|
Typical Clinical Features |
Microscopic Features |
Ancillary Investigations |
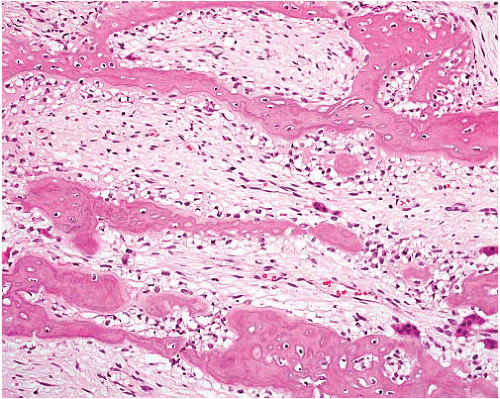
Myositis ossificans |
Young adults, proximal extremities or trunk
Usually intramuscular and often history of trauma |
Zonal pattern
Highest cellularity in early stage
Spindle and stellate fibroblasts resembling nodular fasciitis centrally
Vascular or myxoid stroma with inflammation and extravasated erythrocytes
Transition zone of active bone formation
Peripheral layer of well-formed bone |
Fibroblastic cells SMA+, occasionally desmin+ |
Fibro-osseous pseudotumor |
Adults, digits; infrequently nondigital sites such as wrist
Dermis or subcutis
May have history of trauma |
Variably cellular fascicles of spindle cells in myxoid stroma, similar to nodular fasciitis
Focal irregular bony trabeculae with osteoid and osteoblastic rimming
May display zoning pattern but less organized than in myositis ossificans |
Variably SMA and calponin+ |
Ossifying fibromyxoid tumor |
Subcutaneous circumscribed nodule |
Cords of small rounded glomus like cells in fibromyxoid stroma
About 80% have partial or complete rim of mature bone in capsule, extending long septa
Atypical variants can have intratumoral osteoid and rarely spindle cells |
S100 protein+, GFAP+, desmin±, SMA±, CK+ rarely |
Extraskeletal osteosarcoma |
Older adults |
Atypical osteoblasts producing malignant osteoid and bone |
Similar immunoprofile to skeletal counterpart (e.g., osteocalcin and osteonectin+) |
|
May occur at sites of previous irradiation
Deep soft tissue of extremities, retroperitoneum |
Surrounding tumor varies in morphology but most resemble pleomorphic sarcoma
Atypical mitoses
Calcification, mature bone, and atypical cartilage can be present |
Can show divergent differentiation with variable muscle marker, S100 protein, and CK+ |
Ossifying synovial sarcoma |
Young adults, often ankle or foot, slowly growing |
Irregular distribution of mature bone spicules within tumor
Can be biphasic or monophasic but are often the latter that can be only sparsely cellular
Frequent mast cells
Metaplastic bone can also be seen within fibrous septa |
CK+, EMA+, bcl-2+, CD909+, S100 protein+, TLE1+ |
Lipoma with metaplastic bone |
Usually superficial well-circumscribed masses in adults (some intramuscular, rarely retroperitoneal) |
Resembles mature fat with variation in adipocyte size
Mature-type bone |
MDM2−, CDK4−, no MDM2 amplification, HMGA2 fusions |
Schwannoma with metaplastic bone |
Adults, superficial or deep, head and neck, limbs, retroperitoneum, posterior mediastinum |
Circumscribed, fibrous capsule
Spindle cells with wavy nuclei in palisades or patternless patterns
Inflammatory cells, hyalinization
Mature-type bone |
S100 protein+ (diffuse)
Peripheral rim of EMA+ perineurial cells |
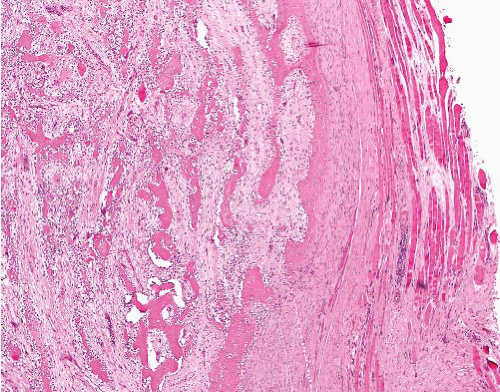
Soft tissue chondroma |
Adults, extraosseous, and extra-articular sites, hands and feet |
Lobules of mature hyaline cartilage, with clusters of chondrocytes
Atypia and normal mitoses can be present, but more mature and sparsely cellular areas elsewhere identify lesion as benign |
S100 protein+ in chondroid areas |
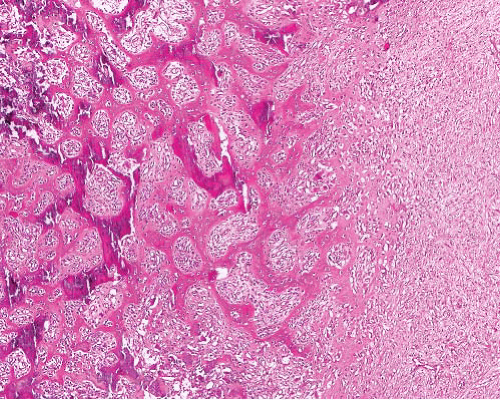
Synovial chondromatosis |
Adults
Synovium of joints, bursae, and tendon sheaths
Most common in large joints (e.g., knee and hip)
Rarely in soft tissue adjacent to, but without communication with, the joint
Has potential for malignant transformation to chondrosarcoma |
Variably cellular nodules and islands of hyaline cartilage, present within the synovial membrane
Atypia, mitoses, and ossification can be present |
S100 protein+ in chondroid areas |
Extraskeletal mesenchymal chondrosarcoma |
Young adults
Head and neck, extremities
Exclude metastasis from extraosseous site |
Biphasic morphology
Hypercellular sheets of primitive small cells with round, ovoid, or spindled nuclei
Discrete or intermingled islands of variably differentiated hyaline cartilage
Hemangiopericytic vascular pattern |
Small cell component CD99+
Cartilaginous component S100 protein+
t(8;8)(q21;q13.3), HEY1-NCOA2 fusion |
Lipoma with metaplastic cartilage |
Usually superficial wellcircumscribed masses in adults (some intramuscular, rarely retroperitoneal) |
Resembles mature fat with variation in adipocyte size
Well-differentiated cartilage |
MDM2−, CDK4−, no MDM2 amplification, HMGA2 fusions |
Atypical lipomatous tumor with metaplastic osteochondroid differentiation |
Deep tumors of adults >50 y |
Adipose tissue with scattered enlarged hyperchromatic nuclei, often found in fibrous septa
Mature-type bone |
MDM2+, CDK4±, p16+, MDM2 gene amplification |
Myxoid liposarcoma with metaplastic osteochondroid differentiation |
Deep soft tissues of extremities of young adults
Often metastasizes to other soft tissue sites as well as to lungs |
Monotonous small uniform spindle or round cells with abundant (myxoid) or minimal (round cell) myxoid matrix
Rich network of delicate vessels becomes inconspicuous in round cell liposarcoma
Lipoblasts |
S100 protein+ in some cases t(12;16) (q13;p11) or t(12;22) (q13;q12) with FUS-DDIT3 or EWSR1-DDIT3 fusion |
Malignant peripheral nerve sheath tumor with divergent osteochondroid differentiation |
M > F
In neurofibromatosis type 1 or sporadic, axial or in limbs
Origin in nerve or neurofibroma |
Elongated spindle cells, wavy or buckled nuclei
Variably cellular and myxoid, fascicular pattern
Nuclei wavy, buckled, or lanceolate
Palisading, neuroid whorls, vascular wall involvement, collagenous “rosettes” |
S100 protein+ focally, occasional GFAP+ |
Dedifferentiated liposarcoma with divergent osteochondroid differentiation |
Older adults, large retroperitoneal tumor, recurrences frequent
M > F |
Low-grade dedifferentiation: cellular fascicles with mild pleomorphism
High-grade dedifferentiation: pleomorphic undifferentiated sarcoma, or myofibrosarcoma-like
Malignant osteochondroid or rhabdomyosarcomatous elements
Well-differentiated liposarcomatous component present or absent |
MDM2+, CDK4+ P16+,
MDM2, CDK4 amplified on fluorescence in situ hybridization+
Variable desmin, SMA, CD34 |