Percutaneous Femoral-Popliteal Reconstruction Techniques: Reentry Devices
Danielle E. Cafasso
Peter A. Schneider
DEFINITION
Reentry devices facilitate true lumen reentry after subintimal recanalization for endovascular treatment of complex lesion morphologies and occlusions in the femoral-popliteal segment.
Subintimal recanalization and reconstruction of the femoral and popliteal arteries have diminished reliance upon femoral-popliteal bypass. Reentry into the true lumen can be challenging and is often the rate-limiting factor for the success of this procedure. Improved wires and support catheters, and also reentry devices, have been developed for crossing chronic total occlusions (CTOs).
Tools for managing CTOs are listed in Table 1. CTO support catheters may be used to support the guidewire that is being used to cross the occlusion. These typically have lubricious surface and a stiff tip. Distal access may be used to recanalize infrainguinal occlusions from a retrograde direction. Reentry catheters may be used to reenter the true lumen. CTO crossing catheters are not discussed in the chapter. These are relatively new and use either mechanized or hand power to manipulate through an occlusion in hopes of remaining in the true lumen.
Planning and performing subintimal recanalization and reentry into the true lumen of the femoral and popliteal arteries are described herein.
Table 1: Tools for Managing Chronic Total Occlusions in the Lower Extremity | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients with clinical symptoms and signs of lower extremity ischemia may benefit from subintimal recanalization and the use of reentry techniques in the course of their clinical care.
Patients present with claudication, rest pain, nonhealing ischemic ulcers, or gangrene. The history and physical examination is consistent with these lower extremity presentations and is described elsewhere in this atlas.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Patients who might benefit from subintimal recanalization and reentry typically have complex lesion morphology, such as arterial occlusion, that may be managed by creating a new channel outside of the potential space offered by the subintimal area. Imaging studies that define the anatomy and lesion morphology are useful prior to revascularization. This may include duplex scanning, magnetic resonance angiography, or computerized tomographic angiography. We usually perform duplex mapping prior to any lower extremity intervention. Long lesions, occlusions, and complex lesions are typically identifiable with preoperative imaging.
Patients with lower extremity ischemia should have objective physiologic confirmation of the degree to which perfusion is diminished. This may be accomplished by ankle-brachial indices or toe pressures.
SURGICAL MANAGEMENT
Preoperative Planning
Preoperative planning includes identifying the best access site for arterial entry. Subintimal recanalization of the femoral-popliteal segment may be performed using an up and over approach, from the contralateral common femoral artery, or using an antegrade approach from the ipsilateral common femoral artery. A reentry catheter may be used through either of these access choices. Preoperative noninvasive imaging is very helpful in making this plan for approach.
The location of lesion helps determine access site and approach. Many patients with superficial femoral artery (SFA) and/or popliteal artery disease are treated with an up and over approach. If the patient has inflow iliac artery disease or has an SFA lesion that begins near the origin of the SFA, an up and over approach is warranted. Reentry devices require placement of a 6-Fr sheath. If an up and over approach is anticipated, the aortic bifurcation should also be assessed to make sure that the reentry device can be passed.
Patients with extensive disease below the knee and without iliac or proximal SFA disease and who are not obese can be treated using an antegrade approach.
TECHNIQUES
RECANALIZATION STRATEGY
In managing complex lesions of the femoral and popliteal arteries, it is quite common to attempt to recanalize the true lumen. Stenosis can almost always be crossed transluminally using a wire supported by a catheter. A steerable, hydrophilic, low-profile wire is best. Long lesions, especially if occluded, may not be possible to cross in the true lumen. In this case, subintimal recanalization and reentry is the best option.
Strategy is based on selection of a reentry site where the artery has an acceptable lumen, collaterals can be preserved, calcification is avoided, and potential bypass sites remain intact. Staying in the true lumen when possible offers the shortest reconstruction and preservation of most collaterals. When subintimal passage is required, reenter the true lumen as close to the distal reconstitution as possible. The most common method of subintimal recanalization is using a loop of hydrophilic wire to dissect the subintimal space and the loop can also be used to reenter the true lumen.
There is typically a large incoming collateral feeding the reconstituted segment. If the reentry site is calcified, the success rate for loop passage is lower and use of a reentry catheter is more likely to be indicated.
If there is a substantial plaque at the intended reentry site, consider a site more distal than the initial reconstitution site. If there is another lesion distal to but near the reentry site, this can pose a challenge for passing the guidewire distally after it has popped into the true lumen.
The operator must decide in this case whether it would be appropriate to reenter distal to all the lesions, given that it might negatively affect bypass options. If the reentry fails and the patient needs a bypass, target sites for distal anastomosis should be anticipated, although failed reentry usually does not result in thrombosis of that segment.
TREATMENT PLATFORM
Sheath Placement
Place sheath tip close to the origin of the occlusion. Contrast administered through sheath fills the distal reconstitution site through collaterals. For an SFA occlusion, the tip of the sheath is usually positioned near the femoral bifurcation and the distal artery is visualized with contrast flowing through profunda collaterals. Use a sheath that is one size larger than that used for angioplasty and stenting, usually 7 Fr. This permits contrast administration even if a reentry device is being positioned (FIG 1).
Entering the Subintimal Space
Place an angled tip catheter pointing toward the artery wall at the origin of the occlusion. Point it opposite the location where the largest runoff collateral is located. Advance a Glidewire™ into the wall. Push it and the tip will catch and a loop will form (FIG 2).
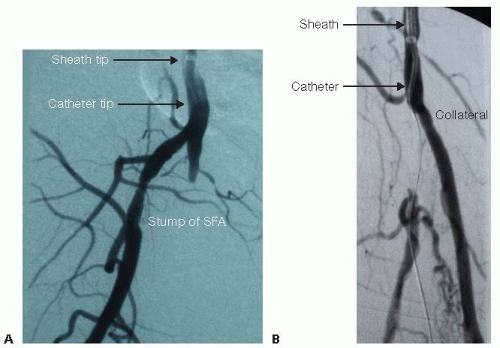 FIG 1 • Sheath placement. A. There is a stump of proximal SFA that is patent. The sheath was placed up and over the aortic bifurcation. The tip of the sheath is in the common femoral artery and can be recognized by a radiopaque tip. The catheter is used to direct the guidewire into the blind sac of the occluded proximal SFA. B. This arteriogram shows a short popliteal artery occlusion. The tip of the sheath is placed directly into the proximal popliteal artery to support the recanalization. There is a large perigenicular collateral that originates from the popliteal artery at the location where the artery occludes. Typically, the subintimal space is entered by directing the catheter tip and the guidewire to the arterial wall on the side opposite the origin of the large collateral.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|