery candidates can be treated with enzymatic debriding agents. Wound debridement should stop once necrotic tissue has been removed and granulation tissue is present.
|
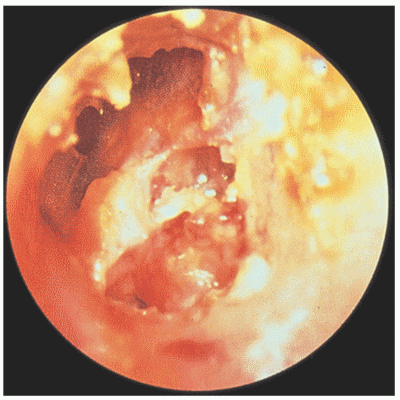
18. A 35-year-old presents with unilateral hearing loss that has been gradual but progressive over the last 6 months. Appropriate treatment of the above condition consists of
A) Prolonged antibiotics for up to 4 weeks
B) Decongestant and antihistamine administration
C) Corticosteroid treatment for 2 weeks
D) Hearing aid amplification
E) Tympanomastoidectomy
View Answer
18. The answer is E. (Tympanomastoidectomy) Cholesteatoma is a growth of desquamated, stratified, squamous epithelium within the middle ear space. The condition occurs when keratin desquamates from the epithelial lining of the sac and gradually enlarges with eventual erosion of the ossicular chain, mastoid bowl, and external auditory canal. The development of a cholesteatoma typically occurs after a retraction pocket has formed in the posterior/superior quadrant of the ear, often as a result of chronic eustachian tube dysfunction. It may also occur after tympanic membrane (TM) trauma, such as a traumatic, inflammatory, or iatrogenic perforation. Without treatment, cholesteatomas may erode the tegmen tympani (the bony covering of the middle fossa), the sigmoid sinus, or even the inner ear. As a result, untreated cholesteatomas can result in lateral sinus thrombosis, sepsis, brain abscess, sensorineural hearing loss, vertigo, disequilibrium, facial paralysis, and even death. Treatment is surgical, usually involving a tympanomastoidectomy.
|
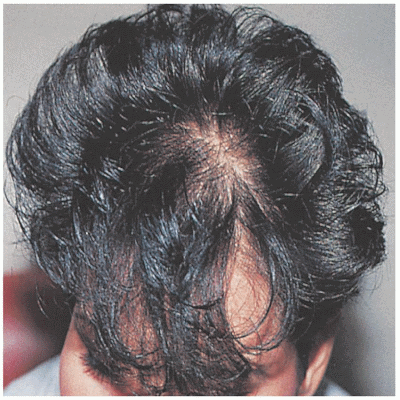
19. A 27-year-old gravida 2, para 2 woman is now 6 months postpartum and complains of excessive hair loss. The most likely diagnosis is
A) Alopecia areata
B) Telogen effluvium
C) Trichotillomania
D) Tinea capitis
E) Hypothyroidism
View Answer
19. The answer is B. (Telogen effluvium) Telogen effluvium is sudden, diffuse hair loss that occurs 3 to 6 months after a stressful event. The causes include medications (heparin, coumarin, propranolol, haloperidol, and lithium), neoplasms, infection, and crash diets. The stressful event triggers the hair follicles to go into a rest phase, and once the cycle returns a larger amount of hair is lost at one time. Typically, 30% to 50% of the scalp hair is affected. No treatment is needed. Patients should be reassured that normal hair growth should resume.
|
20. A 68-year-old man is seen for a general examination and reports a dome-shaped lesion on the back of the hand that has developed over the last few weeks. The lesion is rapidly becoming larger. The most likely diagnosis is
A) Basal cell carcinoma
B) Squamous cell carcinoma
C) Seborrheic keratosis
D) Actinic keratosis
E) Keratoacanthoma
View Answer
20. The answer is E. (Keratoacanthomas) Keratoacanthomas usually develop rapidly over a 2- to 6-week time frame. The lesions are dome-shaped with a central keratin-filled plug. They occur most commonly on sun-exposed areas. Many resolve spontaneously; however, because of their similarity to squamous cell carcinomas and their ability to metastasize, they should be removed by excision. Other treatment options include intralesional methotrexate, 5-fluorouracil, interferon, systemic retinoids, or radiation therapy. Complete excision is usually curative; however, recurrences can develop at the site of treated lesions.
|
21. A 55-year-old woman complains of generalized fatigue, weakness, inability to climb stairs, arthralgias, and dysphagia. Physical examination reveals definite proximal muscle weakness, a periorbital heliotrope rash, and skin findings associated with the hands (shown here). The most likely diagnosis is
A) Lupus erythematosus
B) Sarcoidosis
C) Sjögren’s disease
D) Dermatomyositis
E) Polymyalgia rheumatica
View Answer
21. The answer is D. (Dermatomyositis) Dermatomyositis presents with a heliotrope rash and the presence of Gottron’s papules. The rash is violaceous in color and involves the periorbital areas. Gottron’s papules are erythematous or violaceous papules or plaques that form over the bony prominences, particularly the metacarpophalangeal joints, the proximal and distal interphalangeal joints. The condition is also associated with a myopathy that involves the proximal muscles. The shoulders and pelvic girdle are mainly affected in a symmetric pattern. Symptoms include fatigue, weakness, inability to climb stairs, or weakness in rising from a squatting or sitting position. Dysphagia is also seen. Approximately 20% of patients have an associated malignancy. Laboratory tests include elevated serum creatine kinase or aldolase, or both. Electromyographic studies and a muscle biopsy can also provide additional diagnostic information. The mainstays of treatment are systemic steroids. Other options include immunosuppressant agents and hydroxychloroquine. Those who are older and have severe myositis, dysphagia, associated malignancy, and a poor response to corticosteroids have a poorer prognosis.
|
22. A 50-year-old housewife who enjoys growing roses presents to your office complaining of the lesion shown here. She reports removing a thorn from the area several weeks before. After that, a small painless lump developed that now has crusted over. The most likely diagnosis is
A) Sporotrichosis
B) Blastomycosis
C) Lyme disease
D) Coccidioidomycosis
E) Histoplasmosis
View Answer
22. The answer is A. (Sporotrichosis) Sporotrichosis is a granulomatous fungal infection that affects the skin. The lesion is caused by Sporothrix schenckii, a fungus that grows on wood and in the soil. The lesions typically affect farmers, gardeners (especially those who grow roses), laborers, and miners. A primary chancre occurs at the site of inoculation. The primary lesion is painless and forms a subcutaneous nodule that breaks down to form an ulcer. Within a few weeks, multiple nodules form along the areas of draining lymphatics and break down to form streaks of ulcers, often affecting the arms or legs. The fluid from unopened ulcers can be cultured and can aid in diagnosis. Treatment consists of saturated solution of potassium iodide, ketoconazole, or itraconazole. Systemic invasion is rare.
|
23. A 23-year-old Navy enlisted man is seen in sick bay with the recurrent lesion shown here. The patient reports pain and discomfort associated with the lesion but no dysuria. The likely diagnosis is
A) Molluscum contagiosum
B) Gonorrhea
C) Syphilis
D) Chancroid
E) Herpes infection
View Answer
23. The answer is E. (Herpes infection) Genital herpes is primarily associated with herpes simplex virus type 2. The symptoms include painful vesicles that occur in clusters, often on the shaft of the penis in men or vulvar areas in women. Patients often report fever, regional lymphadenopathy, and generalized fatigue in association with an outbreak. The lesions last for 2 to 3 days before the tops of the vesicles rupture. The remaining ulcers crust over and last an additional 5 to 7 days. Recurrences are common in the same area. Asymptomatic shedding of the virus can occur once the outbreak has resolved and can infect others. Diagnosis can be achieved with the use of Tzanck smears (which detect large bizarre mononucleate and multinucleate giant cells and nuclear changes of ballooning degeneration). Treatment is accomplished with the use of antiviral medications (acyclovir, valacyclovir, famciclovir, and topical penciclovir). Prophylactic therapy may be indicated in recurrent infections.
|
24. A 23-year-old black woman presents with a lesion affecting her groin that has developed over the last few days. Dark-field microscopic examination is negative. The etiologic agent that is responsible for the lesion is
A) Neisseria gonorrhoeae
B) Herpes zoster
C) Treponema pallidum
D) Molluscum contagiosum
E) Haemophilus ducreyi
View Answer
24. The answer is E. (Haemophilus ducreyi) Chancroid is a sexually transmitted disease that is caused by Haemophilus ducreyi. It has a very short (1- to 5-day) incubation period. The primary lesion occurs on the genitalia and forms superficial or deep erosion with surrounding erythema and edema. Marked unilateral and regional lymphadenopathy are present and eventually suppurate, causing buboes in untreated cases. The organisms are arranged like “schools of fish” and are found on smears from active lesions. Treatment consists of a sulfonamide such as sulfisoxazole or third-generation cephalosporin.
|
25. The pictured skin lesion developed over a 4-week period. The most likely diagnosis is
A) Melanoma
B) Basal cell carcinoma
C) Keratoacanthoma
D) Dermatofibroma
E) Molluscum contagiosum
View Answer
25. The answer is C. (Keratoacanthoma) Keratoacanthoma (KA) is a rapidly growing hyperkeratotic nodule with a central keratin plug. A KA typically develops over 3 to 6 weeks, in contrast to the slow growth of typical squamous cell carcinomas (SCCs) over months to years. KAs occur most commonly in areas of sun-damaged skin. KAs are clinically and histologically indistinguishable from welldifferentiated SCC. The etiology of KA is not certain, however; human papillomavirus DNA has been found in some cases. KAs have also occurred in skin soon after radiation therapy. Additionally, there are syndromes of multiple KAs developing over years. There is controversy regarding whether KAs are malignant or benign. Although they resemble SCCs histologically, most spontaneously regress with scar formation. There have been reported cases of invasive KAs, some with metastases, leading many experts to consider all KAs a form of SCC and treat them as such. Because of the uncertain malignant potential of KAs, most are treated as well-differentiated SCC.
|
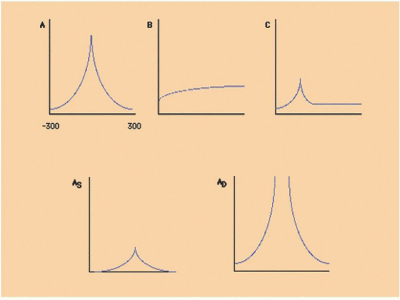
26. Which of the above audiograms represents a likely effusion behind the tympanic membrane?
A) Type A
B) Type B
C) Type C
D) Type As
E) Type Ad
View Answer
26. The answer is B. (Type B) A flattened tympanogram is represented by choices B and is associated with fluid behind the TM or perforation of the TM.
|
27. A 29-year-old man presents in April with the rash shown here. The rash does not itch and has been present over the last week. A large, red area developed first, followed by a more generalized rash that is now present. Physical examination shows that the rash appears in a Christmas-tree pattern on his chest and back. The most likely diagnosis is
A) Pityriasis rosea
B) Tinea versicolor
C) Herpes zoster
D) Varicella
E) Lyme disease
View Answer
27. The answer is A. (Pityriasis rosea) Pityriasis rosea is a common papulosquamous rash that occurs mainly on the trunks of young adults during the spring and fall. The condition begins with the onset of a “herald patch” that is oval and erythematous. Usually within 2 to 10 days, a generalized rash follows. The individual lesions have fine scaling noted around their edges. In many cases, a Christmas-tree pattern is seen over the back. The lesions may continue to appear for 2 to 3 weeks. Most cases resolve by 6 to 8 weeks. Pruritus is often present. The disease is not contagious. Treatment consists of oatmeal colloidal baths, calamine lotion, antihistamines, topical steroids, and ultraviolet-B treatments. Systemic steroids may be necessary for severe cases.
|
28. A 12-year-old boy presents with a crusted honey-brown lesion that affects his cheek. The rash began as red macules 3 days earlier. The best treatment is
A) Intramuscular ceftriaxone
B) Topical hydrocortisone cream
C) Oral ciprofloxacin
D) Topical mupirocin ointment
E) Oral acyclovir
View Answer
28. The answer is D. (Topical mupirocin ointment) Impetigo is caused by group A β-hemolytic streptococci or Staphylococcus aureus and typically affects young children. The lesions begin as erythematous papules that expand to form crusted patches with a honey-brown appearance. More severe cases may cause bullae to form. The infection occurs more commonly around the nose and mouth and in the intertriginous areas; there are no constitutional symptoms. Examination is usually made on clinical presentation. Treatment for mild infections includes 2% topical mupirocin ointment. More severe cases respond to dicloxacillin, cephalexin, or erythromycin. Impetigo is highly contagious. Glomerulonephritis is a rare complication of impetigo that is caused by certain strains of Streptococcus.
|
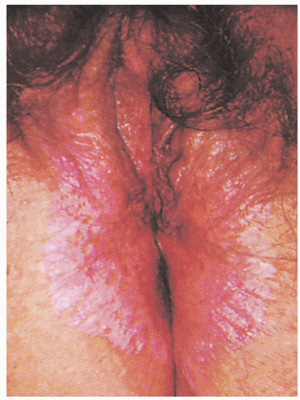
29. A 65-year-old woman presents to your office complaining of gradually increasing dyspareunia. Findings from the physical examination are pictured here. The most likely diagnosis is
A) Yeast vaginitis
B) Herpes genitalis
C) Lichen sclerosis
D) Vitiligo
E) Contact dermatitis
View Answer
29. The answer is C. (Lichen sclerosis) Lichen sclerosis is caused by thinning of the vulvar skin and gives rise to itching and dyspareunia. Atrophy of the skin occurs and gives rise to a shiny whitish appearance. Diagnosis is accomplished with punch biopsy. A slight increase in squamous cell carcinoma has been found in areas that are affected with lichen sclerosis. Treatment consists of potent topical corticosteroids. In addition, a topical antifungal preparation should be used to prevent secondary yeast infections.
|
30. A 45-year-old woman presents with pitting of the nails that has developed slowly over the last few months. The most likely diagnosis is
A) Psoriasis
B) Onychomycosis
C) Hyperthyroidism
D) Chronic obstructive pulmonary disease
E) Scleroderma
View Answer
30. The answer is A. (Psoriasis) Pitting of the nails is commonly associated with psoriasis. Erythematous scaly plaques are usually noted on other parts of the body. Thirty percent of patients with psoriasis have a positive family history for the condition. Men and women are affected equally. Other conditions that are related to nail pitting include alopecia areata and eczematous dermatitis. Chronic obstructive pulmonary disease is related to clubbing. Subungual hyperkeratosis is associated with onychomycosis.
|
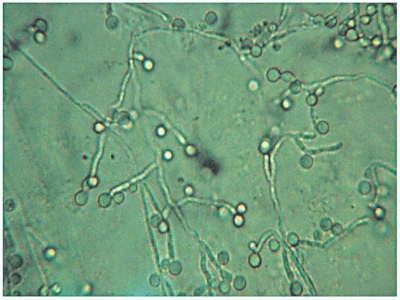
31. A sexually active 24-year-old woman presents to your office complaining of vaginal discharge. Findings from a wet prep are pictured here. The most likely diagnosis is
A) Yeast vaginitis
B) Gardnerella infection
C) Trichomonas infection
D) Gonorrhea
E) Chlamydia
View Answer
31. The answer is A. (Yeast vaginitis) Yeast vaginitis causes approximately one-third of all vaginal infections. Risk factors include pregnancy, diabetes, use of intrauterine devices, recent antibiotic use, immune deficiency, or corticosteroid use. Diagnosis is made by examination of a vaginal smear under high-power microscopy after potassium hydroxide has been added. Budding yeast and pseudohyphae are noted. Topical antifungals are effective, as are single-dose oral antifungals.
|
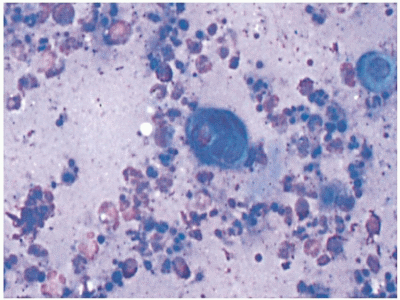
32. The sample shown here was obtained from a penile lesion of a 24-year-old sexually active man. A Tzanck smear was performed. The confirmed diagnosis is
A) Gonorrhea
B) Chancroid
C) Herpes genitalis
D) Syphilis
E) Chlamydia
View Answer
32. The answer is C. (Herpes genitalis) Tzanck smears are used in the diagnosis of herpes infections. The preparation detects multinucleated giant cells. A sample obtained from unroofed vesicles that have appeared within 24 hours provides the best specimen for diagnosis. A #15 blade is used to scrape the base of the vesicle, and the material is spread onto a slide and allowed to dry. Giemsa’s, Wright’s, or methylene blue is used to stain the cells. After staining, the sample is gently flooded with tap water to remove excess stain. Oil immersion is used for viewing with the microscope.
|
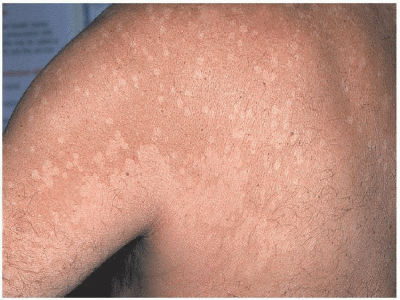
33. An 18-year-old surfer presents with the above skin condition. The most likely diagnosis is
A) Pityriasis rosea
B) Secondary syphilis
C) Seborrheic dermatitis
D) Eczema
E) Tinea versicolor
View Answer
33. The answer is E. (Tinea versicolor) Tinea versicolor is a common skin infection caused by the organism Pityrosporum orbiculare (also known as Malassezia furfur, Pityrosporum ovale, or Malassezia ovalis). The condition usually affects adolescents and young adults in tropical environments. The organism is a yeast that is a constituent of the normal skin flora. A number of factors may trigger conversion to the mycelial or hyphal form that is associated with clinical disease, including hot and humid weather, use of topical oils, hyperhidrosis, and immunosuppression. Tinea versicolor usually responds to medical therapy, but recurrence is common, and long-term preventative treatment may be necessary. Versicolor refers to the variety and changing shades of colors present in this condition. Lesions can be hypopigmented, light brown, or salmon-colored macules. A fine scale is often noted, especially after scraping. Individual lesions are typically small, but frequently coalesce to form larger lesions. Typically the lesions are limited to the outer skin, most commonly on the upper trunk and extremities, and are less common on the face and intertriginous areas. Most patients are asymptomatic; however, some may complain of mild pruritus. The condition may occur in patients who are immunocompromised. It is most evident in the summer because the organism produces a substance that inhibits pigment transfer to keratinocytes, thus making infected skin more demarcated from uninfected, evenly pigmented skin. The diagnosis of tinea versicolor is made by microscopic examination of skin samples with 10% potassium hydroxide (KOH). Both hyphae and spores are evident in a pattern that is often described as “spaghetti and meatballs.” The differential diagnosis includes seborrhea, eczema, pityriasis rosea, and secondary syphilis. Seborrheic lesions are more frequently located on the central trunk, are more erythematous, and have thicker scales. With eczema, patients usually have more scaling, pruritus, and involvement of the extremities. Patients with pityriasis usually have a herald patch, more peripheral scale around border lesions, and confinement of lesions to the central trunk, and the lesions do not show hyphae on KOH prep. Secondary syphilis usually involves the hands and feet, and the lesions do not show hyphae on KOH prep. Topical antifungal therapy given for 2 weeks is the treatment of choice for patients with mild and limited disease. Virtually any topical antiyeast preparation can be used with cure rates exceeding 70% to 80%. Patients should be informed that the healing process continues after the treatment is complete. A return to normal pigmentation may take months after the completion of successful treatment. Oral medications are more convenient for patients with extensive disease and may also be more effective in patients with recalcitrant infection. Most oral antifungal agents, with the exception of griseofulvin or terbinafine, may be used. Additionally, ketoconazole 2% shampoo in a single application or daily for 3 days may be considered as an option for treatment, especially with mild infections.
|
34. The most likely diagnosis is
A) Pearly papule
B) Basal cell carcinoma
C) Molluscum contagiosum
D) Squamous cell carcinoma
E) Keratoacanthoma
View Answer
34. The answer is B. (Basal cell carcinoma) The clinical presentation of basal cell carcinoma (BCC) can be divided into the following three groups:
|
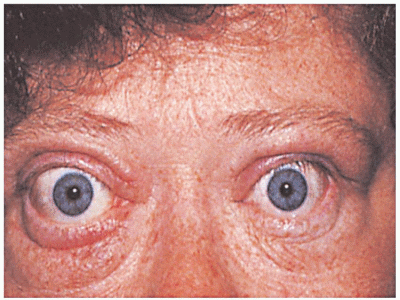
35. The eye findings pictured (at left) were seen in a 40-year-old woman who presented to the emergency room complaining of palpitations. The most likely diagnosis is
A) Scleroderma
B) Graves’ disease
C) Amyloidosis
D) Cushing’s disease
E) Lupus erythematosus
View Answer
35. The answer is B. (Graves’ disease




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree