Pancreas Resection: Parenchymal, Retroperitoneal, and Bile Duct Margins
SURGICAL/CLINICAL CONSIDERATIONS
Goal of Consultation
Evaluate pancreatic parenchymal and bile duct margins for tumor
Change in Patient Management
Additional tissue may be taken to ensure tumor-free margins
Clinical Setting
Pancreatic tumors can be difficult to diagnose preoperatively
Needle biopsies are associated with complications and potential needle-track seeding
Endoscopic biopsies provide diagnosis in some cases, but tumor may be difficult or impossible to reach using this method
It will not be possible to establish a diagnosis for some patients prior to surgery
Clinical information can provide most likely diagnosis prior to surgery
Age
Average age to develop adenocarcinoma is 71 years, and 90% of patients are > 45
Unusual tumors should be suspected in younger patients (solid pseudopapillary neoplasm, mucinous cystic neoplasm, endocrine neoplasms)
Gender
Adenocarcinomas are more common in males
Some tumors are more common in women (solid pseudopapillary neoplasm, mucinous cystic neoplasm)
Imaging findings
Location in head of pancreas: Cancers obstruct bile duct causing jaundice and often leading to detection at an earlier stage
Location in tail of pancreas: Cancers produce fewer symptoms and often present at a more advanced stage and may not be resectable &/or have metastasized
Endocrine and mucinous neoplasms occur most commonly in tail
Connection to duct system: Typical of intraductal papillary mucinous neoplasms and some other types
Complete (Whipple procedure) or distal pancreatectomy may be performed for potential cure or palliation
Biopsies will be taken of lymph nodes, liver, or other possible sites of metastases
If metastatic carcinoma is found, surgery for cure is no longer possible
Patients with other types of metastatic pancreatic tumors may benefit from resection
SPECIMEN EVALUATION
Gross
Identify all structures present (not all will be present in all resections)
Distal stomach
Usually far from carcinoma and not evaluated by frozen section
Proximal duodenum
Usually far from carcinoma and not evaluated by frozen section
Pancreas (head, tail, or complete pancreatectomy)
Spleen
Involvement by carcinoma would be exceedingly unusual; not generally evaluated by frozen section
Great vessels (superior mesenteric/portal vein)
Usually not resected; if they are resected, surgeon may request evaluation of vascular margins
Examine outer aspects to identify any areas of likely tumor involvement
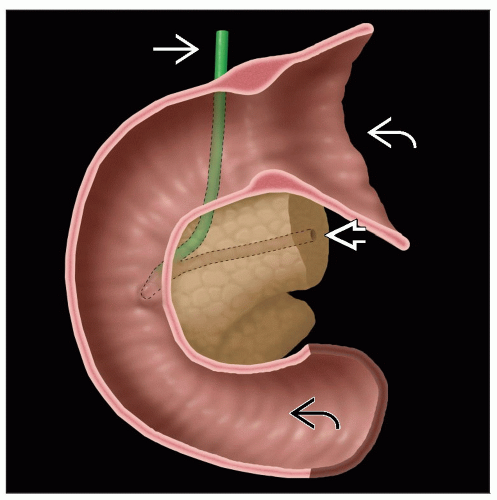
Open stomach along greater curvature and duodenum along outer curvature
If partial pancreatectomy has been performed, identify pancreatic parenchymal margin and pancreatic duct
Ink margin a specific designated color to distinguish it from other margins
Excise margin as en face section
Identify common bile duct margin as it exits pancreas and passes behind proximal duodenum
Ink distal margin
Excise margin as en face section
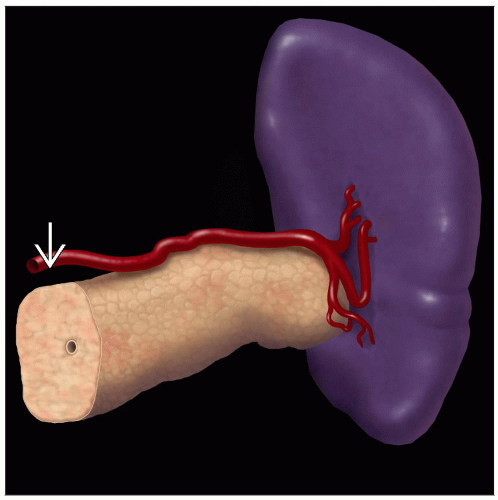
Identify uncinate process (retroperitoneal) margin
This is a nonperitonealized portion of pancreas lying directly on superior mesenteric vessels for 3-4 cm
Surgeon must separate pancreas from blood vessels and surrounding autonomic nerve plexus
Small area of pancreas may be left in this area
This is an important margin and should be inked a specific color for evaluation on permanent sections
This margin is not typically evaluated by frozen section as additional tissue is generally not taken
Remainder of pancreas is inked a different color
Partial pancreatectomy (head of pancreas)
Probes are placed within major ducts
Probe in common bile duct should exit through ampulla in duodenum
Probe in main pancreatic duct is advanced as far as possible
Duct may be obstructed by carcinoma
Pancreatic head is sectioned along plane of both probes
Area of duct obstruction may be identified
Carcinomas are firm and white and efface normal parenchyma
Intraductal papillary mucinous neoplasm (IPMN) is mucinous and papillary in appearance and fills main duct
Distance of gross lesions from common bile duct and pancreatic parenchymal margin is useful in helping determine likelihood of positive margin
Distal pancreatectomy
Parenchymal margin is taken as en face section
Pancreas is serially sectioned perpendicular to long axis
Size, color, borders, and relationship to margins of lesions are recorded
Separate en face parenchymal margin submitted by surgeon
It is recommended that margin be taken from specimen by pathologist
If submitted separately, pathologist cannot evaluate distance of a gross lesion involving main duct from margin
Frozen Section
Pancreatic parenchymal margin
True margin is embedded face up
1st section is true margin
Bile duct margin
True margin is embedded face up
1st section is true margin
Uncinate margin
Not examined by frozen section as additional tissue cannot be resected
Cytologic Preparations
Can be useful for diagnosis of pancreatic mass but not used for margins
MOST COMMON DIAGNOSES
Adenocarcinoma
Most common pancreatic tumor (> 90% of total)
Carcinomas eligible for resection are usually in head of pancreas
Often associated with chronic pancreatitis
Gland may be fibrotic due to inflammatory changes
Carcinomas may be difficult to discern visually or by palpation
Carcinomas efface normal architecture
Often small and diffusely infiltrative
Consist of small tubules or nests of cells
Cytologic atypia may be minimal
Endocrine Tumors
2nd most common pancreatic tumor (3-5% of total)
˜ 10% occur in patients with a germline mutation
Patients with multiple endocrine neoplasia type 1 (MEN1) develop multiple nonfunctioning endocrine microadenomas (< 0.5 cm)
20-70% develop functional tumor
Usually arise in tail of pancreas
Well-circumscribed, encapsulated, fleshy yellow to red masses
Necrosis, cysts, and hemorrhage may be present
Uniform cells in nests, sheets, or trabeculae
Monomorphic nuclei with dispersed (“salt and pepper”) chromatin
Rare or absent mitoses
Small nucleoli
Scant granular cytoplasm
Solid Pseudopapillary Neoplasm
Most common in young women (20s-30s)
Occurs at any site in pancreas
Well-circumscribed solid and cystic tumor that may be unilocular or multilocular
Central necrosis is common
Pseudopapillae form around blood vessels
Nuclei are uniform and grooved
Cells are dyscohesive
Cytoplasmic eosinophilic hyaline globules may be present
Mucinous Cystic Neoplasm
Most common in women (40s-50s)
˜ 1/3 are malignant, usually in older individuals
Mucinous cystadenoma and cystadenocarcinoma are most common in tail of pancreas but also occur in head
Grow as thin-walled cystic tumors containing mucin
Tumors with solid areas or papillary excrescences in cyst wall are more likely to be carcinomas
Do not communicate with duct system
Cysts lined by tall columnar mucin-producing epithelium
Ovarian-type stroma lines cyst wall
Serous Cystic Neoplasm
Intraductal Papillary Mucinous Neoplasm (IPMN)
Macroscopic lesions that grow within duct system of pancreas
Defined as being ≥ 1 cm in size
Often extend microscopically beyond grossly evident mass
Multifocal in 40% of cases
˜ 1/3 associated with invasive carcinoma
Usually involve main pancreatic duct
Majority are in head of pancreas
Can involve entire length of duct as well as common bile duct and ampulla of Vater
Associated pancreas with chronic obstructive pancreatitis
IPMN in branch duct usually forms cystic mass in uncinate process
Mucinous cysts range from 1-10 cm
Cyst walls are thin and have flat or papillary lining
Adjacent pancreas is normal
Lower risk of high-grade dysplasia and invasive carcinoma compared to tumors involving main duct
Histologic types
Gastric type
Low- or intermediate-grade dysplasia most common
Intestinal type
Intermediate- to high-grade dysplasia most common
Pancreaticobiliary type
High-grade dysplasia
Oncocytic type
High-grade dysplasia most common
Not associated with ovarian-type stroma
Pancreatic Intraepithelial Neoplasia (PanIN)
Not detected clinically and not seen on gross examination