Parathyroidectomy
Samuel M. Maurice
Geeta Lal
Introduction
In experienced hands, parathyroidectomy is >95% successful in curing hyperparathyroidism. Hyperparathyroidism may result from the overactivity of one gland, as in the case of a parathyroid adenoma or rarely parathyroid carcinoma, or it may result from the overactivity of multiple glands, as in the case of diffuse hyperplasia or multiple adenomas. The goal of parathyroidectomy is to remove all abnormal glands or, in the case of diffuse hyperplasia, to leave only a small remnant of parathyroid tissue.
The gold standard operation for hyperparathyroidism is a bilateral neck exploration, which entails identification of all parathyroid (PTH) glands. Advances including localization studies, use of intraoperative PTH assays, and endoscopic techniques have allowed for less invasive and more focused explorations. This chapter will focus on the standard, formal four-gland exploration. Various minimally invasive techniques in use will also be briefly discussed.
Steps in Procedure
Standard Four-gland Exploration
Ligate middle thyroid vein and retract gland medially
Identify and preserve recurrent laryngeal nerve
Identify both parathyroids on both sides before biopsy or resection
Superior parathyroid glands commonly found dorsal to recurrent laryngeal nerve and posterior to the upper thyroid capsule
Inferior parathyroid glands commonly found anterior to recurrent laryngeal nerve near lower thyroid pole and thyrothymic ligament
If single adenoma—resect
If multiglandular disease—subtotal parathyroidectomy or autotransplantation
Focused Exploration or Reoperation
Consider lateral incision for reexploration
Proceed as guided by ultrasound, radioisotope, or serum levels
Close without Drains
Hallmark Anatomic Complications
Hypoparathyroidism
Recurrent hyperparathyroidism
Injury to recurrent laryngeal nerve
Bleeding
List of Structures
Adult Structures
Parathyroid glands
Superior parathyroid glands
Inferior parathyroid glands
Thyroid gland
Middle thyroid vein
Inferior thyroid artery
Superior thyroid artery
Recurrent laryngeal nerve
Thymus
Thyrothymic ligament
Mediastinum
Cricoid cartilage
Thyroid cartilage
Esophagus
Tracheoesophageal groove
Embryologic Structures
Pharyngeal pouch III
Ventral wing
Dorsal wing
Pharyngeal pouch IV
Ventral wing
Dorsal wing
Patients should be suitable candidates for general anesthesia. Patients with marked hypercalcemia (i.e., calcium levels higher than 12.5 mg/dL) or with marginal renal function should be well hydrated. Some patients may also benefit from the administration of furosemide, bisphosphonates, or calcitonin. Correct any electrolyte abnormalities. Document vocal cord function by direct or indirect laryngoscopy in those already suspected of having vocal cord dysfunction (i.e., those with prior neck surgery or altered phonation), because bilateral injury may lead to airway obstruction.
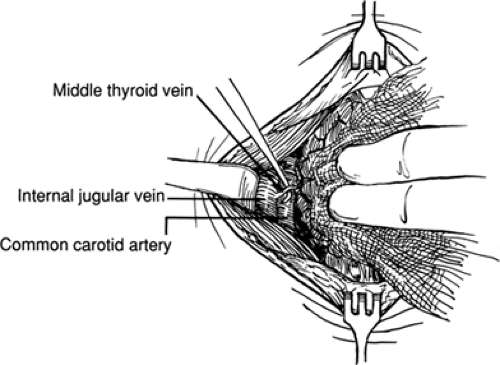
Initial Exposure of PTH Glands (Fig. 7.1)
Technical Points
Position the patient with neck extended on a donut cushion with a bean bag beneath the shoulders in a modified “beach-chair” position. Make an incision approximately 1 cm below the cricoid cartilage and carry this through the subcutaneous tissues and platysma. Develop subplatysmal flaps superiorly to the thyroid cartilage notch and inferiorly to the suprasternal notch using electrocautery. After placing a self-retaining retractor, divide the strap muscles in the midline and mobilize them off the thyroid gland (see Figs. 6.2, 6.3, 6.4 and 6.5 and accompanying discussion).
Dissect the sternothyroid muscle off the thyroid and prethyroidal fascia by blunt and sharp dissection. Then retract the strap muscles laterally to expose the middle thyroid vein. Ligate and divide this vein and retract the thyroid lobe medially. Sometimes, several branches, rather than one middle thyroid vein, are encountered. These branches may be similarly ligated and divided. A Kitner or 2-0 silk suture placed in the surface of the thyroid gland may be used to help retract the thyroid gland medially. Develop the space between the thyroid gland and carotid sheath bluntly or with gentle sharp dissection. Identify and protect the recurrent laryngeal nerve, using a neurostimulator if desired.
Most PTH glands are found within 1 cm of the junction of the inferior thyroid artery and the recurrent laryngeal nerve. The superior PTH glands are usually found dorsal to the recurrent laryngeal nerve and posterior to the upper thyroid capsule. The inferior PTH glands are usually located anterior to the recurrent laryngeal nerve near the lower thyroid pole and thyrothymic ligament. Location of glands can vary widely, reflecting differences in degree of embryologic migration and extent of displacement as glands enlarge. Any fat lobule at a typical PTH gland location could be harboring a PTH gland. A fine, curved Jacobsen hemostat and a scalpel can be used to incise the fascia overlying a suspicious fat lobule allowing an underlying PTH gland to come into view. A Kitner may also be used to gently dissect in the space between the carotid sheath and the thyroid gland. This gentle dissection often causes an underlying PTH gland to come into view, the so-called “float sign.”
After identification of the PTH glands on one side, the exploration should be continued on the contralateral side. When glands on one side are located in their normal position, the contralateral gland is usually located in a similar position. Contralateral symmetry is observed 80% of the time with superior PTH glands and 70% of the time with inferior PTH glands. Ideally in a four-gland exploration, all PTH glands are identified before removing any PTH tissue. During thyroidectomy, vessels are dissected and ligated on the surface of the thyroid gland (extrathyroidal dissection). However, during parathyroidectomy, the dissection is carried out more laterally to facilitate identification of the PTH glands and avoid inadvertent devascularization. As in the case of thyroidectomy, careful dissection and meticulous hemostasis are essential.
Anatomic Points
The middle thyroid vein is varied and is present in only about half of patients. The vein drains into the ipsilateral internal jugular vein after traveling superficial to the common carotid artery. Division of the middle thyroid vein or veins allows mobilization of the thyroid gland medially. This allows exposure of the space between the thyroid gland and the carotid sheath (containing the carotid artery, internal jugular vein, and vagus nerve). This space contains the recurrent laryngeal nerve, the inferior thyroid artery, and the PTH glands.
Normal PTH glands are golden yellow to light brown in color. The color does vary depending on the fat and oxyphil cell content of the gland and on the gland’s vascularity. Each gland generally weighs between 40 and 50 mg and is 3 to 7 mm in size. The PTH glands usually derive their blood supply from branches of the inferior thyroid artery, but branches of the superior thyroid artery supply approximately 20% of superior glands.
Most patients (approximately 84%) have four glands, 13% have more than four glands, and 3% have fewer than four glands. The bilateral superior PTH glands are usually superior and dorsal to the intersection of the inferior thyroid artery and the recurrent laryngeal nerve. The bilateral inferior PTH glands are usually inferior and ventral to the intersection.
PTH glands are generally soft and molded by their anatomic position. Distinguishing between a normal and hypercellular gland is often difficult. Generally, hypercellular glands are
larger in size (i.e., >7 mm) and generally darker, firmer, and more vascular. An intraoperative density test may prove useful. Hypercellular glands tend to sink when submersed in a saline solution, whereas normal glands usually float. No single characteristic is 100% reliable in distinguishing normal from hypercellular glands. The PTH surgeon must therefore rely on a combination of factors; this gestalt recognition favors the well-trained and experienced eye.
larger in size (i.e., >7 mm) and generally darker, firmer, and more vascular. An intraoperative density test may prove useful. Hypercellular glands tend to sink when submersed in a saline solution, whereas normal glands usually float. No single characteristic is 100% reliable in distinguishing normal from hypercellular glands. The PTH surgeon must therefore rely on a combination of factors; this gestalt recognition favors the well-trained and experienced eye.
Identification of the Superior PTH Glands (Fig. 7.2)
Technical Points
The superior PTH gland generally resides at the posterior aspect of the thyroid lobe approximately 1 cm superior to the intersection of the inferior thyroid artery and the recurrent laryngeal nerve (Fig. 7.2A). The gland is often found within a
globule of fat. Careful dissection with a Jacobsen or right angle clamp of the fascial layers covering the gland usually aids in identification. Gentle probing with a Kitner often causes the gland to pop into view (the so-called “float sign”). If differentiation between a fat lobule and gland is still in question, a fine scissors or scalpel can be used to cut a small piece from the nonhilar aspect of the gland. A PTH gland diffusely oozes from its cut surface where fat generally bleeds from distinct small blood vessels. The sample of tissue obtained can also be sent for frozen section analysis if there is still a question.
globule of fat. Careful dissection with a Jacobsen or right angle clamp of the fascial layers covering the gland usually aids in identification. Gentle probing with a Kitner often causes the gland to pop into view (the so-called “float sign”). If differentiation between a fat lobule and gland is still in question, a fine scissors or scalpel can be used to cut a small piece from the nonhilar aspect of the gland. A PTH gland diffusely oozes from its cut surface where fat generally bleeds from distinct small blood vessels. The sample of tissue obtained can also be sent for frozen section analysis if there is still a question.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree