Parathyroid Gland: Diagnosis and Margins
 Parathyroid hyperplasia usually involves all 4 glands but can be asymmetric with marked variation in the extent of glandular involvement (pseudoadenomatous variant). Adenomas are usually solitary. |
SURGICAL/CLINICAL CONSIDERATIONS
Goal of Consultation
Confirm a parathyroid gland has been biopsied or resected
Confirm parathyroid disease
Change in Patient Management
After removal of parathyroid gland(s) or biopsy confirmed, additional surgery is not necessary
Differentiation of adenoma, primary hyperplasia, and normal parathyroid may be used to guide surgery
In rare cases, confirmation of parathyroid carcinoma can guide completion of surgery
Clinical Setting
Primary hyperparathyroidism
Patients usually present with elevated parathyroid hormone (PTH) and hypercalcemia as detected by serum levels
Less commonly, patients present with symptoms of osteoporosis or renal calculi
85% have solitary adenoma
Primary hyperplasia involving multiple glands is less common
Surgery continues until adenoma has been removed
In cases of primary hyperplasia, multiple glands are removed
Imaging techniques with sestamibi can identify > 90% of adenomas
Useful to identify adenomas in unusual locations
Less useful to detect multiple hyperplastic glands
Single enlarged gland is removed
Remaining glands are inspected to ensure they are normal in size
Frozen section has been replaced by intraoperative PTH assays in some places
If serum level of PTH decreases by > 50% after removal of adenoma, further surgery is not necessary
Secondary hyperparathyroidism
Parathyroid glands become enlarged and hyperplastic in response to low calcium levels
Most commonly due to renal failure
Causes debilitating loss of calcium from bones
Usually 3 parathyroid glands will be removed while 1 gland is partially resected
Frozen section confirms identification of all 4 removed glands
Surgery for thyroid resection or neck exploration
Parathyroid glands may be resected inadvertently
Practical Considerations in Parathyroid Intraoperative Consultation
Parathyroid glands can be difficult for surgeon to identify
Normal glands are very small
Location and number of glands can vary
15% are found in unusual locations
Lymph nodes, thymic tissue, thyroid nodules, and other areas of nodular tissue may resemble glands grossly
Frozen section is necessary to definitively identify tissue as parathyroid
Tissue is assessed as normal or abnormal
Disease involving gland should be diagnosed when possible
SPECIMEN EVALUATION
Gross
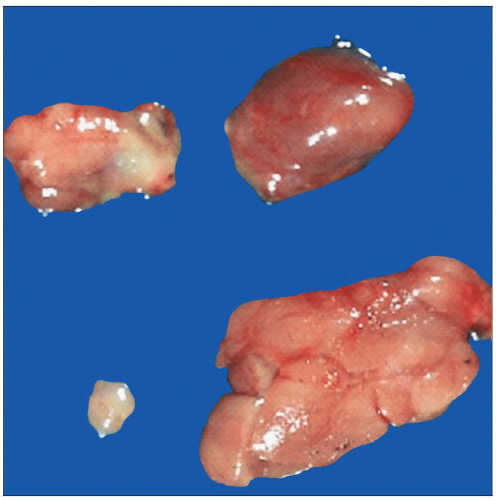
Specimen is identified as biopsy or resection of entire gland
Parathyroid gland is ovoid and has smooth glistening surface
Size and weight are measured and are important parameters to identify and document abnormal glands
Normal parathyroid gland is size and shape of kidney bean (4-6 mm × 2-4 mm), 20-40 mg each
Most people have 4 parathyroid glands, 10% have ≥ 5, and 3% have < 4
Adenoma: Single enlarged gland, usually 0.2 to > 1 g, tan to red-tan, encapsulated, ± rim of normal parenchyma
Hyperplasia: Multiple enlarged glands
Biopsies are small irregular fragments of tissue
Frozen Section
Representative section of a complete gland is frozen
Biopsies are completely frozen
Cytology
Usually helpful when used in combination with frozen section
Highest sensitivity and specificity for correctly identifying parathyroid tissue
However, as a single test, frozen section alone is superior to cytological preparations
Useful to differentiate parathyroid cells from thyroid follicular cells
However, cytological preparations tend to yield many bare nuclei and lack architectural features that are helpful in identifying parathyroid tissue
Special Stains
Oil red O
Parenchymal cells in normal glands contain a large amount of intracytoplasmic lipid droplets
Intracellular and extracellular parenchymal lipid content is decreased to absent in hyperfunctioning parathyroid cells
Rim of normocellular parathyroid can be highlighted by this stain, confirming diagnosis of parathyroid adenoma
Other stains may be used to evaluate fat during intraoperative consultations
Sudan IV, osmium carmine, and air-dried slides stained with Wright-Giemsa stain
Not commonly used
MOST COMMON DIAGNOSES
Normal Parathyroid Glands
Normal size
4-6 mm × 2-4 mm × 0.5-2 mm
Normal weight
Men: 30 ± 3.5 mg
Women: 35 ± 5.2 mg
Any gland > 60 mg is enlarged
Normal parathyroid glands can show significant variation in cellularity, even in a single individual
Age, gender, constitutional factors (body fat, etc.) affect cellularity of normal parathyroid
Normal parathyroid cellularity distributed unevenly, high in infants and children, decreases with age
Adipose tissue
Stromal fat constitutes 10-30% of parathyroid
Increases with age
Not a reliable feature to distinguish normal glands from adenomas or hyperplasia
More stromal fat in polar regions of parathyroid than central
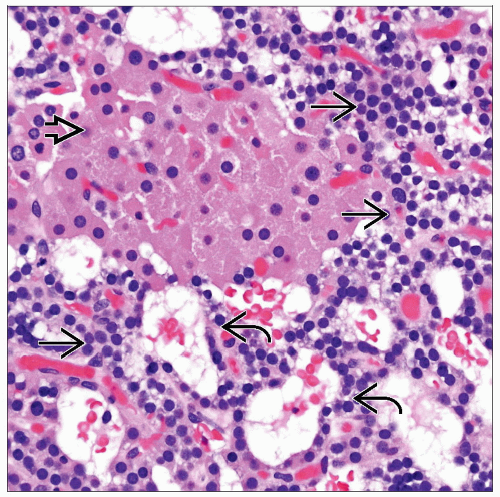
Parathyroid Adenoma
˜ 85% of surgical cases are to resect an adenoma
Excision of adenoma is curative and should result in immediate decrease in circulating PTH
If PTH is not decreased, 2nd adenoma may be present
Majority (˜ 96%) of adenomas are solitary
Rare cases of ≥ 2 adenomas can occur
Size: 1-3 cm
Weight: 300 mg to several grams
Light tan color
Thyroid tissue is dark red
Usually < 5% adipose tissue
However, some adenomas do have intracellular fat and adipose tissue
Cystic change can occur in large adenomas
Spontaneous infarction may result in adjacent inflammatory changes and adherence to surrounding tissue
Scattered cells with marked nuclear atypia may be present
Not a diagnostic feature of malignancy
Normal-appearing parenchyma may be seen compressed to 1 side in ˜ 50%
Rarely located completely within thyroid gland
Rarely associated with genetic syndromes such as hyperparathyroidism-jaw tumor syndrome (HPT-JT) and familial hypercalcemic hypercalciuria
Parathyroid Adenoma Variants
Parathyroid microadenoma: Weight < 0.1 g
Oxyphil parathyroid adenoma: Composed of > 90% mitochondria-rich oncocytes
Water clear cell parathyroid adenoma: Composed of cells with extensively vacuolated clear cytoplasm
Parathyroid lipoadenoma: Composed of abundant adipose tissue with scattered nests of parenchymal chief cells
Ectopic parathyroid adenoma: Located at abnormal sites
Intrathyroidal, mediastinum, thymus, soft tissue behind esophagus and pharynx
Predominantly macropseudofollicular growth pattern with colloid-like material are relatively common in parathyroid adenomas
This pattern may mimic thyroid follicles
Cystic parathyroid adenoma
Varying degrees of cystic change can be seen in parathyroid adenomas
Particularly common in larger parathyroid adenomas
Associated with hyperparathyroidism-jaw tumor syndrome
HPT-JT is an autosomal dominant disorder caused by inactivating mutations in HRPT2 tumor suppressor gene that encodes parafibromin
Secondary Hyperplasia
All 4 glands are usually enlarged, but enlargement may not connote level of involvement
Each, some, or all 4 glands may be multinodular
Asymmetric enlargement can resemble an adenoma or adenomas (pseudoadenomatous variant)
Nodular growth pattern is usually seen in parathyroid hyperplasia
Cell populations can consist of multiple types with nodules of chief cells, oxyphil cells, and clear cells
Scattered fat cells are usually present
Adipose tissue may be decreased and rarely absent
Oil red O or other stains for fat show diminished staining in most cases
It may not be possible to distinguish an adenoma from hyperplasia if only 1 gland is examined and clinical history is not provided
3 glands are removed
4th gland is biopsied to ensure parathyroid tissue has been identified and left in situ
Primary Hyperplasia
Very rare
1-4 glands may be enlarged
20% of patients will have a multiple endocrine neoplasia (MEN) syndrome
Generally MEN1 or MEN2A
Thyroid Lesion
Often show follicular growth, which can be seen in some parathyroid adenomas
Sometimes ectopic nodule of multinodular hyperplasia may grossly mimic a parathyroid gland
Thyroid tissues and neoplasms often
Have colloid and calcium oxylate crystals (highlighted by polarization)
Lack intracytoplasmic lipid and well-defined cytoplasmic membranes of parathyroid tissue
Atypical Parathyroid Adenoma
Noninvasive parathyroid neoplasm composed of chief cells with variable oncocytes, transitional cells, and water-clear cells with some features of parathyroid carcinoma
Adherence to adjacent structures
Mitotic activity
Fibrosis
Trabecular growth
Tumor cells in capsule
No definitive invasion
No invasion into adjacent structures
No capsular invasion
No vascular invasion
No perineural invasion
Parathyroid Carcinoma
Majority are functional and cause hyperparathyroidism
Parathyroid carcinoma usually necessitates en bloc resection
En bloc resection is necessary because carcinomas adhere to/infiltrate adjacent tissues
Removed with attached skeletal muscle and adjacent thyroid
Specimen should be inked and margins evaluated
Invasion into adjacent structures, vessels, perineural space
Very rare (˜ 2% of cases)
Usually in older adults (4th-6th decades)
Generally large: 2-6 cm, over 40 grams
Histologic features
Monotonous or trabecular growth, prominent nucleoli, high nuclear to cytoplasmic ratios are frequently identified
˜ 2/3 have marked nuclear pleomorphism present throughout carcinoma
Thick capsule that may be invaded
Numerous mitoses
Necrosis
Lymphovascular or perineural invasion
Dense fibrous bands
Fibrosis and fibrous bands but can be seen in both parathyroid adenoma and carcinoma
Metastatic Carcinoma
Rarely identified during life
Autopsy studies show up to 12% of patients with known cancer have parathyroid involvement
Metastases are usually from breast, prostate, liver, lung, and hematolymphoid malignancies
Also may be involved from direct extension from a thyroid tumor or head and neck neoplasm
Immunohistochemistry studies are very helpful to confirm primary site
REPORTING
Frozen Section
Document that parathyroid tissue is present
If entire gland has been removed, size and weight are reported
Report if ≥ 1 gland(s) are hypercellular
% of adipose tissue should be reported
Specific diagnosis of adenoma or hyperplasia is not necessary and is often not possible
If single gland is enlarged and if rim of normocellular parathyroid, diagnosis of adenoma may be rendered
Presence or absence of intracellular and extracellular lipid on oil red O stain (when used)
Cytology
Reported in conjunction with gross and frozen section findings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree