Pedicled Transverse Rectus Abdominis Myocutaneous Flap Breast Reconstruction
Dale Collins Vidal
Emily B. Ridgway
DEFINITION
All patients undergoing mastectomy, or those who have undergone a prior mastectomy, are potential candidates for breast reconstruction. The choice to have breast reconstruction is personal, and the options available for breast reconstruction are affected by an individual’s anatomy, weight, prior surgical procedures and radiation, and personal preferences. Each patient is unique and consideration must be made of their current breast size, goal breast size, and anatomic limitations.
The pedicled transverse rectus abdominis myocutaneous (TRAM) flap was first described by Hartrampf in the 1980s and remains the autologous “workhorse” of breast reconstruction. Diabetic patients, smokers, and patients with an elevated BMI or a pendulous panniculus have higher risk for flap failure.
PATIENT HISTORY AND PHYSICAL FINDINGS
A complete medical and surgical history is essential.
Prior comorbidities should be identified and the decision for preoperative anesthesia evaluation should be made.
Current related history must include cancer stage; BRCA status; and prior treatments including lumpectomy, biopsy, neoadjuvant chemotherapy, and radiation.
Accurate documentation of any prior abdominal, pelvic, cardiac, and groin surgery is necessary in order to evaluate the candidacy for a TRAM flap.
Current breast size, the patient’s goal for breast size, and the amount of abdominal tissue will also guide surgical planning and the need for a contralateral symmetry surgery.
Risks, benefits, and alternate therapies must also be reviewed with the patient including other autologous options (free and pedicled) and implant-based reconstruction options.
Anatomy
As with any surgical technique, a thorough working knowledge of the anatomy of the chest and abdominal wall and any variants is essential. The primary blood supply of the breast originates from internal mammary perforating branches. Secondary blood supply is received via perforating arteries from the lateral thoracic, pectoral, thoracic, and lateral intercostal arteries. Many of these vessels are injured during mastectomy and much of the mastectomy flap blood supply is compromised and relies on dermal and subcutaneous vessels running just deep to the dermis.
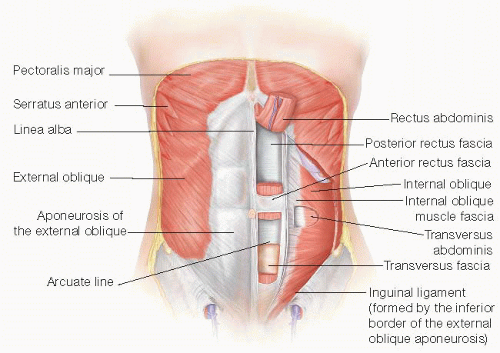
The abdominal wall is made of skin, varying thickness of subcutaneous adipose tissue, and an anterior rectus fascia overlying the paired rectus abdominis muscles (FIG 1).
Deep to the muscles is the posterior rectus fascia made up of the transversus fascia and internal oblique muscle fascia above the arcuate line and the transversus fascia below the arcuate line.
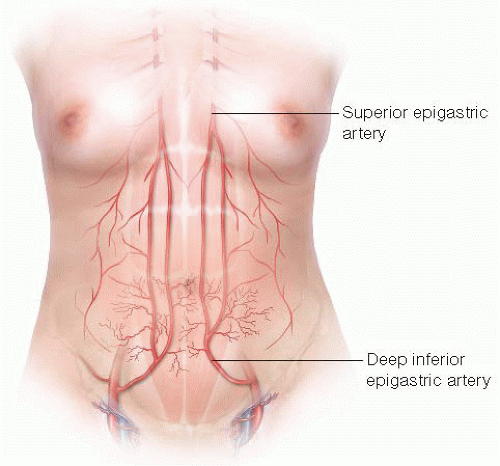
The paired rectus muscles originate from the pubic bone and extend to the cartilage of the 6th, 7th and 8th ribs. The blood supply comes from the dominant deep inferior epigastric artery and the superior epigastric artery (FIG 2).
Additional blood supply comes from the posterior perforating vessels accompanying the 8th through 12th intercostal neurovascular bundles.
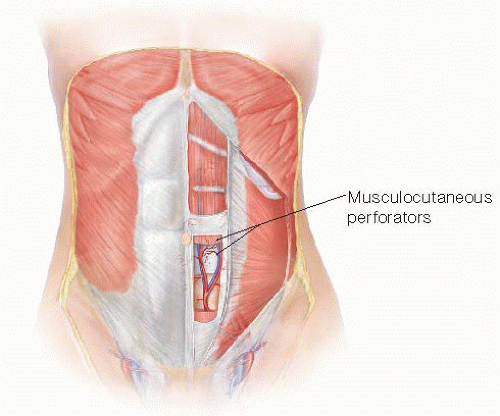
Within the muscle, the superior and inferior epigastric arteries may not have direct anastomoses under normal conditions. These connections are made or increased with surgical delay of the deep inferior epigastric artery. Musculocutaneous perforators pass through the muscle and anterior rectus fascia (FIG 3). They are often gathered in the periumbilical area and in mirrored medial and lateral rows of perforators. The medial and lateral row of perforators on a given side is separated by approximately 1.5 to 2 cm. In the case of the pedicled TRAM flap, the flap is based on the superior epigastric vessels.
SURGICAL MANAGEMENT
Preoperative Planning
For high-risk patients, ligation of the inferior epigastric artery (surgical delay) should be considered. Surgical delay of the inferior epigastric artery is performed 10 to 14 days prior to the mastectomy. This is often performed at the time of sentinel lymph node biopsy in order to limit events requiring anesthesia.
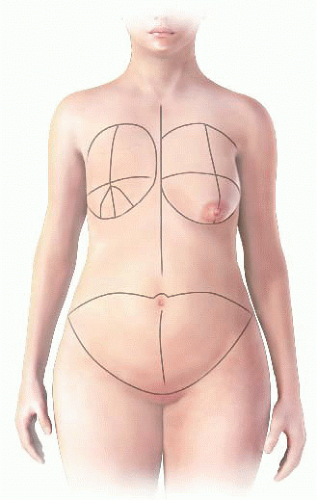
On the day of reconstruction, the patient is marked first in the standing position. At the breast, the inframammary fold (IMF), midline and a line 1 cm off the midline on either side, the lateral breast extension, and proposed or prior mastectomy skin incision approach are marked. The width of the proposed breast reconstruction is measured as this will guide the ideal width of the abdominal flap, which is particularly important in delayed breast reconstruction where there is often a paucity of breast skin (FIG 4).
On the abdomen, the midline is marked and an ellipse of skin including the umbilicus is marked. In our experience, all patients offer at least 13 cm in width of the ellipse and this can be assessed with a pinch test (FIG 4). The patient is then seated and any further extensions of the incisions are laterally marked to remove any “dog ear.”
TECHNIQUES
Perioperative antibiotics are provided and a Foley catheter and sequential compression device (SCD) boots are placed.
The flap can be raised while the mastectomy is being performed. No tumescence is used. The superior incision is made first, and the upper abdominal wall is raised to the level of the costochondral cartilages. On the side of the planned reconstruction, a tunnel is made through the IMF into the mastectomy pocket that fits a fist and the planned flap.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree