Overview of Myeloproliferative Neoplasms
Kathryn Foucar, MD
TERMINOLOGY
Abbreviations
Myeloproliferative neoplasms (MPN)
Synonyms
Chronic myeloproliferative disorders (CMPD)
Definitions
Clonal hematopoietic (HP) neoplasm characterized by bone marrow hypercellularity and intact maturation with effective hematopoieses resulting in elevations of ≥ 1 HP lineages in blood
Myeloblasts not substantially increased and dysplasia is not significant in chronic phase of MPN
Molecular genetic abnormalities are common in MPN and define some subtypes
Mutations in tyrosine kinase genes in most MPNs
About 10% of MPN cases are unclassifiable
WHO 2008 classification of MPN
Chronic myelogenous leukemia (CML) BCR-ABL1(+)
Polycythemia vera (PV)
Primary myelofibrosis (PMF)
Essential thrombocythemia (ET)
Chronic neutrophilic leukemia (CNL)
Chronic eosinophilic leukemia, not otherwise specified (CEL, NOS)
Mastocytosis
MPN, unclassifiable (MPN-U)
Cases do not fulfill criteria for other MPN
ETIOLOGY/PATHOGENESIS
Mutations in Tyrosine Kinase Genes
Present in virtually all types of MPN
Acquired mutations in tyrosine kinase genes result in constitutive activation
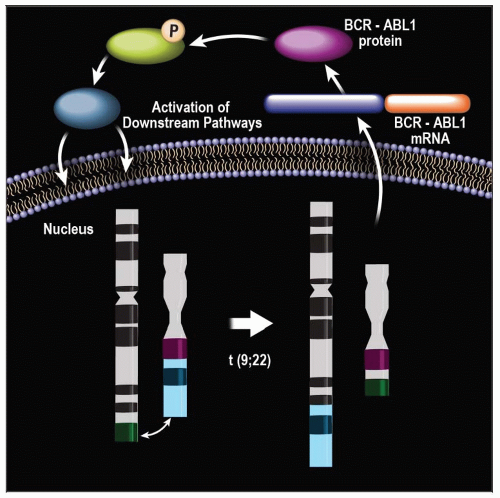
BCR-ABL1 fusion gene
Defines CML
Responsible for dysregulated overproduction of neutrophils, basophils, and variable other HP cells
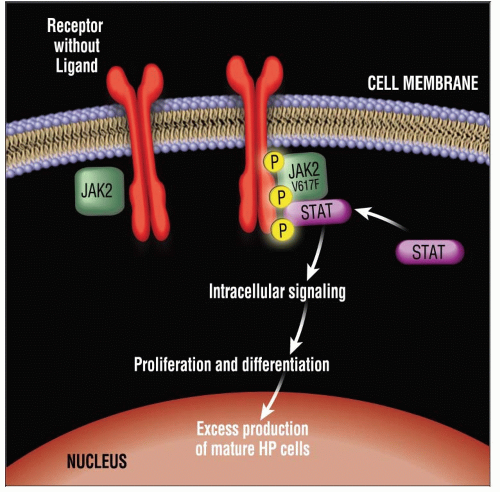
JAK2 V617F mutation
Detected in almost all cases of PV (alternate JAK2 mutation in remainder)
Detected in about 1/2 of ET and PMF cases
Occasionally detected in other myeloid neoplasms
MPL W151 L/K mutation
Detected in many PMF and some ET cases
KIT D816V mutation
Common in mastocytosis
CLINICAL IMPLICATIONS
Epidemiology
Incidence
Rates for MPN subtypes range from rare case reports of CNL to 1-2 cases per 100,000 for CML & ET
Age
MPNs predominate in middle-aged to elderly
Rare presentations in children (e.g., CML)
Localized extramedullary (cutaneous) forms of mastocytosis predominate in children
Gender
No striking gender predilection
Ethnicity
No striking ethnic predilections
Presentation
Most MPNs exhibit indolent type of presentation with gradual onset of symptomatology
Many distinctive & more dramatic manifestations in mastocytosis secondary to granule release
Flushing, urticaria, gastrointestinal symptoms
Splenomegaly is a hallmark of many MPNs
CML, PV, PMF
Laboratory Tests
Complete blood count (CBC) with differential provides many clues to MPN and specific MPN subtypes
Marked nontoxic neutrophilia, left shift to blasts, and basophilia in CML
Erythrocytosis in PV
Leukocytosis, leukoerythroblastic picture, and teardrop-shaped RBCs in PMF
Thrombocytosis in ET
Marked eosinophilia in CEL, NOS
Many other laboratory tests utilized to exclude differential diagnostic considerations and assess cell turnover, iron stores, and erythropoietin levels
Natural History
Most well-delineated for CML, PV, PMF, and ET
ET often very indolent with survival times similar to age-matched controls
PV characterized by long stable phase with eventual progression to myelofibrosis (> 10-year survival); substantial risk of thrombosis
PMF shows variable survival times: Range of 3-7 years
Prior to era of tyrosine kinase inhibitor therapy, CML patients had median survival < 5 years and inevitable accelerated/blast phase
Treatment
Tyrosine kinase inhibitor therapy has resulted in markedly prolonged survival in CML
Dramatic reductions in incidence of disease progression
Application of tyrosine kinase inhibitors in JAK2 mutation-mediated neoplasms in progress
MICROSCOPIC FINDINGS
Blood
Key general features include cytosis(es), lack of dysplasia, blasts < 2%, and basophilia
Other specific features of individual MPNs
Teardrop-shaped erythrocytes in PMF
Marked erythrocytosis in PV
Marked eosinophilia in CEL
Toxic neutrophilia in CNL
Bone Marrow
General features
Hypercellularity
Increased megakaryocytes
Intact maturation
Lack of dysplasia in stable phase (aside from megakaryocytes)
Blasts < 2% in stable phase
Distinctive MPN subtype-specific features
Small, hypolobated megakaryocytes in CML
Markedly hyperlobated megakaryocytes in ET
Prominent intrasinusoidal megakaryocytes in PMF
Osteosclerosis in PMF and some mastocytoses
Fibrosis in PMF and some mastocytoses
Normocellularity in some ET
Marked eosinophilia in CEL, some mastocytoses
Associated non-mast cell hematologic disorders in systemic mastocytosis
ANCILLARY TESTS
Flow Cytometric Immunophenotyping
Relatively limited utility in chronic phase MPN
Valuable for blast lineage assessment and enumeration in progressive MPNs
Valuable in detecting aberrant CD2 and CD25 on neoplastic mast cells
Cytogenetics/FISH/Molecular Genetic Testing
Essential in diagnosis of most MPN subtypes
Essential for exclusionary reasons in CNL, CEL, NOS
DIFFERENTIAL DIAGNOSIS
MPN vs. Disorders That Mimic MPN
Collagen vascular diseases
Chronic infections
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree