Pancreatic Resections
James J. Mezhir
This chapter discusses distal (left) pancreatectomy and pancreaticoduodenectomy (Whipple procedure). Because of the close anatomic proximity of the body and tail of pancreas to the splenic vessels, splenectomy is generally performed when the tail of the pancreas is resected for treatment of malignant disease. When this operation is performed for benign tumors, trauma, or highly select cancer cases, it is possible to preserve the blood supply of the spleen. The laparoscopic approach to distal pancreatectomy is described in Chapter 85e.
Resection of the head of the pancreas (pancreaticoduodenectomy) can be performed with or without pylorus preservation. References at the end of the chapter give additional details about total pancreatectomy and central pancreatectomy which are beyond the scope of this chapter.
For patients with pancreatic cancer, high quality contrast-enhanced imaging for staging is essential to prevent unnecessary laparotomy in these patients. Diagnostic laparoscopy is used selectively—in general those with any concern for M1 disease, body and tail lesions, and elevated Ca 19-9 (greater than 140 U/mL).
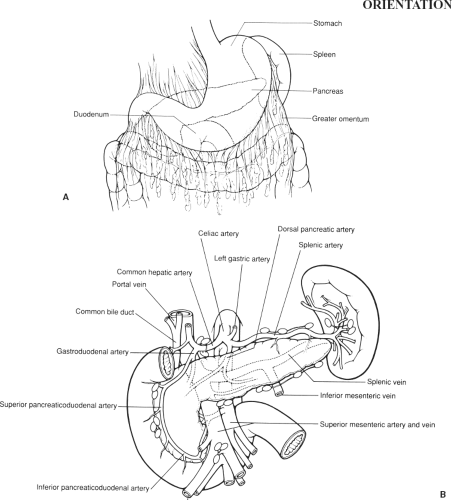
The regional anatomy is shown in Figure 84.1.
SCORE™, The Surgical Council on Resident Education, classified distal pancreatectomy as an “ESSENTIAL UNCOMMON” procedure, and other pancreatic resections as “COMPLEX” procedures.
HALLMARK ANATOMIC COMPLICATIONS
Tearing of the gonadal vein during Kocher maneuver
Inadvertent division of the hepatic artery
Injury to superior mesenteric vein (SMV) or branches during retraction (gastroepiploic or middle colic veins) or dissection (first jejunal branch, uncinate branch)
Accidental division of a replaced right hepatic artery coursing behind pancreas and/or common bile duct
Mesenteric bleeding during resection of first portion of jejunum
Inadvertent injury to the middle colic vessels or transverse mesocolon
Abdominal collection (sterile or infected)
Pancreatic leak/fistula/abscess
Bile leak, delayed gastric emptying (for pancreaticoduodenectomy)
Delayed hemorrhage (most commonly gastroduodenal artery [GDA] after a pancreatic leak)
LIST OF STRUCTURES
Pancreas
Head
Body
Tail
Uncinate process
Pancreatic duct
Spleen
Splenic artery
Splenic vein
Colon
Transverse mesocolon
Transverse colon
Middle colic artery and veins
Stomach
Greater curvature
Pylorus
Antrum
Duodenum
First, second, third, and fourth portions
Ligament of Treitz
Gallbladder
Cystic artery
Cystic duct
Bile duct
Porta hepatis
Right hepatic artery (and anatomic variants)
Portal vein
Superior mesenteric artery and vein
Inferior vena cava (IVC) and right gonadal vein
Left and right gastroepiploic arteries and veins
Inferior (transverse) pancreatic artery
Gastrocolic omentum (ligament)
Gastrosplenic ligament
Splenocolic ligament
Distal Pancreatectomy with or without Splenectomy
STEPS IN PROCEDURE
Distal Pancreatectomy
Diagnostic laparoscopy (adenocarcinoma of body or tail)
Upper midline or extended left subcostal incision
Start with a small incision and palpate the liver and the remainder of the abdomen for M1 disease
Open the greater omentum and enter the lesser sac and lower right colon
Divide gastroepiploic vessels
Preserve short gastrics (for splenic preservation)
Mobilize back wall of stomach from pancreas and inferior border of pancreas from transverse mesocolon
Create a tunnel behind the pancreas over the SMV
Secure gastropancreatic arteries and divide pancreas
If splenectomy: Staple or suture ligate the splenic artery followed by the vein and move medial to lateral and perform splenectomy
If splenic preservation: Elevate distal remnant and gently dissect from splenic vessels
If splenic vessels need to be taken, the short gastric vessels must have been preserved (Warshaw procedure)
Check for a defect in the transverse mesocolon before closure
Consider using a drain if high risk features present (e.g., small duct, soft pancreas)
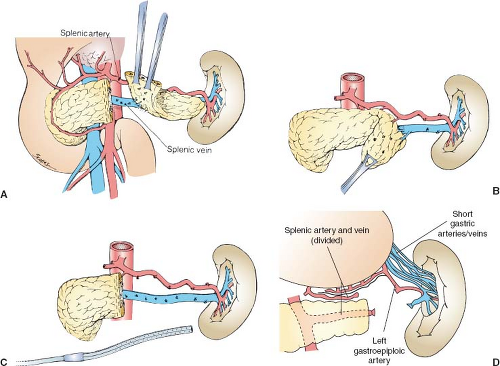
Exposure of the Body and Tail of the Pancreas and Resection of Distal Pancreas (Fig. 84.2)
Technical Points
Use an upper midline (most patients) or extended left subcostal or Chevron incision (morbidly obese patient). Explore for distant disease. Make a window in the gastrocolic omentum by dividing the gastroepiploic vessels on the greater curvature of the stomach. Divide these from the region of the distal antrum to the short gastric vessels. Preserve the short gastric vessels if planning splenic preservation and if the main splenic artery and vein are going to require resection (Warshaw modification). At this point, the greater omentum can be removed to enhance exposure or retraction or simply moved out of the way (see Chapter 80e, Figure 80.5). Protect the transverse mesocolon throughout the operation when dissecting on the inferior border of the pancreas.
Follow the gastroepiploic vein and middle colic down to the SMV to define the medial point of transection for formal left pancreatectomy. Now place retractors in to maintain the stomach in an elevated position along with the left lateral segment of the liver and take care to not injure the left gastric arcade. Retract the colon inferiorly. Divide the avascular folds between the stomach and the pancreas (gastropancreatic folds or Allen’s veil) to expose the body and tail of the pancreas fully. The splenic vessels may be palpable in the region of the distal pancreas. The splenic artery runs along the superior surface of the pancreas and is often seen here and can be palpated. Be sure it is not the common hepatic artery. The splenic vein lies posterior to the pancreas and cannot be seen until the pancreas is mobilized. Incise the peritoneum along the inferior border of the pancreas with electrocautery and take care not to injure the inferior mesenteric vein (IMV).
Elevate the pancreas out of the retroperitoneum by blunt dissection in an avascular (normally) plane. The splenic artery and vein will be elevated along with the body and tail of the pancreas. Identify the point at which the pancreas is to be divided. Generally, this point will be over the SMV. Develop a plane between the pancreas and the splenic artery and splenic vein by careful blunt dissection. Use Silastic vessel loops on the two vessels to facilitate traction after the plane has been developed. Divide the pancreas using the technique of choice (stapler, sharp with duct ligation, radiofrequency ablation) (Fig. 84.2A).
Alternatively, in some situations, it may be simpler to mobilize the tail of the pancreas first and then divide it (Fig. 84.2B). This is particularly useful in trauma situations where a more limited resection is indicated.
Multiple, short, fine vessels connecting the body and tail of the pancreas to the splenic artery and splenic vein must then be isolated and serially clipped or ligated (Fig. 84.2C). If these small vessels are inadvertently avulsed, use fine Prolene sutures to obtain hemostasis in the splenic artery and splenic vein. Continue the dissection out to the tail of the pancreas, preserving the splenic artery and splenic vein.
The splenic artery and vein can be taken safely if the short gastric vessels were left intact (Warshaw procedure). The application of this technique to a limited distal pancreatectomy is shown in Figure 84.2D. As previously noted, formal distal pancreatectomy for tumor generally requires resection to the SMV, but when the procedure is done for trauma a more limited resection may be appropriate. The Warshaw procedure is applicable in either situation.
If splenic preservation is not planned, simply mobilize both the spleen and tail of the pancreas together. Divide the short
gastric vessels. Secure the splenic artery and vein and transect the pancreas with stapler as previous noted.
gastric vessels. Secure the splenic artery and vein and transect the pancreas with stapler as previous noted.
Check the area for hemostasis and place omentum over the pancreatic stump if possible. Intraperitoneal drains may be placed to gravity selectively at the pancreatic stump.
Anatomic Points
The greater omentum is attached to the greater curvature of the stomach and the first part of the duodenum. On the left, it is continuous with the gastrosplenic ligament. The entire length of its posterior surface is adherent to the entire length of the transverse colon. That portion of the greater omentum connecting the stomach and transverse colon is the gastrocolic omentum (ligament). The gastroepiploic vessels, contained within the greater omentum, typically are close to the stomach, but may be 2 cm or more distant from the stomach.
On the left, the gastrosplenic and splenocolic ligaments are continuous with the greater omentum. Multiple, short, gastric arteries (commonly, four to six) arise from the splenic artery or its branches and run through the gastrosplenic ligament to the greater curvature of the stomach at the fundus. The left gastroepiploic artery has a similar origin and similar course, except that it parallels the greater curvature, running from left to right, ultimately anastomosing with the right gastroepiploic artery. There are no vessels of consequence in the splenocolic ligament, although small communications may exist between the splenic vessels and branches of the middle or right colic vessels.
The lienorenal ligament attaches the spleen to the retroperitoneum. In this ligament are the major splenic vessels and the tail of the pancreas, which usually is either in contact with the splenic hilum or is no more than 1 cm distant from the hilum.
The gastropancreatic folds are formed by the left gastric artery as it passes from the celiac trunk to the upper part of the lesser curvature. Avascular, filmy connections can occur between the visceral peritoneum of the stomach and the parietal peritoneum
covering the pancreas. These are common at the right extremity of the stomach, where the antrum is in close proximity to the head of the pancreas, and, on the left, where the posterior surface of the stomach is very close to the tail of the pancreas. These avascular folds tether the stomach to the posterior wall of the lesser sac, as the duodenum starts to become retroperitoneal, and to the gastrosplenic ligament and its contained vasculature.
covering the pancreas. These are common at the right extremity of the stomach, where the antrum is in close proximity to the head of the pancreas, and, on the left, where the posterior surface of the stomach is very close to the tail of the pancreas. These avascular folds tether the stomach to the posterior wall of the lesser sac, as the duodenum starts to become retroperitoneal, and to the gastrosplenic ligament and its contained vasculature.
The splenic artery runs along the superior border of the pancreas from its celiac trunk origin to the hilum of the spleen. The celiac trunk lies superior and to the left of the neck of the pancreas. As it progresses toward the spleen, it has a characteristically tortuous course (in the adult) owing to tethering by pancreatic branches, and it frequently dips downward posterior to the pancreas. By contrast, the splenic vein should not be visible until the pancreatic tail and splenic hilum are explored because this vein is posterior to the pancreas. As these vessels approach the splenic hilum, both artery and vein have a variable number of splenic branches or tributaries (usually two or three) that serve the different splenic segments; this branching most commonly occurs about 4 cm from the splenic hilum, but the distance may range from 1 to 12 cm. Typically, the splenic vein tributaries are inferior and somewhat posterior to the corresponding arterial branches.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree