Pancreatic Resections
In this chapter, distal pancreatectomy (resection of the tail of the pancreas) will be described first. Because of the close anatomic proximity of the tail of pancreas to the splenic vessels, splenectomy is generally performed when the tail of the pancreas is resected. When this operation is performed for benign tumors or for trauma, it may be possible to preserve the blood supply of the spleen. Both methods of performing the procedure are described in this section. Laparoscopic distal pancreatectomy is described in Chapter 72.
Resection of the head of the pancreas is done in combination with duodenal resection. This procedure is called pancreatoduodenectomy, or the Whipple procedure. It is described in the second part of this chapter. Both the conventional and the pylorus-preserving version of this procedure are described. Total pancreatectomy is discussed briefly. References at the end of the chapter give additional details about this and other specialized pancreatic procedures.
Steps in Procedure
Distal Pancreatectomy without Splenectomy
Upper midline or extended left subcostal incision, thorough abdominal exploration
Clamp and divide gastroepiploic vessels on the greater curvature of stomach from distal antrum to short gastric vessels
Mobilize back wall of stomach from pancreas
Incise peritoneum along inferior aspect of pancreas and gently elevate pancreas from retroperitoneum
Separate pancreas from splenic artery and splenic vein
Choose point of division on pancreas, secure gastropancreatic arteries, and divide pancreas with a stapler (3.5-mm cartridges)
If desired, oversew pancreatic duct with suture ligature
Elevate distal remnant and gently dissect from splenic vessels
Control multiple small tributaries with clips or fine Prolene sutures
Check hemostasis and place omentum over pancreas
Place a closed suction drain, if desired, and close abdomen in the usual fashion
Distal Pancreatectomy with Splenectomy
Incision and exploration as noted above
Incise peritoneum lateral to spleen and mobilize spleen and tail of pancreas into operative field
Determine point of division; isolate, ligate, and divide splenic artery and vein
Proceed as noted above
Pancreaticoduodenectomy (Whipple Resection)
Chevron incision, assess resectability
Mobilize hepatic flexure and perform wide Kocher maneuver
Open gastrocolic omentum by dividing gastroepiploic vessels along greater curvature
Feel tumor and assess proximity to superior mesenteric artery and vein and portal vein
Entering adventitial plane of vein, develop space behind pancreas
If tumor is respectable, pass Penrose drain around pancreas, elevating it from portal vein
For standard pancreaticoduodenectomy
Choose point of division on greater curvature of stomach and create a window in the lesser omentum
Partially divide stomach with straight clamps, create Hofmeister shelf with stapler
For pylorus-preserving pancreaticoduodenectomy
Incise peritoneum above and below first portion of duodenum about 1 cm beyond pylorus
Gently develop plane behind duodenum
Divide duodenum with linear stapler
Elevate proximal stomach (with pylorus, if preserved) and mobilize from underlying pancreas
Perform cholecystectomy and divide bile duct above pancreas
Identify ligament of Treitz and divide jejunum at a convenient point just beyond this structure
Mobilize proximal duodenum from ligament of Treitz and pass it through the mesenteric defect into the right side of the field, so that the entire specimen to be resected lies to the right
Complete dissection of duodenum from pancreas up to point of transection
Secure pancreatic arcades with figure-of-eight sutures
Divide pancreas and remove specimen
Assure hemostasis
Anastomose end of pancreas to end of jejunal limb (stent if desired, inkwell if desired)
Anastomose end of bile duct to side of jejunal limb (stent if desired)
Anastomose gastric remnant (or proximal duodenum, if pylorus-preserving Whipple) to side of jejunal limb
Place drains in vicinity of pancreatic anastomosis and biliary anastomosis
Place omentum in vicinity of anastomoses
Close abdomen in the usual fashion
Hallmark Anatomic Complications
Injury to splenic, superior mesenteric, or portal vein
Subphrenic abscess
Anastomotic leak
List of Structures
Pancreas
Head
Body
Tail
Uncinate process
Pancreatic duct
Spleen
Splenic artery
Splenic vein
Hilum of spleen
Colon
Transverse mesocolon
Transverse colon
Middle colic artery and veins
Stomach
Greater curvature
Pylorus
Antrum
Duodenum
First, second, third, and fourth portions
Ligament of Treitz
Gallbladder
Cystic artery
Cystic duct
Bile duct
Porta hepatis
Right hepatic artery
Portal vein
Superior mesenteric artery and vein
Inferior vena cava
Left and right gastroepiploic artery and vein
Gastropancreatic arteries
Inferior (transverse) pancreatic artery
Great pancreatic artery
Gastrocolic omentum (ligament)
Gastropancreatic folds
Gastrosplenic ligament
Splenocolic ligament
Distal Pancreatectomy without Splenectomy
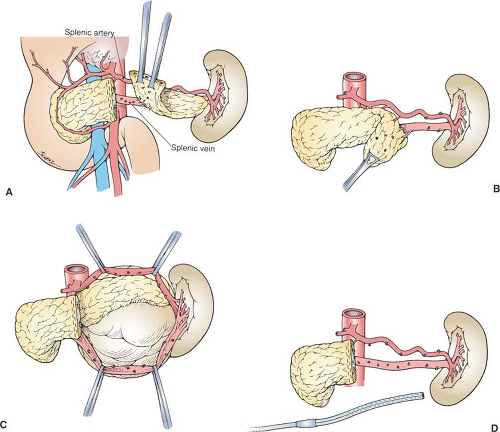
Exposure of the Body and Tail of the Pancreas (Fig. 71.1)
Technical Points
Use an upper midline or extended left subcostal incision, depending on the body habitus of the patient. Make a window in the gastrocolic omentum by serially clamping and dividing the gastroepiploic vessels on the greater curvature of the stomach. Divide these from the region of the distal antrum to the short gastric vessels. Retract the portion of the stomach that is cephalad to the greater omentum inferiorly. Place retractors or stay sutures to maintain the stomach in an elevated position. Divide the avascular folds between the stomach and pancreas (gastropancreatic folds, or Allen’s veil) to expose the body and tail of the pancreas fully. The splenic vessels may be palpable in the region of the distal pancreas. The splenic artery runs along the superior surface of the pancreas and is often visible, palpable, or both. The splenic vein lies posterior to the pancreas and cannot be seen until the pancreas is mobilized. Incise the peritoneum along the inferior border of the pancreas with electrocautery.
 |
Elevate the pancreas out of the retroperitoneum by blunt dissection in an avascular (normally) plane. The splenic artery and vein will be elevated along with the body and tail of the pancreas. Identify the point at which the pancreas is to be divided. Generally, this point will be somewhat to the left of the superior mesenteric vein. Develop a plane between the pancreas and the splenic artery and splenic vein by careful blunt dissection. Use Silastic vessel loops on the two vessels to facilitate traction after the plane has been developed. Divide the pancreas using a TA-55 stapler with
3.5-mm staples. Place Allis clamps on the distal pancreas and lift up.
3.5-mm staples. Place Allis clamps on the distal pancreas and lift up.
Multiple, short, fine vessels connecting the body and tail of the pancreas to the splenic artery and splenic vein must then be isolated and serially clipped or ligated. If these small vessels are inadvertently avulsed, use fine Prolene sutures to obtain hemostasis in the splenic artery and splenic vein. Continue the dissection out to the tail of the pancreas, preserving the splenic artery and splenic vein. Check the area for hemostasis and place omentum over the pancreatic stump. Closed-suction drains may be placed in the bed of the resection if desired.
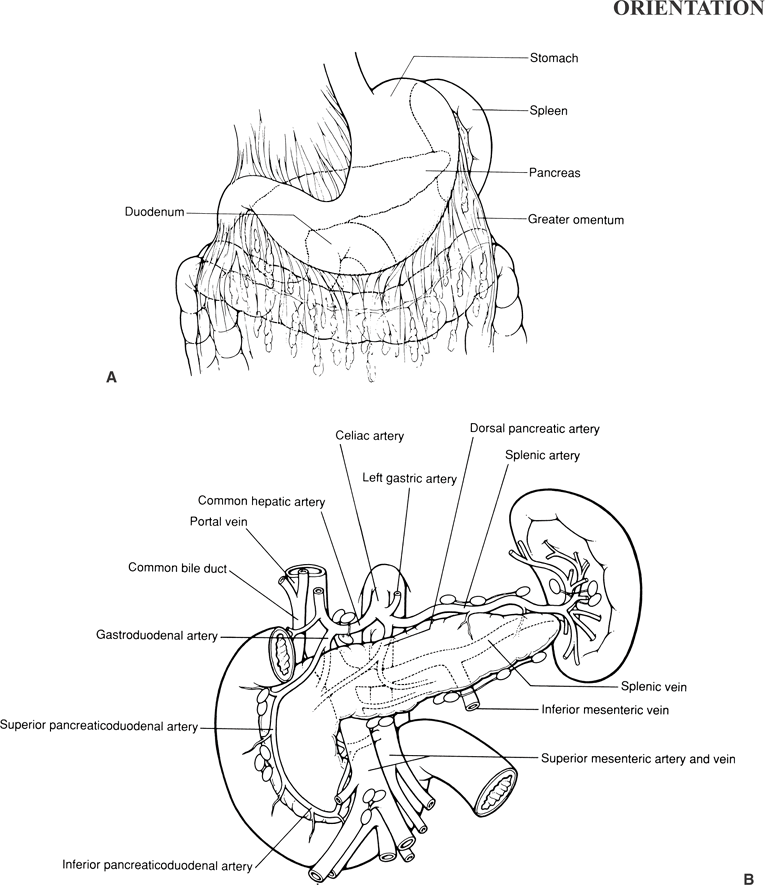
Anatomic Points
The greater omentum is attached to the greater curvature of the stomach and first part of the duodenum. On the left, it is continuous with the gastrosplenic ligament. The entire length of its posterior surface is adherent to the entire length of the transverse colon. That portion of the greater omentum connecting the stomach and transverse colon is the gastrocolic omentum (ligament). The gastroepiploic vessels, contained within the greater omentum, typically are close to the stomach, but may be 2 cm or more distant from the stomach.
On the left, the gastrosplenic and splenocolic ligaments are continuous with the greater omentum. Multiple, short, gastric arteries (commonly, four to six) arise from the splenic artery or its branches and run through the gastrosplenic ligament to the greater curvature of the stomach at the fundus. The left gastroepiploic artery has a similar origin and similar course, except that it parallels the greater curvature, running from left to right, ultimately anastomosing with the right gastroepiploic artery. There are no vessels of consequence in the splenocolic ligament, although small communications may exist between the splenic vessels and branches of the middle or right colic vessels.
The lienorenal ligament attaches the spleen to the retroperitoneum. In this ligament are the major splenic vessels and the
tail of the pancreas, which usually is either in contact with the splenic hilum or is no more than 1 cm distant from the hilum.
tail of the pancreas, which usually is either in contact with the splenic hilum or is no more than 1 cm distant from the hilum.
The gastropancreatic folds are formed by the left gastric artery as it passes from the celiac trunk to the upper part of the lesser curvature. Avascular, filmy connections can occur between the visceral peritoneum of the stomach and the parietal peritoneum covering the pancreas. These are common at the right extremity of the stomach, where the antrum is in close proximity to the head of the pancreas, and, on the left, where the posterior surface of the stomach is very close to the tail of the pancreas. These avascular folds tether the stomach to the posterior wall of the lesser sac, as the duodenum starts to become retroperitoneal, and to the gastrosplenic ligament and its contained vasculature.
The splenic artery runs along the superior border of the pancreas from its celiac trunk origin to the hilum of the spleen. The celiac trunk lies superior and to the left of the neck of the pancreas. As it progresses toward the spleen, it has a characteristically tortuous course (in the adult) owing to tethering by pancreatic branches, and it frequently dips downward posterior to the pancreas. By contrast, the splenic vein should not be visible until the pancreatic tail and splenic hilum are explored because this vein is posterior to the pancreas. As these vessels approach the splenic hilum, both artery and vein have a variable number of splenic branches or tributaries (usually two or three) that serve the different splenic segments; this branching most commonly occurs about 4 cm from the splenic hilum, but the distance may range from 1 to 12 cm. Typically, the splenic vein tributaries are inferior and somewhat posterior to the corresponding arterial branches.
Posterior to the pancreas, an avascular plane exists as a result of the fusion of the mesogastrium with the posterior parietal peritoneum and that those more proximal structures contained within the mesogastrium become retroperitoneal. As could be expected, the avascular fusion plane is also posterior to the splenic vessels.
The relationship of the major vessels posterior to the pancreas is also important. The portal vein, formed by the union of the superior mesenteric and splenic veins, lies to the right of the aorta and superior mesenteric artery. The splenic vein, which lies more or less in the transverse plane, joins the superior mesenteric vein by passing between the superior mesenteric artery and pancreas; thus, in this region, the splenic vein is the most anterior major vascular structure.
As the splenic artery and vein travel along the length of the pancreas, several short, delicate radicles either supply or drain the pancreas. There are more pancreatic veins (15 to 31) than there are pancreatic arteries (4 to 11), and both appear to be distributed fairly evenly along the length of the vessels.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree