Ovary, Mass: Diagnosis
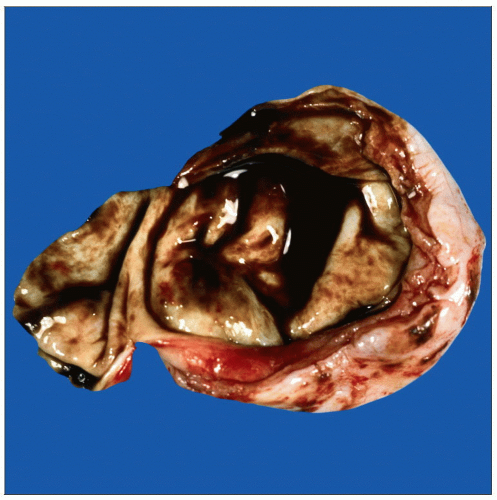 A typical endometrioma, or “chocolate cyst,” of the ovary has a flat velvety lining and is filled with a thick, brown fluid. Carcinomas arising in these lesions may form masses or papillary areas. |
SURGICAL/CLINICAL CONSIDERATIONS
Goal of Consultation
Determine if ovarian lesion is benign or malignant
Malignant mucinous carcinomas are evaluated for likelihood of metastasis vs. primary carcinoma
Accurately stage patients with carcinoma
For patients with uterine carcinoma, involvement of ovaries increases stage
For patients with ovarian carcinoma, surface involvement of ovary may alter stage
Change in Patient Management
If malignancy is identified, appropriate staging biopsies and definitive surgery may be performed
Total abdominal hysterectomy and bilateral salpingooophorectomy
Debulking of large tumors
Peritoneal washings
Lymph node biopsies
If no malignancy is identified, no additional surgery is required
Fertility can be preserved in premenopausal women
If metastasis to ovary is suspected and there is no prior history of carcinoma, peritoneal cavity is inspected for possible primary sites
Appendix is a possible site and may be resected
Clinical Setting
It is difficult to determine if ovarian mass is benign or malignant preoperatively
Imaging findings are often nonspecific
Needle biopsy is contraindicated due to risk of spillage of malignant cells into peritoneal cavity
Malignancy is more common in women > age 40
Ovarian lesions in women < age 40 are generally benign
Preservation of fertility is a frequent goal in young women
SPECIMEN EVALUATION
Gross
Great care should be used in examining outer surface of ovary, as involvement may alter stage
Do not rub or abrade surface
Note any irregularities
May be due to carcinoma penetrating capsule or to a serosal metastasis
Selectively ink surface including any possible excrescences or metastasis
Serially section ovary
Cysts with fluid under pressure can appear to be solid masses by palpation
These cysts should be opened with caution and with proper eye protection to avoid uncontrolled release of contents
Small incision directed away from prosector should be made
Adequate surgical drapes, pan, or sink should be available to dispose of cyst fluid
If multilocular, all cysts should be opened
Evaluate appearance of solid masses and cysts
Do not touch inner surface of cysts as this may dislodge diagnostic cells
Bilateral involvement or multiple nodules within a single ovary may be seen in metastatic disease
Note whether contents are serous (freely flowing) or mucinous (viscous and sticky)
Unilocular cyst with smooth inner lining
Almost always benign
Gross examination is sufficient
Cystic lesion filled with sebaceous material and hair
Mature cystic teratoma (dermoid cyst)
Almost always benign
Gross examination is sufficient unless there is a substantial solid area or cyst has ruptured
Unilocular or multilocular cysts with irregular lining or solid areas
Lining is inspected
Minute papillary excrescences or solid/nodular areas are suspicious for borderline tumors or malignancy
Most suspicious area may be selected for frozen section
Hemorrhagic mass
Most common diagnoses are ovarian torsion, endometrioma, and nongestational choriocarcinoma
Tumors are sometimes cause of torsion
Carcinomas may arise in endometriomas in older women
Solid areas suspicious for carcinoma may be selected for frozen section
Solid mass
Majority are benign, but many malignancies have this appearance
Carcinomas typically have a homogeneous appearance with variable amounts of necrosis, hemorrhage, and cystic degeneration
Frozen Section
1-2 representative sections of area most likely to show malignancy may be frozen
2 frozen sections may be performed in cases of suspected borderline tumor (both mucinous and serous) or mucinous carcinoma
If definite diagnostic features are not seen, lesion is best evaluated by extensive sampling on permanent sections
MOST COMMON DIAGNOSES
Mature Cystic Teratoma (Dermoid)
Most common tumor of ovary
10-15% are bilateral
Most common in premenopausal women
Unilocular cystic mass filled with sebaceous material, keratin, and hair
Rare tumors have immature elements (immature teratoma)
Appear as homogeneous, fleshy or solid areas
Foci of necrosis may be present
May be intermingled with mature areas
Spontaneous rupture is suspicious for underlying malignancy
Cellular immature areas need to be distinguished from differentiated neural tissue (e.g., retina or cerebellum)
Difficult to make a malignant diagnosis on frozen section
Gross examination may be sufficient if no suspicious areas are identified and pathologic and clinical impressions agree
Serous Tumors
˜ 5-10% borderline, 20-25% malignant, and remainder benign
May be unilocular or multilocular
Cysts are filled with clear, watery serous fluid
Benign tumors have thin cyst walls with smooth inner linings
Borderline lesions have numerous small papillary projections in inner cyst lining
Carcinomas have areas of solid &/or papillary growth
Most common type of ovarian malignancy
Malignant features are generally present throughout tumor
Necrosis often present
Surface involvement common
May be extensive
May invade adjacent structures
25-30% bilateral
30% associated with extraovarian implants
Mucinous Tumors
˜ 10-15% borderline, 10% malignant, and remainder benign
Benign and borderline tumors tend to be large (≥ 20 cm)
Carcinomas are generally smaller
5% of benign lesions are bilateral and 20% of carcinomas are bilateral
May be difficult to distinguish from metastatic carcinomas
Cysts filled with viscous gelatinous fluid
Benign tumors usually simple cysts with thin, delicate cyst walls and a smooth inner lining
Borderline tumors are usually multilocular
May only have focal areas of papillary projections within cyst wall
Carcinomas are often multilocular with solid areas and necrosis
Diagnostic features of malignancy can be very focal
May be difficult to document malignancy on limited sampling by frozen section
At least 2 frozen sections should be examined
Fibroma
Well-circumscribed firm mass with a homogeneous chalky white, whorled surface
Almost all bilateral
Fibrosarcomas are rare
Thecoma
Large (often > 10 cm), lobulated, solid, yellow tumor
Calcifications, cysts, hemorrhage, and necrosis may be present
Majority are unilateral
Endometrial hyperplasia may be present due to secretion of estrogen by tumor
Endometrioid Neoplasms
Usually, mixture of solid and cystic areas
40% are bilateral
Cysts filled with hemorrhagic or mucinous fluid
Majority are malignant
Metaplasia is common (squamous, secretory, oxyphilic)
Wide variety of histologic patterns occur (including spindle, adenoid cystic, microglandular)
Can resemble metastatic colon carcinoma
15-20% are associated with endometriosis
Brenner Tumor
Germ Cell Tumors
More common in children and young adults
Dysgerminoma: Large, solid masses with creamy white “cerebriform” cut surface
Embryonal carcinoma: Solid, soft, heterogeneous mass with abundant hemorrhage and necrosis and occasional cysts
Yolk sac tumor: Large tumors with a solid and cystic cut surface, usually associated with hemorrhage and necrosis
Nongestational choriocarcinoma: Rare in its pure form, typically presents as solid, unilateral hemorrhagic mass
Usually a component of a mixed germ cell tumor
Clear Cell Carcinoma
May be solid or cystic
Usually unilateral or only minimally involves surface of contralateral ovary
Can arise as fleshy nodule in an endometriotic cyst
Can mimic low-grade mucinous and serous tumors
Clear cells may not be as apparent on frozen section as they are on permanent sections
Due to tumor heterogeneity, marked nuclear atypia and mitotic figures may not be seen
Granulosa Cell Tumor
Large (often > 12 cm), soft solid, and cystic yellowbrown masses
Hemorrhagic cysts or necrosis may be present
Majority are unilateral; 5% are bilateral
Have a tendency to rupture preoperatively leading to surgical emergency
Endometrial hyperplasia may be present due to estrogen production by tumor
Monotonous cell population: Nuclear grooves and scant cytoplasm
Cytologic preparations can be helpful to identify nuclear features
Call-Exner bodies: Small spaces filled with eosinophilic material
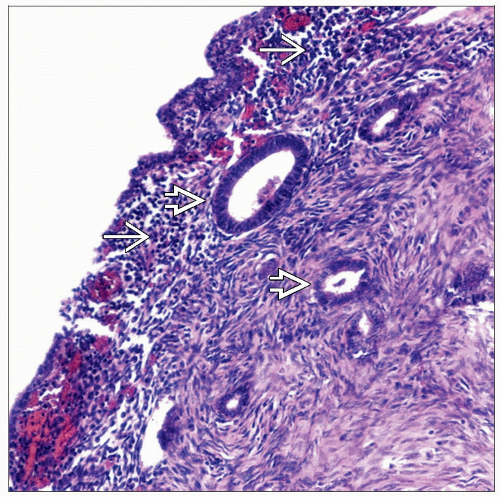
Endometrioma
Usually found in premenopausal women
Cystic mass with shaggy or velvety lining and hemorrhagic contents
Thick, brown, chocolate-like blood within cyst
Surface usually covered by fibrous adhesions
Carcinoma should be suspected in older women
Polypoid masses or solid areas may indicate malignancy (but are most often benign)
Usually endometrioid carcinoma or clear cell carcinoma
Metastatic Carcinoma
May diffusely involve ovary, giving a homogeneous appearance, or be present as multiple nodules
Very large tumors (> 10 cm) are more likely to be primary ovarian carcinomas
˜ 2/3 involve both ovaries
Some primary ovarian tumors may be bilateral
Most commonly from gastrointestinal tract
History of prior malignancy should be provided
If patient has not been diagnosed with cancer and metastasis is suspected, surgeon should closely inspect peritoneal cavity, including appendix
Unusual histologic patterns suggest metastasis
Infiltrative invasive pattern by small glands or single cells is highly suggestive of metastasis
Tall columnar cells with dirty necrosis are typical of metastatic colon carcinoma
Signet ring cell carcinoma may be metastatic from stomach or breast (Krukenberg tumor)
May be associated with stromal hyperplasia and simulate a fibrous lesion
Pseudomyxoma peritonei may involve 1 or both ovaries and mimic a primary ovarian mucinous tumor
Most cases are due to appendiceal primary
Ovarian Masses During Pregnancy
Masses may enlarge secondary to hormonal stimulation, leading to torsion or rupture of ovary
Some lesions are present due to pregnancy
Luteoma of pregnancy, luteal cyst, corpus luteum of pregnancy, stromal hyperthecosis, stromal hyperplasia
Tumors may be altered by pregnant state
Luteinized granulosa cell tumor
Stromal luteinization of metastatic carcinoma
Ovarian Torsion
Enlarged, rubbery ovary with hemorrhage and red to brown discoloration
Gelatinous, “weeping” cut surface
Massive edema may be seen in early stages of ovarian torsion, typically in younger patients
Careful gross examination is important to determine if mass has caused torsion
˜ 1/2 associated with benign neoplasms
˜ 1/3 associated with other types of lesions (endometrioma, corpus luteum, cysts)
Rarely (< 5%) associated with carcinoma
˜ 1/4 of postmenopausal women with torsion will have a malignancy
Follicular Cyst
Small (< 2 cm), thin-walled, unilocular cyst with a smooth inner lining
May contain clear or blood-tinged serous fluid
Cysts have inner layer of granulosa cells with basally located luteinized theca cells
Luteal Cyst
Small, thin-walled cyst with a slightly convoluted yellow inner lining
Usually contains blood, although clear fluid may be present
May become large during pregnancy, and multiple cysts may be present
Cystadenoma
Typically unilocular with flat lining
Small firm excrescences are indicative of cystadenofibroma
Corpus Luteum
Corpora Albicantia
Normal regressed form of a corpus luteum
Small, fibrotic, white lobulated masses
Lutein Cyst (Theca Lutein Cyst)
Bilateral functional cysts that form due to elevated human chorionic gonadotropin (hCG)
Multifetal gestation
Molar pregnancy
Filled with clear yellow fluid
Yellow areas in cyst wall correspond to luteinized cells
Benign Stromal Changes
Stromal hyperthecosis: Bilateral ovarian enlargement with a homogeneous, yellow cut surface
Stromal hyperplasia: Normal to slightly enlarged ovaries with a uniform, occasionally nodular, expansion of ovarian medulla
REPORTING
Frozen Section
Carcinoma
In cases of carcinoma where a subtype (serous, mucinous, or endometrioid) is obvious, a specific diagnosis is appropriate
Example: “Serous carcinoma, high grade, involving ovarian surface in 1 examined section”
Cases with ambiguous histologic features or mixed phenotypes may be reported as “carcinoma” with a note describing tumor grade (low vs. high) and a possible subtype
Example: “Adenocarcinoma, low grade, favor endometrioid in 1 examined section”
If lesion is a possible metastasis, this should be reported
Example: “Adenocarcinoma with extensive necrosis, colorectal metastasis cannot be ruled out”
If definitive diagnosis of carcinoma is uncertain, it is best to defer to permanent sections
Patient can undergo definitive surgery in a 2nd procedure if carcinoma is confirmed
Borderline tumors
Use of phrase “at least” is appropriate to convey heterogeneous nature of these tumors
Up to 1/4 of cases will show areas of carcinoma after more extensive sampling on permanent sections
Example: “At least serous borderline tumor; ovarian surface negative in 2 examined sections”
Number of sections examined should be communicated to surgeon
Solid spindle cell tumors
Fibromas and leiomyomas may appear similar on frozen section; therefore, diagnosis of “benign spindle cell neoplasm” is appropriate
Presence of marked cellularity, atypia, and necrosis may indicate malignant sarcoma
PITFALLS
Adequate Sampling of Large Tumors (> 10 cm)
It may be difficult to exclude malignancy in very large ovarian masses
Mucinous Neoplasms
Mucinous carcinomas can be very heterogeneous in appearance and can require extensive sampling for diagnosis
Metastasis from gastrointestinal primary may mimic ovarian mucinous tumor
Borderline Tumors
Up to 1/4 of tumors classified as borderline on frozen section will be reclassified as malignant after extensive sampling
RELATED REFERENCES
1. Medeiros LR et al: Accuracy of frozen-section analysis in the diagnosis of ovarian tumors: a systematic quantitative review. Int J Gynecol Cancer. 15(2):192-202, 2005
2. Tangjitgamol S et al: Accuracy of frozen section in diagnosis of ovarian mass. Int J Gynecol Cancer. 14(2):212-9, 2004
3. Lee KR et al: The distinction between primary and metastatic mucinous carcinomas of the ovary: gross and histologic findings in 50 cases. Am J Surg Pathol. 27(3):281-92, 2003
4. Kooning PP et al: Relative frequency of primary ovarian neoplasms: a 10-year review. Obstet Gynecol. 74:921-926, 1989