Peptic Ulcer Disease
General
Although the incidence of peptic ulcer disease has steadily declined in the United States since the turn of the twentieth century, approximately 500,000 new cases and 4 million recurrences annually are reported. In 1990, it was estimated that the annual direct cost related to diagnosis and treatment of peptic ulcer disease in the United States was between 3 and 4 billion dollars, compared to the 2.5 million dollars estimated in 1975.
Duodenal ulcer is the major lesion in Western populations, whereas gastric ulcers are more frequent in Asian countries, particularly Japan. Japanese-Americans develop duodenal ulcers, showing that the frequency of gastric ulcers in Japan is due to environmental factors, not genetic constitution.
Although less prevalent than duodenal ulcer, gastric ulcer (0.1% of the population in developed countries) has a higher associated mortality and a greater morbidity resulting from hemorrhage, perforation, and obstruction. Frequent recurrence after healing has been a major component of the natural history of gastric ulcer, and without therapy, ulcers recur in 35% to 80% of the patients within 6 to 12 months of healing.
The advent of H. pylori eradication and appropriate acid-suppressive therapy in recent times has considerably narrowed the gap in therapeutic outcome between gastric and duodenal ulcers. The recognition that two of the major factors in defining gastric ulcer, namely H. pylori and NSAIDs, can be therapeutically addressed is mostly responsible for this advance. Therapy, therefore, for gastric ulcers has exhibited a remarkable transition, as PPI therapy combined with H. pylori eradication produced healing and recurrence
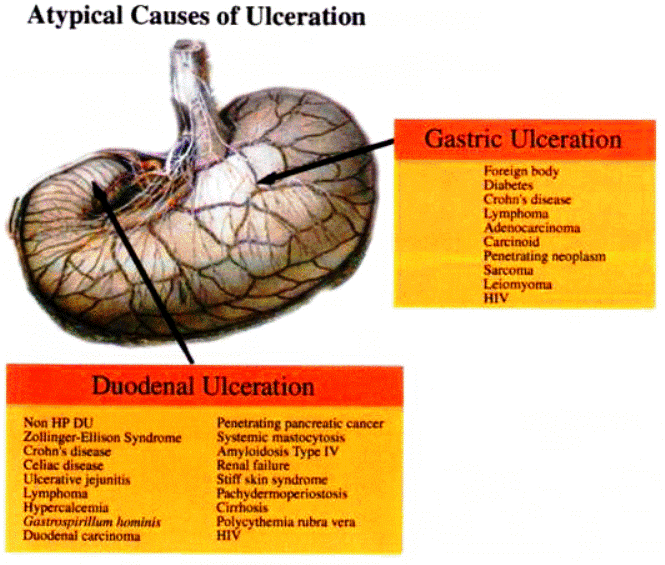
rates quite similar to those obtained with duodenal ulceration. Similarly, the recognition of NSAID involvement and the use of prophylaxis with acid suppressants or prostaglandins or withdrawal of the NSAID has further amplified healing rates. The introduction of curative therapy whereby H. pylori may be eradicated has been a further significant advance in eliminating the cause of gastric ulceration. The important caveat is that in all patients with gastric ulceration, an underlying neoplastic process should be considered and eliminated as a possibility. Multiple biopsies of the ulcer margin and rigorous histologic evaluation are critical to ensure that there is no delay in identifying an ulcer of malignant origin. Indeed, the failure of a gastric ulcer to heal in the face of a compliance with a curative regime (PPI therapy and H. pylori eradication) should be regarded as an alarm symptom or a sign suggestive of gastric neoplasia.
rates quite similar to those obtained with duodenal ulceration. Similarly, the recognition of NSAID involvement and the use of prophylaxis with acid suppressants or prostaglandins or withdrawal of the NSAID has further amplified healing rates. The introduction of curative therapy whereby H. pylori may be eradicated has been a further significant advance in eliminating the cause of gastric ulceration. The important caveat is that in all patients with gastric ulceration, an underlying neoplastic process should be considered and eliminated as a possibility. Multiple biopsies of the ulcer margin and rigorous histologic evaluation are critical to ensure that there is no delay in identifying an ulcer of malignant origin. Indeed, the failure of a gastric ulcer to heal in the face of a compliance with a curative regime (PPI therapy and H. pylori eradication) should be regarded as an alarm symptom or a sign suggestive of gastric neoplasia.
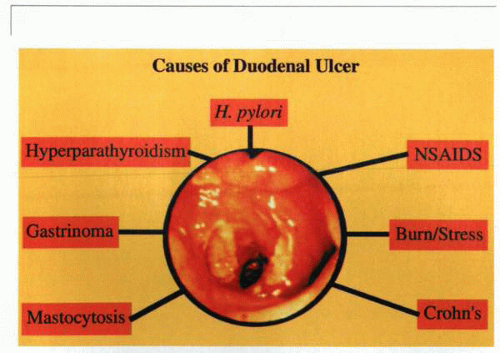 Despite the fact that H. pylori was unrecognized until 1983, it has in the last decade become regarded as the most common cause (85% to 95%) of all duodenal ulcers. |
In this context, the consideration of mucosal-associated lymphoid tumors (MALTs) should not be overlooked. Epidemiologic studies have concluded that H. pylori infection is the major cause of gastric cancer worldwide. The infection increases the risk of gastric adenocarcinoma by three to six times, probably by promoting the development of chronic atrophic gastritis. In addition, H. pylori increases the likelihood of the development of the primary non-Hodgkin’s lymphoma MALT by approximately sixfold. In the majority of circumstances, however, the eradication of H. pylori is associated with complete remission of this disease process.
The early introduction of appropriate therapeutic measures once a gastric ulcer has been diagnosed will likely lead to a cure rate in at least 90% of individuals. Ensuring that NSAID therapy is withdrawn and H. pylori are eradicated is mandatory in individuals who exhibit recurrence of ulceration. Under such circumstances, however, rigorous endoscopic reassessment by biopsy for the presence of neoplasia should be undertaken. In those individuals who experience a complication, such as hemorrhage, perforation, or obstruction, appropriate surgical intervention is necessary. Although bleeding gastric ulcers may be under-run with a suture, more often than not, they are better managed by appropriate tailored surgical resection. Perforation, which in the past used to mandate resection for management, is currently more often managed by repair of the defect followed by appropriate acid-suppressive and H. pylori eradication therapy. In some circumstances, anatomic considerations may mandate resection, particularly in ulcers close to the gastroesophageal junction on the lesser curve.
Chronic gastric obstruction, usually in the juxtapyloric region, usually mandates gastric resection with establishment of a Billroth II anastomosis. Overall, however, the picture of gastric ulcer disease as a difficult problem with a high level of complication often necessitating surgical intervention has declined significantly and has more and more begun to resemble duodenal ulcer as a pathologic process amenable to conservative medical therapy except in complicated circumstances.
Metaanalysis for predicting the degree of acid inhibition (elevation of pH for a given period of the day) showed that a mean intragastric pH of 3.0 for 18 hours per day provided an optimal healing for duodenal ulcer, indicating that
the duodenum was able to handle a significant pH load due to its ability to secrete HCO3−. Results of metaanalyses to predict healing of gastric ulcers as a function of pH have not been published. Still, current PPI therapy requires longer administration for healing of gastric, as compared to duodenal, ulcers, presumably because there is still wall acidity in the stomach impeding healing.
the duodenum was able to handle a significant pH load due to its ability to secrete HCO3−. Results of metaanalyses to predict healing of gastric ulcers as a function of pH have not been published. Still, current PPI therapy requires longer administration for healing of gastric, as compared to duodenal, ulcers, presumably because there is still wall acidity in the stomach impeding healing.
|
Pathogenesis
In the past, considerable attention had been directed to the role of acid in the generation of damage to the mucosa. Innumerable studies have correlated levels of acid secretion with ulceration. Pepsin had been noted as a cofactor in such pathology, but its precise role in the pathogenesis had been largely ignored in favor of a preoccupation with neutralizing or inhibiting acid secretion. Confounding factors, such as cigarette smoking, alcohol ingestion, and spicy foods, had been identified, but their precise involvement in mucosal damage remains controversial. The biology of the mucosa itself was not well understood. Cytoprotection had been proposed as a generic entity, embracing the concept of gastric mucosal defensive mechanisms. In broad terms, these were regarded as preepithelial, epithelial, and subepithelial. Each level was proposed to exhibit specialized properties that allowed the gastric epithelium to protect itself against the many noxious agents it was exposed to. A further philosophic entity entitled the mucosal barrier was conceived and variously considered to embrace the mucous bicarbonate barrier, specialized apical ion-transport systems, and tight junctions that provided an anatomic barrier for acid and pepsin diffusion.
The pathogenesis of peptic ulcer may best be viewed as representing a complex scenario involving an imbalance between defensive and aggressive factors, of which the most notable now appears to be H. pylori. Although mucosal restitution and the reestablishment of epithelial cell continuity independent
of cell proliferation is an important issue closely linked to the expression of growth factors and mucosal integrity, the elucidation of its precise role still remains to be defined. Nevertheless, mucosal integrity as constituted by a variety of mucosal defense mechanisms is an important issue and will be dealt with separately in Section 4, Chapter 1.
of cell proliferation is an important issue closely linked to the expression of growth factors and mucosal integrity, the elucidation of its precise role still remains to be defined. Nevertheless, mucosal integrity as constituted by a variety of mucosal defense mechanisms is an important issue and will be dealt with separately in Section 4, Chapter 1.
Although the subject of H. pylori is separately dealt with further on, in Section 7, it is worthy of brief comment at this point in the context of noxious agents affecting the gastric mucosa. Its identification in 90% to 95% of patients with duodenal ulcer and 60% to 80% of patients with gastric ulcer, as compared to 25% to 30% incidences in symptomatic control subjects, confirms its relevance in the genesis of mucosal ulceration. The prevalence of infection increases with age, and infection is more common in those with deprived socioeconomic circumstances. It is apparent that, in some countries, infection is not always involved with peptic ulceration. Such observations have raised the issue as to whether all types of H. pylori are of equal pathogenicity. Nevertheless, given the fact that the lifetime prevalence for duodenal ulcer is approximately 10% for men and 5% for women, the importance of H. pylori as a component of the disease process is substantial. The recognition that there exists a critical association between gastric metaplasia in the duodenal cap and H. pylori that appears to confer a predisposition to ulcer disease has been clearly identified. Similarly, strong evidence has accumulated to demonstrate an association between the eradication of H. pylori infection and the cure of peptic ulcer disease.
The production of NH3 by the urease of the organism may also explain part of the role of H. pylori in the generation of duodenal ulcer. It has been established that the majority of the urease activity of the organism is internal and acid activated. Activity reaches maximum at a pH of 6.0 and remains steady until a pH of 2.5. The toxicity of the NH4+ depends on entry of NH3 with a consequent increase in intracellular pH and release of calcium from stores in the endoplasmic reticulum and mitochondria. At gastric pH, the ratio of NH3 to NH4+ is low, but when at the neutral pH of the duodenum, the ratio rapidly rises, providing more NH3 for entry into duodenal cells. Thus, the load of NH3 to the duodenal cell may be a contributing factor to the generation of duodenal ulcers. This is discussed in more detail in the section on H. pylori.
pH and disease
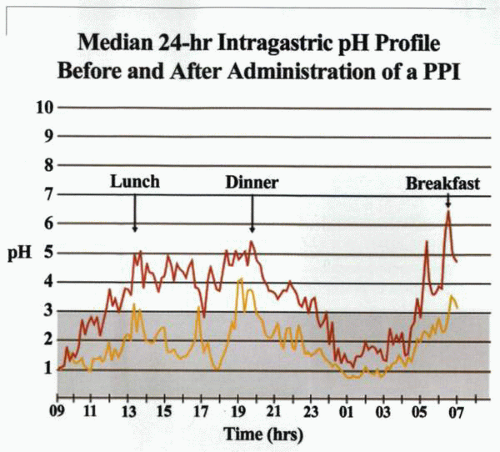
There is considerable overlap between 24-hour intragastric pH measurements in normal individuals and in those with duodenal ulcer. Nevertheless, there appears to be greater gastric acid secretion in duodenal ulcer patients than normal subjects, particularly at night. Overall, however, the 24-hour pH profile is not predictive of duodenal ulcer in an individual patient. The suppression of nocturnal acid secretion by H2 receptor antagonists proved effective in downregulating increased nocturnal acid secretion but is not essential to promote healing of a duodenal ulcer. Other factors, particularly duodenal bicarbonate secretion, have been proposed to be implicated in the genesis of duodenal ulceration. For the most part, however, duodenal mucosal bicarbonate
effects on luminal pH in the duodenal bulb may only be minor, because the overall secretory rate is in the range of 1 mmol per hour. Given the intermittent release of gastric chyme into the duodenum, a steep pH gradient exists between the terminal part of the pyloric antrum and the first part of the duodenum. When gastric pH values are below 4.0, the correlation between duodenal and gastric pH is linear, but this relationship disappears when the gastric pH is above 4.0; it is not possible to predict intraduodenal pH from intragastric pH during antisecretory therapy. Nevertheless, a series of metaanalytic studies of clinical trials that evaluated duodenal ulcer healing and pharmacodynamic studies of antisecretory drugs and acid suppression have revealed that healing rates for duodenal ulcer correlate with the suppression of gastric secretion. An evaluation of the pH profiles of individuals with ulcers in whom acid-suppressive therapy induced healing revealed three critical determinates predictive of duodenal ulcer healing. These were the degree of acid suppression; the duration of acid suppression within a 24-hour period; and the length of treatment. Thus, the healing rates for duodenal ulcer were demonstrated to be highly correlatable with the degree of acid suppression, and a daily intragastric pH of 3.0 for longer than 18 to 20 hours provided conditions that would achieve maximal healing rates for duodenal ulcers at 4 weeks. It was of interest that increasing acid suppression to an intragastric pH greater than 3.0 did not significantly improve healing. However, increasing the total duration of acid suppression by lengthening treatment or during the individual 24-hour period itself resulted in higher healing rates. It was also evident that the therapeutic effect of H2 receptor antagonists reflected their ability to suppress nocturnal acidity better than daytime acidity.
effects on luminal pH in the duodenal bulb may only be minor, because the overall secretory rate is in the range of 1 mmol per hour. Given the intermittent release of gastric chyme into the duodenum, a steep pH gradient exists between the terminal part of the pyloric antrum and the first part of the duodenum. When gastric pH values are below 4.0, the correlation between duodenal and gastric pH is linear, but this relationship disappears when the gastric pH is above 4.0; it is not possible to predict intraduodenal pH from intragastric pH during antisecretory therapy. Nevertheless, a series of metaanalytic studies of clinical trials that evaluated duodenal ulcer healing and pharmacodynamic studies of antisecretory drugs and acid suppression have revealed that healing rates for duodenal ulcer correlate with the suppression of gastric secretion. An evaluation of the pH profiles of individuals with ulcers in whom acid-suppressive therapy induced healing revealed three critical determinates predictive of duodenal ulcer healing. These were the degree of acid suppression; the duration of acid suppression within a 24-hour period; and the length of treatment. Thus, the healing rates for duodenal ulcer were demonstrated to be highly correlatable with the degree of acid suppression, and a daily intragastric pH of 3.0 for longer than 18 to 20 hours provided conditions that would achieve maximal healing rates for duodenal ulcers at 4 weeks. It was of interest that increasing acid suppression to an intragastric pH greater than 3.0 did not significantly improve healing. However, increasing the total duration of acid suppression by lengthening treatment or during the individual 24-hour period itself resulted in higher healing rates. It was also evident that the therapeutic effect of H2 receptor antagonists reflected their ability to suppress nocturnal acidity better than daytime acidity.
Diagnosis
The widespread recognition of symptomatology involving epigastric discomfort related to the ingestion of food and broadly grouped under the nomenclature of dyspepsia is well accepted as synonymous with evidence of acid peptic disease. Although considerable emphasis in the past had been placed on precise delineation of the symptomatology to determine whether the site of the ulceration is gastric or duodenal, currently, the identification of dyspepsia
rapidly leads to upper gastrointestinal endoscopy and the determination of the precise location of the lesion. Of particular relevance in the history should be the determination of alarm symptoms or signs such as weight loss, vomiting, the development of back pain, or failure to relieve symptomatology with acid-inhibitory therapy. Broadly speaking, the presence of such features would suggest either the development of a complicated ulcer (bleeding, penetration, perforation, stenosis, or neoplasia) or that the ulcer may be due to other causes, such as aspirin, NSAID intake, or a gastrinoma. These entities will be discussed separately in further detail.
rapidly leads to upper gastrointestinal endoscopy and the determination of the precise location of the lesion. Of particular relevance in the history should be the determination of alarm symptoms or signs such as weight loss, vomiting, the development of back pain, or failure to relieve symptomatology with acid-inhibitory therapy. Broadly speaking, the presence of such features would suggest either the development of a complicated ulcer (bleeding, penetration, perforation, stenosis, or neoplasia) or that the ulcer may be due to other causes, such as aspirin, NSAID intake, or a gastrinoma. These entities will be discussed separately in further detail.
The establishment of the diagnosis of acid peptic disease requires not only the identification and characterization of the site of the lesion but also the determination of the presence of H. pylori. This can be undertaken by a number of techniques, including histologic staining, urease identification in the biopsy material, serology, or breath or stool testing. The sensitivity and specificity of such tests are important criteria, although costs will probably be the dominant issue in determining how the organism should be identified.
Medical management
Duodenal ulcer
Ulcer healing and acid suppression
There is a direct correlation between the healing rate of duodenal ulcers and the degree of suppression of 24-hour intragastric acidity associated with the use of antisecretory agents. Hunt and his colleagues were the first to point out that a primary determinant of duodenal ulcer healing is represented by the fraction of the day for which intragastric pH is maintained above 3.0 as well as the duration of treatment itself. Using metaanalysis, they predicted that all duodenal ulcers could be healed within 4 weeks if intragastric pH were to be maintained above 3.0 for between 18 and 20 hours per day. In this respect, the PPI class of drugs has proved to be superior because they inactivate the H,K ATPase enzyme and produce inhibition of both peripherally and centrally mediated gastric acid secretion. On the contrary, the H2 receptor antagonists act via competitive antagonism at the H2 receptor on the basolateral membrane of the parietal cell to inhibit histaminemediated acid secretion. Such agents are therefore somewhat less effective in controlling food-stimulated gastric acid secretion, because cholinergic-mediated stimulation is not inhibited. Almost every clinical trial has demonstrated the superiority of PPIs over H2 receptor antagonists in the treatment of both gastric and duodenal ulceration. PPIs thus produce healing in a greater proportion of ulcers than do H2 receptor antagonists as well as faster healing and more rapid relief of symptoms. Apart from the personal advantages to the patient of the more rapid amelioration of the disease process, both the duration and cost of medical therapy can thus be decreased. A number of comparative studies have demonstrated that omeprazole heals duodenal ulcers faster and more effectively than do H2 receptor antagonists. Similarly, other studies have demonstrated that pantoprazole (40 mg daily) produces significantly higher rates of duodenal ulcer healing than does ranitidine when compared at both 2 and 4 weeks. In a separate series of studies, lansoprazole (30 mg daily) produced more rapid and effective healing of
duodenal ulcers than 300 mg of ranitidine administered at night. Other data have demonstrated that omeprazole (20 mg daily) resulted in significantly less daytime pain than that experienced by patients receiving 300 mg of ranitidine at bedtime. Studies comparing pantoprazole (40 mg daily) with ranitidine (300 mg daily) demonstrated that improvement of pain relief after 2 weeks was greater in patients receiving pantoprazole than in those receiving ranitidine. Similarly, lansoprazole has been shown to decrease ulcer pain more effectively than ranitidine, with a significantly greater percentage of patients free of symptoms after 2 weeks using the PPI as opposed to the H2 receptor antagonist.
duodenal ulcers than 300 mg of ranitidine administered at night. Other data have demonstrated that omeprazole (20 mg daily) resulted in significantly less daytime pain than that experienced by patients receiving 300 mg of ranitidine at bedtime. Studies comparing pantoprazole (40 mg daily) with ranitidine (300 mg daily) demonstrated that improvement of pain relief after 2 weeks was greater in patients receiving pantoprazole than in those receiving ranitidine. Similarly, lansoprazole has been shown to decrease ulcer pain more effectively than ranitidine, with a significantly greater percentage of patients free of symptoms after 2 weeks using the PPI as opposed to the H2 receptor antagonist.
Comparable observations of the use of acid suppression in gastric ulcer patients have been found. Omeprazole (20 mg daily) produced consistently higher rates of healing than did H2 receptor antagonists. Pantoprazole (40 mg daily) resulted in significantly higher healing rates of gastric ulcers than did ranitidine (300 mg daily) at both 4 and 8 weeks. Lansoprazole (30 mg daily) healed significantly more ulcers than did famotidine (20 mg twice daily). In addition, pantoprazole, omeprazole, and lansoprazole produced more rapid relief of symptoms in patients with gastric ulceration than did H2 receptor antagonists. In those individuals with peptic ulcers refractory to long-term treatment with H2 receptor antagonists, a number of clinical trials have demonstrated that pantoprazole, lansoprazole, and omeprazole are capable of generating effective healing.
H. pylori eradication
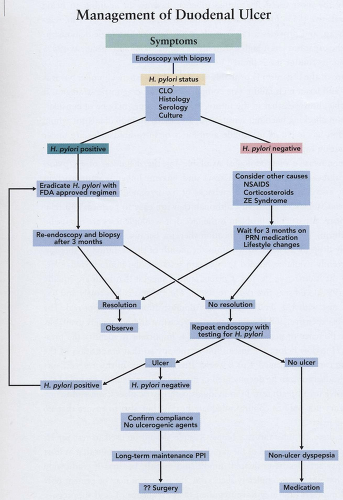
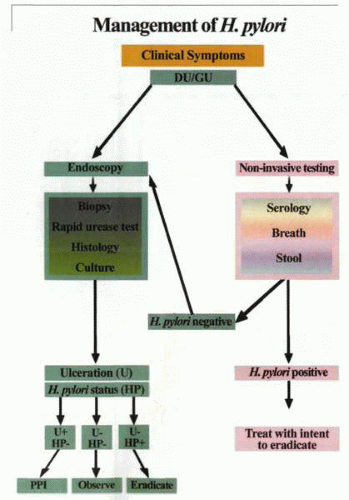
On determination of clinical symptomatology consistent with a putative diagnosis of peptic ulcer disease, the site and nature of the lesion should be identified. Thus, at endoscopy, the presence and site of the ulcer, as well as the
presence or absence of H. pylori, should be determined and documented. The diagnosis of H. pylori can be undertaken by the use of noninvasive or invasive tests. Invasive methodology involves endoscopy with gastric mucosal biopsy and either histology culture or rapid urease testing. The rapid urease test is probably the most useful in routine practice, because in addition to being highly sensitive (85% to 95%) and specific (98%), it is easy to perform, relatively cheap, and provides a rapid result. Although the histologic demonstration of the organism has a high sensitivity (85% to 90%) and specificity (93% to 100%), its routine use is limited by its high cost.
presence or absence of H. pylori, should be determined and documented. The diagnosis of H. pylori can be undertaken by the use of noninvasive or invasive tests. Invasive methodology involves endoscopy with gastric mucosal biopsy and either histology culture or rapid urease testing. The rapid urease test is probably the most useful in routine practice, because in addition to being highly sensitive (85% to 95%) and specific (98%), it is easy to perform, relatively cheap, and provides a rapid result. Although the histologic demonstration of the organism has a high sensitivity (85% to 90%) and specificity (93% to 100%), its routine use is limited by its high cost.
Culture of the organism is probably the ideal diagnostic technique, but it is difficult and has a high failure rate compared to other diagnostic strategies. It is probable, however, that in the future, H. pylori culture may be of considerable use in checking bacterial sensitivity, particularly in individuals for whom eradication has failed as macrolide antibiotics or nitro-imidazoles are under consideration for future therapy.
The noninvasive methodologies available for the diagnosis of H. pylori include radiolabeled urea breath tests and enzyme-linked immunosorbent serologic assays (ELISAs). The drawbacks of the serologic studies are related to the relative lack of sensitivity, although they are easy to perform and relatively cheap. A particular problem is the fact that serologic tests are not useful in monitoring the success of eradication therapy, because IgG and IgA titers may only drop by 20% to 50% within the month of the cessation of therapy. The currently available labeled urea breath tests are the nonradioactive 13C test and the radioactive 14C test. Current studies suggest that both are equally specific (99%) and sensitive (90% to 98%). The 14C test is less costly and has recently met with U.S. Food and Drug Administration (FDA) approval. The 13C test is expensive, and the equipment is expensive and not widely available.
In the presence of peptic ulcer disease, it is important to identify the presence of H. pylori before the institution of therapy so that eradication of the organism can be confirmed 4 to 6 weeks after treatment. In this respect, successful eradication can be documented in duodenal ulcer patients by use of the noninvasive urea breath test. In individuals with gastric ulceration, endoscopy is necessary not only to confirm adequate healing but also to ensure that no neoplasia exists.
Under these circumstances, a biopsy sample should be used to test for H. pylori, preferably by means of the rapid urease test. It is important that at least two biopsy samples be evaluated (fundic and antral), because if eradication therapy has not been completely successful, the organism may be present only in small numbers and may have migrated (a consequence of acid-suppressive therapy and the alteration of its ideal pH milieu) from its original site. In those patients who exhibit relapse or recurrence of symptomatology, the presence of H. pylori should be meticulously assessed.
Bismuth-based antimicrobial therapy
H. pylori has been demonstrated to be sensitive to a wide variety of antimicrobial agents, including macrolides, beta lactams, ketoconazoles, tetracyclines, gentamycin, rifampicin, nitrofuran, and some quinolones. Nevertheless, the use of any of these agents alone (monotherapy) has generally proved to
render suboptimal results, with eradication rates of approximately 20%. Clarithromycin, a macrolide antibiotic, is more acid stable than its counterpart, erythromycin, and is well tolerated, more effective, and has an eradication rate alone of greater than 50%. It is, however, clearly apparent that the use of more than one antibiotic has resulted in improved cure rates. The most commonly administered combinations include the classic bismuth triple therapy of bismuth, subsalicylate, or subcitrate and metronidazole in combination with amoxicillin or tetracycline (standard bismuth triple therapy). The use of this classic triple-therapy mode has limitations.
render suboptimal results, with eradication rates of approximately 20%. Clarithromycin, a macrolide antibiotic, is more acid stable than its counterpart, erythromycin, and is well tolerated, more effective, and has an eradication rate alone of greater than 50%. It is, however, clearly apparent that the use of more than one antibiotic has resulted in improved cure rates. The most commonly administered combinations include the classic bismuth triple therapy of bismuth, subsalicylate, or subcitrate and metronidazole in combination with amoxicillin or tetracycline (standard bismuth triple therapy). The use of this classic triple-therapy mode has limitations.
Evaluation of the two different combinations has demonstrated that triple therapy incorporating amoxicillin is significantly less effective than triple therapy that includes tetracycline, because amoxicillin is significantly less effective in eradicating H. pylori. A further important clinical issue is the relatively high rate of pretreatment resistance to metronidazole in some parts of the world. Patients taking less than 60% of their prescribed medication fail to achieve eradication rates greater than 70%. Alternatively, if greater than 60% of the prescribed medications is taken, eradication rates up to 95% may be expected. Because the bismuth triple-therapy regime requires the ingestion of up to 18 tablets daily, such compliance may become a serious issue. Adverse events may be predicted in between 25% and 30% of patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree