a large part on secondary peristalsis, because the primary peristaltic wave moves too rapidly to propel solids in the esophageal body, thus passing over them and moving them only a small part of the esophageal length. Secondary peristalsis is the event that follows the primary peristaltic wave and initiates a powerful, initially static contraction that occurs directly around the boluses. Abnormalities in primary and secondary peristalsis need to be defined in patients with GERD, particularly in those for whom a surgical remedy may be sought.
The best methodology for evaluating secondary peristalsis is to abruptly insufflate 10 mL of air into the midesophageal body via the wide-core lumen of a manometric extrusion system. The motor response of the esophagus to this distention can then be evaluated.
The measurement of LES relaxation is of particular importance, not only in the early diagnosis of achalasia and the assessment of dysphagia after antireflux surgery but also to determine the appropriateness of LES contraction and relaxation. Water swallow-induced LES relaxation has a duration of 4.1 (3.0 to 5.4 range) seconds, with a mean nadir pressure of relaxation of 1.0 (0.2 range) mm Hg. Some conditions, such as achalasia or diffuse esophageal spasm, can be easily defined, but in some instances, only a nonspecific motor defect is evident. This somewhat vague term embraces individuals with “underpowered” peristalsis and results in the failure of development of an adequate propulsive force to clear the esophagus.
The identification of a manometric abnormality is important in helping define the cause of GERD or the failure of ing in a terminal sphincter (LES) relaxation. The progression of the waves over time demonstrates the progression of the descending esophageal peristaltic wave following a swallow of water. The LES (red) relaxes intermittently to allow passage of the bolus into the stomach.
Intraluminal pressures in the esophagus may be measured by either water-perfused manometric assemblies connected to external pressure transfusers or recording assemblies using intraluminal transfusers. The latter technique does not require water perfusion, which is an advantage but is expensive, fragile, and costly to repair. The perfused manometric assemblies are therefore most widely used, given their relatively low cost, easy maintenance, and reliable function. They consist of an extrusion with multiple fine channels, each of which opens sideways at the esophageal lumen at different levels, thus enabling recordings of pressure simultaneously at multiple levels. Using a lowcompliance manometric pump, each hole and its associated channel transmits pressure to an external transducer, enabling a pressure profile of the sphincteric zone and the area of interest to be developed. Because the LES has a maximal pressure zone that is only a few millimeters, positioning is of critical importance, especially given the fact that the LES moves approximately 10 cm each time a swallow occurs. The pull-through technique was previously used to precisely identify the pressure zones but is uncomfortable for the patient and involves repeated manipulation of the manometric assembly. For the most part, swallow-induced esophageal peristalsis is used to define the site of the LES and measure its function. A perfused sleeve of 6 cm in length provides reliable monitoring of both basal and swallow-induced changes of sphincteric pressure, because this length is adequate to accommodate the predictable movement of the LES relative to the manometric assembly. Primary peristalsis can be evaluated using 5-mL water boluses and provides information
that enables the termination of appropriate esophageal clearing. A peak threshold pressure of 33 mm Hg per mL is reached in the distal esophagus for reliable fluid transport by primary peristalsis. Esophageal transport of solids depends in reference in the form of a combination electrode. They are also the most durable of electrodes (can be chemically sterilized) and have a service life of approximately 100 studies. Their main disadvantages are their expense, fragility, and relative bulkiness. The result is that they are often difficult to pass and require extra care with handling. Indeed, nasal passage, particularly with combination electrodes, can often be difficult and uncomfortable. Antimony electrodes are cheaper than their glass counterparts, are smaller in size, and are more resistant to me>The best methodology for evaluating secondary peristalsis is to abruptly insufflate 10 mL of air into the midesophageal body via the wide-core lumen of a manometric extrusion system. The motor response of the esophagus to this distention can then be evaluated.
that enables the termination of appropriate esophageal clearing. A peak threshold pressure of 33 mm Hg per mL is reached in the distal esophagus for reliable fluid transport by primary peristalsis. Esophageal transport of solids depends in reference in the form of a combination electrode. They are also the most durable of electrodes (can be chemically sterilized) and have a service life of approximately 100 studies. Their main disadvantages are their expense, fragility, and relative bulkiness. The result is that they are often difficult to pass and require extra care with handling. Indeed, nasal passage, particularly with combination electrodes, can often be difficult and uncomfortable. Antimony electrodes are cheaper than their glass counterparts, are smaller in size, and are more resistant to me>The best methodology for evaluating secondary peristalsis is to abruptly insufflate 10 mL of air into the midesophageal body via the wide-core lumen of a manometric extrusion system. The motor response of the esophagus to this distention can then be evaluated.
The measurement of LES relaxation is of particular importance, not only in the early diagnosis of achalasia and the assessment of dysphagia after antireflux surgery but also to determine the appropriateness of LES contraction and relaxation. Water swallow-induced LES relaxation has a duration of 4.1 (3.0 to 5.4 range) seconds, with a mean nadir pressure of relaxation of 1.0 (0.2 range) mm Hg. Some conditions, such as achalasia or diffuse esophageal spasm, can be easily defined, but in some instances, only a nonspecific motor defect is evident. This somewhat vague term embraces individuals with “underpowered” peristalsis and results in the failure of development of an adequate propulsive force to clear the esophagus.
The identification of a manometric abnormality is important in helping define the cause of GERD or the failure of acid-suppressive medication to provide adequate relief and healing. In addition, it provides information necessary to confirm the need for a prokinetic agent. Under circumstances in which defined motor abnormality is evident, the use of surgery should be carefully considered, because wrap procedures performed under such circumstances may not function adequately. In individuals who meet the criteria for elective surgery based on demonstration of abnormal LES function, manometric evaluation is useful as a quantitative tool to evaluate efficacy of the surgery or alternatively define causes for its failure.
Esophageal pH monitoring
Esophageal pH monitoring is an important adjunct to clinical assessment and endoscopy in the diagnosis of GERD. Methods of esophageal pH monitoring have advanced substantially in the last decade. Better and more versatile recording equipment has been developed and is now widely marketed. Computers and purpose-designed software have extended the scope of interpretation of the recordings and made this process more time dependent.
In contrast to endoscopy or the Bernstein test, ambulatory esophageal pH monitoring records spontaneous reflux events and measures directly the degree of esophageal acid exposure, fundamental factors in the pathogenesis of this disease. Not surprising, therefore, is the regard by many that this is the gold standard for the diagnosis of reflux disease. However, as in any medical test, it
is not without limitations. There are both methodologic and inappropriate approaches to analysis and interpretations of the results.
is not without limitations. There are both methodologic and inappropriate approaches to analysis and interpretations of the results.
Equipment
The major components are the pH electrode, data recorder, and software. There are three main types of pH electrodes: glass, monocrystalline antimony, and ion-selective field effect transistor (ISFET) electrodes. The first two are the most widely used. Glass electrodes are distinguished by having a linear response over a pH range from 1.0 to 12.0 and are relatively drift free, particularly when used with an internal =”FIGURE-COL1″>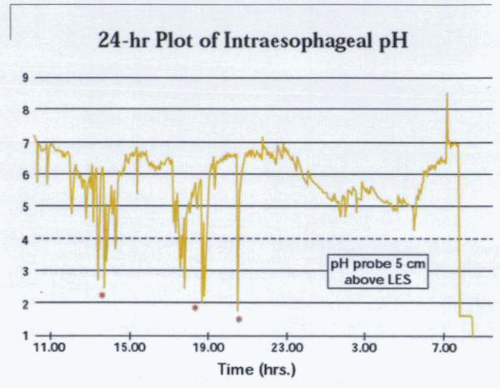
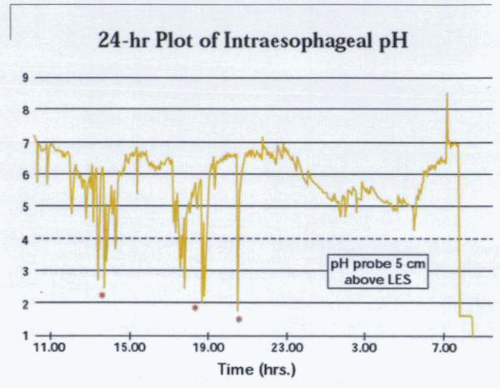
There is a clear relationship between esophageal mucosal damage, the hydrogen ion concentration, and the acid dwell time in the esophagus. Episodic reflux events are documented by a sudden drop in esophageal pH (*).
Analysis
There are two major considerations in the analysis of pH recordings: measurement of the amount of reflux and the relationship between the patient’s symptoms and reflux. Interestingly, these two issues are not necessarily related and rather appear often to be complementary aspects of the analysis and interpretation of pH recordings. Traditionally, reflux is thought to occur when esophageal pH falls below 4.0. This threshold is clinically relevant, because heartburn occurs at a pH of less than 4.0, and peptic activity diminishes rapidly above this level. Interestingly, it is common for buffering of gastric contents early in the postprandial period to lead to reflux of gastric contents with a pH of above 4.0. In addition, falls in pH that do not reach a pH of 4.0 can also be symptomatic, and in some circumstances (e.g., gastric resection), it may be appropriate to set the threshold above pH 4.0 or 5.0. The end of the reflux period is defined as the point at which esophageal pH rises above 4.0 (or 5.0); it is recommended that a minimum time (18 seconds) should elapse before a new reflux period is scored. Reflux events occurring at a pH of less than 4.0 are not currently identifiable but do not have an adverse impact on the clinical importance of pH monitoring. Shifts in esophageal pH to greater than 7.0 (alkaline pH events) have been interpreted as reflux of alkaline duodenal contents. However, more recent analysis has suggested that these may be as a result of swallowed saliva. Inclusion of such events in the final analysis is, therefore, potentially inappropriate. The duration of pH below 4.0, usually expressed as a percentage oiv class=”P”>It is not unusual for pH monitoring to be performed without the patient taking any antireflux therapy.
Before the study, H2 receptor antagonists and prokinetics should be stopped for 24 to 72 hours. pH monitoring, however, is flexible enough to assess the efficacy of antireflux treatment on esophageal physiology. Before beginning a study, the electrode should be calibrated in a neutral and acid buffer (pH less than 2.0) and again at the end to check for electrode drift. Glass electrodes




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


