Overview of Megakaryocytic Disorders
Kaaren K. Reichard, MD
TERMINOLOGY
Abbreviations
Immune thrombocytopenia (ITP)
Myelodysplasia (MDS)
Myeloproliferative neoplasm (MPN)
Acute myeloid leukemia (AML)
EPIDEMIOLOGY
Age Range
Full spectrum
Constitutional disorders
Predominate in the young
Diagnosed in early childhood/infancy
Acquired disorders
Tend to predominate in adults
Key exceptions: ITP, neonatal thrombocytopenia
May be neoplastic or nonneoplastic
Incidence
Constitutional megakaryocytic disorders
Rare
Acquired, reactive thrombocytosis and thrombocytopenia
More common than constitutional/neoplastic counterparts
ETIOLOGY/PATHOGENESIS
Constitutional Disorders
Often result of underlying genetic mutation
Predisposition to malignancy
Acquired Disorders
Nonneoplastic
Nonclonal
Variety of causes
Infection
Inflammatory conditions
Drug
Autoimmune-related phenomena
Neoplastic
Clonal
Exposure to toxic substances
Carcinogens
Chemotherapy
Radiation
Acquired genetic mutations
CLINICAL IMPLICATIONS
Clinical Presentation
Constitutional megakaryocytic disorders
Often associated with physical abnormalities
May be associated with mental deficiency
Presentation in early childhood/infancy
Abnormal complete blood cell count (CBC)
Thrombocytosis
Thrombocytopenia
Bleeding tendency with thrombocytopenia
Some predisposition to thrombosis with thrombocytosis
Acquired platelet/megakaryocytic disorders, nonneoplastic
Reactive thrombocytosis
Clinically benign
Generally transient phenomenon
Treat underlying cause
Mild thrombocytopenia
Usually not associated with catastrophic clinical consequences
Moderate or severe thrombocytopenia
Acquired megakaryocytic disorders, neoplastic
Abnormal CBC
Bone marrow failure, except for MPN
Cytopenias
Bleeding
Infection
Cytoses
Thrombosis
MICROSCOPIC FINDINGS
Normal Megakaryopoiesis
Megakaryocytes originate from hematopoietic stem cells
Cells committed to megakaryocytic lineage
Immunophenotypic identification
Expression of CD41a, CD42b, CD31, and von Willebrand factor (vWF)
Thrombopoietin is primary regulator
Loss of MPL or THPO gene results in profound thrombocytopenia
TPO normally binds to its receptor (Mpl)
Megakaryocytic maturation
DNA replication without cell division
Process termed endomitosis
Results in markedly enlarged cell with large amounts of cytoplasm
Megakaryocytes are multilobulated
Megakaryocytes are polyploid
Often 16N or occasionally 32N or 64N
1,000-3,000 platelets shed from cytoplasm of each megakaryocyte
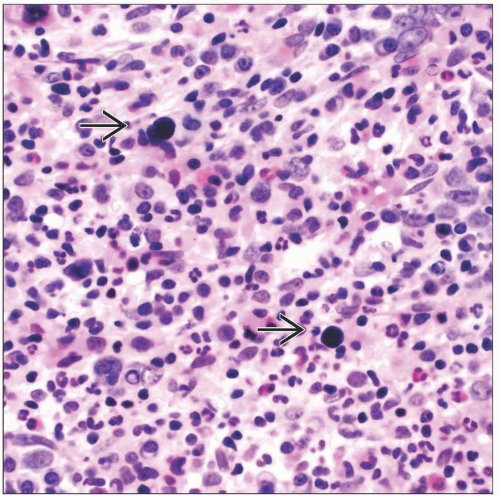
Megakaryocyte morphology
Megakaryoblasts are difficult to identify in BM
Blasts may show cytoplasmic blebbing
Immature (young) megakaryocytes
Smaller overall size
Higher nuclear to cytoplasmic ratio
More basophilic cytoplasmic appearance
Fewer nuclear lobes
Mature megakaryocytes
Voluminous, granular, pink cytoplasm
May exhibit broad range in size
May exhibit broad range in nuclear lobation
Assessment in BM aspirate
Megakaryocytes tend to reside in particles
In particles, more difficult to assess cytomorphology
In contrast to core biopsy, no sectioning artifact
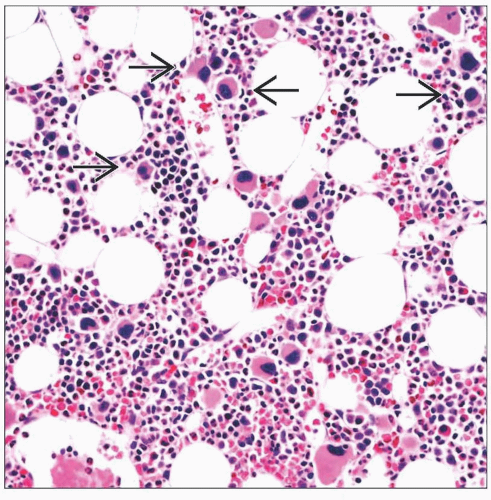
Assessment in BM core biopsy
Advocated by many experts
Recall sectioning artifact when identifying hypolobated megakaryocytes
Due to large size, sectioning through megakaryocytes may distort morphology
Megakaryocyte BM topography
Predominantly individually distributed
Rarely, may see loose clusters
On average, range from 1-5 megakaryocytes on typical 40x magnification
Megakaryocytes typically reside adjacent to BM sinuses
Facilitates prompt shedding of platelets into circulation
Facilitates transmigration of other nucleated cells (e.g., neutrophils) through their cytoplasm (a.k.a. emperipolesis)
Highlight location with immunohistochemistry (CD31)
Normal Platelet Production and Appearance
Platelets are formed from pseudopodial megakaryocytic projections
Adult human can produce 1011 platelets per day; more if needed
Typical size: 2-4 µm
Typical count: 150-400 × 109/L in peripheral blood (PB)
Typically well granulated
Circulating megakaryocytes/megakaryocytic nuclei
Typically seen along feathered edge of blood smear
May be seen in neoplastic and nonneoplastic conditions
Nonneoplastic conditions
Acute stress
Severe infection
Trauma
Surgery
Burn
Neoplastic conditions
Variety of disorders: Mainly primary hematopoietic
Abnormal Megakaryopoiesis
Abnormal cytomorphology
Hypolobation/monolobation
Characteristic of myeloid neoplasms, particularly a myelodysplasia-related change
Cytoplasm remains eosinophilic with mature appearance
Not specific for clonal disorder: ITP, HIV infection, collagen vascular disease, certain drugs (e.g., valproate)
Megakaryocytes with distinctly separate nuclei
Characteristic of MDS
So-called pawn ball in the literature
Marked hyperlobulation
Sufficient numbers generally indicate a myeloid neoplasm
Megakaryocytes with > 64N (2N is normal diploid)
Pleomorphic and bizarre nuclei
Sufficient numbers generally indicate a myeloid neoplasm
Hyperchromasia
Naked nuclei
Prominent feature of ITP and HIV infection
Also seen in MPNs, namely primary myelofibrosis and polycythemia vera
Abnormal clustering
Characteristic of myeloid, particularly myeloproliferative, neoplasms
Not specific for clonal disorder
May be seen as early regenerative phenomenon after BM injury/toxic insult
Intrasinusoidal location
Characteristic of myeloproliferative neoplasms
Often indicative of extramedullary hematopoiesis
Not specific for clonal disorder
Abnormal Platelets
Abnormal size
Large
Macrothrombocytopenic disorders (e.g., ITP, MYH9-related diseases, Bernard-Soulier, Gray platelet syndrome)
Small
Thrombocytopenic disorders (e.g., WiskottAldrich syndrome)
Hypogranular/gray
Abnormal number
Thrombocytopenia
Thrombocytosis
APPROACH TO MEGAKARYOCYTIC/PLATELET DISORDERS
Constitutional vs. Acquired Disorder
May further subclassify based on platelet count on number of BM megakaryocytes
Thrombocytosis defined as > 450 × 109/L
Thrombocytopenia defined as < 150 × 109/L
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree