Parotidectomy
The parotid gland is divided into a superficial lobe and a deep lobe for the purposes of surgical dissection. Because 70% to 80% of the parotid tissue lies in the superficial lobe, most tumors, whether benign or malignant, arise in this lobe. Superficial lobectomy remains the standard treatment for small benign tumors. Simple enucleation is unwise, even when technically feasible, because even histologically benign tumors are likely to recur. A recurrent tumor is much more difficult to resect with preservation of the facial nerve and is more likely to be malignant.
SCORE™, the Surgical Council on Resident Education, classified this as a “COMPLEX” Head and Neck procedure.
STEPS IN PAROTIDECTOMY
Creation of incision and elevation of flaps
Identification of main trunk of facial nerve
Dissection in plane between superficial and deep lobe, preserving facial nerve branches (superficial parotidectomy)
Or: Dissection of deep lobe from around branches of facial nerve and ligation of parotid duct
HALLMARK ANATOMIC COMPLICATIONS
Partial facial paralysis resulting from facial nerve injury
Gustatory sweating (Frey’s syndrome) resulting from aberrant reinnervation
Patchy facial numbness resulting from damage to auriculotemporal nerve
LIST OF STRUCTURES
Parotid Gland and Associated Structures
Parotid gland
Superficial lobe
Deep lobe
Parotid duct
Superficial parotid lymph nodes
Parotid fascia
Deep cervical fascia
Nerves
Facial nerve
Temporofacial division
Temporal branches
Zygomatic branches
Buccal branches
Cervicofacial division
Marginal mandibular branch
Cervical branch
Great auricular nerve
Auriculotemporal nerve
Muscles
Masseter
Sternocleidomastoid
Digastric
Posterior belly of digastric
Platysma
Vessels
External carotid artery
Superficial temporal artery
Transverse facial artery
Maxillary artery
External jugular vein
Superficial temporal vein
Maxillary vein
Retromandibular vein
Facial vein
Landmarks
Lateral palpebral commissure (canthus)
External acoustic meatus
Mandible
Ramus of mandible
Zygomatic arch
Temporal bone
Tympanic portion
Mastoid process
Styloid process
Styloid vaginal process
Stylomastoid foramen
Atlas
Transverse process
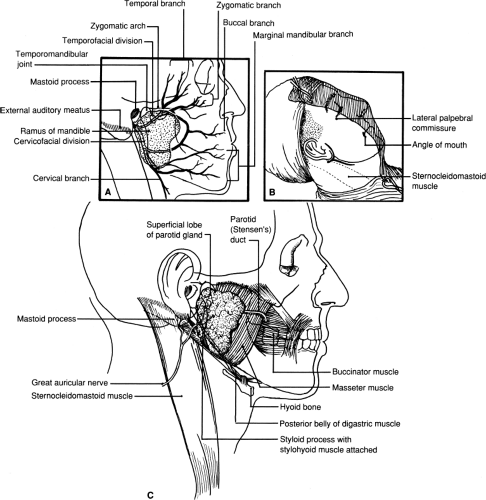
The safe performance of superficial parotidectomy involves careful identification and preservation of the facial nerve and its branches (Fig. 1.1A). Total parotidectomy is sometimes required when the deep lobe is involved. This procedure is briefly described in Figure 1.5. More complex problems, including reconstruction of branches of the facial nerve, are covered in the references at the end of this chapter. In this chapter, the anatomy of the parotid region is illustrated as it is demonstrated during the performance of parotidectomy.
There are three potential anatomic complications of parotid surgery. The first one, injury to the facial nerve or its branches, can be avoided by careful dissection as emphasized here. The second complication, gustatory sweating or Frey’s syndrome, appears to result from aberrant regeneration of nerve fibers divided, of necessity, during dissection. Several techniques have been proposed to prevent it, including interposition of a flap of sternocleidomastoid muscle or use of a bioprosthesis. This interposed material presumably acts as a barrier to nerve fiber regrowth. The third complication is the division of auriculotemporal nerve, which results in patchy numbness.
Positioning the Patient (Fig. 1.1)
Technical Points
Position the patient supine on the operating table. General anesthesia is preferred; however, avoid muscle relaxants,
so that nerve function can be assessed intraoperatively, if necessary. Place the operating table in a head-up position to improve exposure and minimize bleeding. Turn the head to the contralateral side and slightly hyperextend the neck to enhance exposure of the preauricular region. Place a cotton plug in the external ear to prevent blood accumulation within the external acoustic meatus and on the eardrum. Drape an operative field that includes the external ear and mastoid process, the neck, the angle of the mouth, and the lateral palpebral commissure of the eye. This allows you to observe motion of the angle of the mouth or eyelid in response to stimulation of facial nerve branches, which may assist in safe dissection.
so that nerve function can be assessed intraoperatively, if necessary. Place the operating table in a head-up position to improve exposure and minimize bleeding. Turn the head to the contralateral side and slightly hyperextend the neck to enhance exposure of the preauricular region. Place a cotton plug in the external ear to prevent blood accumulation within the external acoustic meatus and on the eardrum. Drape an operative field that includes the external ear and mastoid process, the neck, the angle of the mouth, and the lateral palpebral commissure of the eye. This allows you to observe motion of the angle of the mouth or eyelid in response to stimulation of facial nerve branches, which may assist in safe dissection.
Plan the preauricular skin incision so that it lies in a skin fold (Fig. 1.1B). Draw an incision in the skin fold anterior to the ear and extend the line of incision along the inferior margin of the mandible anteriorly. This incision provides adequate exposure to the area, can be extended if necessary, and lies in an inconspicuous position behind the mandible. Extend the incision posteriorly in an inverted T to provide additional exposure in difficult cases. Deepen the incision through the platysma muscle and achieve hemostasis with electrocautery.
Anatomic Points
The parotid region is bounded anteriorly by the mandibular ramus, posteriorly by the tympanic part of the temporal bone and the mastoid process, and superiorly by the external acoustic meatus, zygomatic arch, and temporomandibular joint (Fig. 1.1C). The deep structures in this region include the styloid process and, more inferiorly, the transverse process of the atlas. The gland overlies portions of the surrounding masseter muscle, the sternocleidomastoid muscle, and the posterior belly of the digastric muscle.
The parotid is enclosed in a sheath derived from the superficial (investing) lamina of deep cervical fascia. Branches of the great auricular nerve (the largest sensory branch of the cervical plexus, with fibers derived from C2 and C3), part of the platysma muscle, and a variable number of superficial parotid lymph nodes (draining the auricle, external acoustic meatus, eyelids, and frontotemporal region of the scalp) are superficial to the gland.
Elevation of Flaps to Expose the Parotid Gland (Fig. 1.2)
Technical Points
Elevate flaps in the plane just superficial to the dense superficial parotid fascia. Use skin hooks or fine-pointed rake retractors to exert upward traction on the skin flap because the plane is developed between subcutaneous tissue and superficial parotid fascia by sharp dissection. Identify the main trunk of the great auricular nerve and preserve it. Branches from the great auricular nerve will enter the substance of the parotid gland and must be divided. Divide the posterior facial vein, but preserve the retromandibular vein to avoid venous engorgement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree