KEY POINTS
The main principle of internal fixation for fracture care (most commonly intramedullary nails or plate and screw fixation) is to create a stable construct that will allow the fracture to heal in proper alignment.
Often, in open fractures, definitive treatment of the fracture is delayed until the wound is sufficiently cleaned and healthy soft tissue is available to cover the fracture.
When compartment syndrome is suspected, emergent fasciotomy must be performed in which the overlying tight fascia is released through long incisions. These must be done as soon as possible because the damage to muscles and nerves will result in irreversible necrosis and contractures causing severe loss of function.
Fractures of the scapula often result from significant trauma and can be associated with injuries to the head, lungs, ribs, and spine.
The shoulder is one of the most commonly dislocated joints and most dislocations are anterior. Posterior dislocations are associated with seizures or electric shock.
Humeral shaft fractures occur from direct trauma to the arm or from a fall on an outstretched arm, especially in elderly patients. The radial nerve spirals around the humeral shaft and is at risk for injury, therefore a careful neurovascular exam is important.
Hemorrhage from pelvic trauma can be life threatening. An important first line treatment in the emergency room is the application of a pelvic binder or sheet that is wrapped tightly around the pelvis to control bleeding.
In spinal injury spinal stability must be assessed, and the patient immobilized until his spine is cleared. CT scan is more reliable in assessing spine injury than plain radiographs.
Spinal cord injuries should be triaged to trauma centers since trauma center care is associated with reduced paralysis.
According to the CDC and the National Health Interview Survey approximately 50 million adults (22% of the US population) have been diagnosed with some form of arthritis. This number is projected to grow to an astounding 67 million adults by 2030 (or 25% of the U.S. population).
Weight loss of as little as 11 pounds has been shown to decrease the risk of developing knee osteoarthritis in women by 50%. Similarly, patients who engage in regular physical activity have been found to have lower incidence of arthritis.
Smaller incisions come with the disadvantage of decreased visualization intra-operatively and associated risks of component malposition, intraoperative fracture and nerve or vascular injury. The only documented benefit of minimally invasive techniques appears to be improved cosmesis.
INTRODUCTION
Orthopedic surgery is a specialty with which every physician should be familiar. Anyone who cares for patients in an outpatient or emergency room setting will find that the majority of presenting complaints involve the musculoskeletal system. A basic understanding of musculoskeletal anatomy is assumed, and understanding the principles of care for musculoskeletal trauma is essential.
For physicians, the field of orthopedics offers an array of subspecialties with such diversity that it seems that “there is something for everyone.” Trauma specialists have the satisfaction of physically putting complex fractures back together. Sports medicine offers remarkably rapid recovery in athletes who have suffered fibrocartilage tears with ever improving arthroscopic techniques and instrumentation. Spine surgeons see remarkable results from their minimally invasive microscopic techniques, while also managing massive deformities with new instrumentation and open surgery. Joint reconstruction is one of our most exciting subspecialties, working with orthopedic bioengineers to develop improved designs, biomaterials, and minimally invasive surgical approaches to return function faster for patients crippled by arthritis and injury. Musculoskeletal oncology offers the intellectual challenge of arriving at appropriate differential diagnoses as well as the technical challenge of limb salvage and major reconstructive surgery. Pediatric orthopedics is an especially challenging and rewarding subspecialty because of the remarkable ability of children to heal even severe injuries rapidly and completely. The incredible array of congenital and developmental disorders makes pediatrics a uniquely intellectually challenging field as well. The authors hope that our readers will share our enthusiasm for orthopedic surgery and all of its subspecialties: trauma, sports, spine, joint replacement, musculoskeletal oncology, and pediatric orthopedics.
ORTHOPEDIC TRAUMA
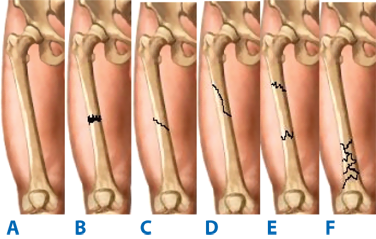
Musculoskeletal injuries resulting from trauma include fractures of bones, damage to joints, and injuries to soft tissues. Long bone fractures can be described as transverse, oblique, spiral, segmental, or comminuted (Fig. 43-1). The goals of treating musculoskeletal injuries are to restore the normal anatomy, immobilize injured extremities for both pain relief and to allow for healing, and to repair or reconstruct these injuries to restore function.
Fractures frequently result from high energy trauma as well as from falls onto an extremity (Fig. 43-2).The majority of fractures can heal well with immobilization, which stabilizes the fracture while new bone forms at the fracture site. Methods of immobilization can vary and depend on the fracture being treated. The most common tool used in orthopedics to treat fractures is immobilization with a splint or cast, and their proper application is important to successfully treat the injury without causing additional problems. A successful splint contains adequate padding on the underlying skin, and particularly over bony prominences, to prevent pressure or burns that can be caused by plaster. Splints, which are not circumferential, are preferred for acute injuries because they allow room for swelling which inevitably occurs after a fracture.
Fractures that are displaced or angulated require closed reduction to properly realign the bone. This is done using analgesia, local or general anesthesia, and often muscle relaxation. Reduction is performed with axial traction and reversal of the mechanism of injury in order to restore length, rotation, and angulation. A splint is then applied and can be gently molded to help hold the reduction in place. It is important to obtain X-rays after a close reduction to verify acceptable alignment of the fracture, and to perform a neurovascular exam to ensure the splint is not too tight.
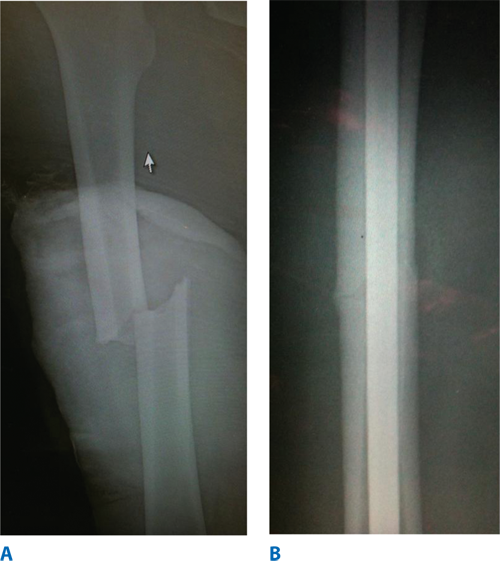
For certain fractures, splint or cast immobilization alone is not enough and in these instances internal fixation is used. The main principle of orthopedic implants for fracture care is to create a stable construct that will allow the fracture to heal in proper alignment. Screws can be placed across a fracture to create compression at the fracture site, which promotes healing. Plates can be placed on the cortex of bones and held with screws, which creates a long area of fixation to stabilize the fracture. Intramedullary rods are commonly used for long bone fractures, such as the femur and tibia (Fig. 43-3A). Prior to their placement, the marrow in the canal is usually removed with a reamer. The rod is then inserted into the canal. Screws can then be placed across the cortices of the bone through holes in the rod proximal and distal to the fracture to create a locked construct that further stabilizes the rod (Fig. 43-3B). In situations where patients are severely injured and cannot safely undergo surgery, or when the soft tissues are too swollen or injured to allow for surgical incisions to be safely made, an external fixation device can be used to temporarily immobilize the fracture. External fixators involve pins placed in bone proximal and distal to the fracture through healthy tissues that are connected by strong rods on the outside extremity, creating a stable construct.
An open fracture occurs when the bone breaks through the skin. These typically result from high energy injuries and are often associated with significant damage to the surrounding soft tissues and contamination of the wound (Fig. 43-4A). These injuries require immediate irrigation and debridement in the operating room and treatment with antibiotics to prevent wound infections and osteomyelitis (Fig. 43-4B). They can also cause injuries to surrounding vessels and nerves, which must be addressed as well. Often, definitive treatment of the fracture is delayed until the wound is sufficiently cleaned and healthy soft tissue is available to cover the fracture.
Compartment syndrome is an orthopedic emergency caused by significant swelling within a compartment of an injured extremity that jeopardizes blood flow to the limb. Increased pressure within the compartment compromises perfusion to muscles and can cause ischemia or necrosis. Patients complain of pain and numbness, and passive stretch of muscles within the compartment causes severe pain. While the diagnosis is based on clinical exam, pressures can be measured with needles placed into the compartment, which is necessary in unconscious patients who will not show these exam findings. When compartment syndrome is suspected, emergent fasciotomy must be performed in which the overlying tight fascia is released through long incisions. These must be done as soon as possible because the damage to muscles and nerves will result in irreversible necrosis and contractures causing severe loss of function.
TREATMENT OF FRACTURES AND DISLOCATIONS
Fractures of the clavicle are one of the most common fractures in orthopedics. They typically occur following a fall onto the shoulder and the majority of clavicle fractures occur in the middle third of the clavicle. Since the bone is subcutaneous, the fracture is often evident on inspection. Most clavicle fractures can be treated nonoperatively with a sling, range of motion exercises, and gradual return to normal activities. Fractures that are significantly displaced and shortened, or that penetrate the skin, are treated with open reduction internal fixation, typically with plate and screw fixation.
Distal clavicle fractures are less common and may occur along with coracoclavicular ligament ruptures. These injuries can be more troublesome and are at risk for nonunion if the bone ends are not in contact. If there is displacement of the fracture, surgical management is often recommended.
Acromioclavicular (AC) joint injuries occur from either a fall directly onto the shoulder or onto an outstretched hand and can result in tears of the acromioclavicular and coracoclavicular ligaments. A step-off, or separation, of the AC joint may be apparent on radiographs. The majority of these injuries can be treated with a sling and gentle range of motion. Injuries resulting in severe displacement of the clavicle may require open reduction and surgical repair.
The sternoclavicular (SC) joint is the only articulation between the upper extremity and the axial skeleton, and injuries to this joint are rare. Anterior dislocations occur more frequently and closed reduction can be attempted, followed by sling immobilization. Posterior SC joint dislocations can be dangerous, resulting in pulmonary or neurovascular compromise, and closed reduction under general anesthesia is recommended with a vascular surgeon present in case of vascular injury.
Fractures of the scapula often result from significant trauma and can be associated with injuries to the head, lungs, ribs, and spine. Most scapula fractures are treated nonoperatively with the exception of fractures to the glenoid. As with most intra-articular fractures, displacement of the articular surface of the glenoid is an indication for open reduction and internal fixation.
The shoulder is one of the most commonly dislocated joints and most dislocations are anterior. They are often associated with injuries to the labrum (Bankart lesion), impression fractures of the humeral head (Hill-Sachs lesion), and rotator cuff tears. Posterior dislocations are associated with seizures or electric shock. Adequate radiographs are required to diagnose a shoulder dislocation, with the axillary view being the most critical. If proper X-rays are not performed then dislocations can be missed and can result in significant debilitation of the shoulder. Dislocation of the shoulders can be managed with closed reduction followed by a short period of sling immobilization.
Proximal humerus fractures occur most frequently in elderly patients following a fall onto the shoulder, though they can also occur following high-energy trauma. They have historically been classified by the number of fracture fragments using the Neer classification, which divides the proximal humerus into 4 parts: the humeral head, greater and lesser tuberosities, and the humeral shaft. Treatment is determined by the displacement of the fracture fragments, the amount of angulation of the fracture, and the amount of comminution (which means multiple fracture fragments). If there is suspicion of an intra-articular fracture, a computerized tomography (CT) scan is often indicated. The majority of proximal humerus fractures is minimally displaced and can be treated with sling immobilization, followed by early shoulder motion and pendulum exercises. Displaced fractures and fractures involving the humeral head are at increased risk for osteonecrosis and therefore surgery is often recommended. If there is adequate bone stock and the fracture can be successfully reduced, open reduction internal fixation with plate and screw fixation is the treatment of choice. Older patients with osteoporotic bone and comminuted fractures are typically treated with a prosthetic replacement of the humeral head, or a hemiarthroplasty.
Humeral shaft fractures occur from direct trauma to the arm or from a fall on an outstretched arm, especially in elderly patients. The radial nerve spirals around the humeral shaft and is at risk for injury, therefore a careful neurovascular exam is important. Most radial nerve injuries are neuropraxias, or stretching of the nerve, and function typically returns in 3 to 4 months. The majority of humeral shaft fractures can heal with nonsurgical management if they are within an acceptable degree of angulation. They are treated with a coaptation splint or functional bracing, which consists of a plastic clamshell brace with Velcro straps. Close follow-up with serial radiographs is important to verify healing of the fracture, and gentle motion exercises are begun within 1 to 2 weeks. Fractures with significant angulation are most commonly treated with open reduction and plate fixation, with care to protect the radial nerve as it often lies close to the fracture site. Intramedullary nailing can also be performed, though it carries the risk of shoulder pain from the nail insertion.
Fractures of the distal humerus result from falls onto the elbow or onto an outstretched arm. Supracondylar fractures are most common, occurring above the elbow joint and do not involve the articular surface. Those minimally displaced can be treated with a posterior long arm splint, with the elbow typically flexed to 90 degrees. Fractures involving the articular surface are treated with plate fixation, and depending on the fracture pattern may require 2 plates, one placed medially and one posterolaterally. As with other intra-articular fractures, the goals of treatment are anatomic reduction of the joint surface with stable fixation, restoration of the anatomic alignment of the joint, and early range of motion. Severely comminuted fractures, especially in the elderly, may be treated with a total elbow replacement, which involves replacing the joint surfaces of the distal humerus, proximal ulna, and radial head with prosthetic components. Fractures about the elbow are notorious for developing stiffness and therefore early motion of the elbow is paramount to a successful outcome. Range of motion should be started as soon as the patient can tolerate therapy.
Dislocations of the elbow are common and typically occur posteriorly after a fall on an outstretched hand. A dislocation results in injury to the joint capsule and rupture of the lateral collateral ligament, though the medial collateral ligament can also be involved. They may even be associated with a fracture of the radial head, coronoid, or the epicondyles of the humerus. Simple elbow dislocations should be urgently reduced with the patient under sedation and treated briefly in a posterior long arm splint. Stiffness of the elbow is a common complication following elbow dislocations and therefore short-term immobilization (about 7–10 days) and early range of motion is recommended.
Dislocations associated with fractures may be treated surgically if there is any instability of the elbow joint. A severe injury, known as the “Terrible Triad,” includes an elbow dislocation, a radial head fracture, and a coronoid fracture. These are unstable injuries and require repair of the torn lateral collateral ligament (LCL), fixation or replacement of the radial head, and possible fixation of the coronoid depending on the size of the fracture fragment.
Most fractures of the radial head can be treated nonoperatively, simply with a sling for 1 to 2 days followed by motion exercises. However, if there is a displaced fracture or if the fracture blocks pronation or supination of the forearm, then surgery is recommended. If the fracture can be well reduced, it is fixed with 1 or 2 screws. If the radial head is fractured into multiple pieces, the treatment of choice is a radial head replacement with a metallic implant. Excision of the radial head can also be performed, but this is reserved for elderly patients with limited demands and may contribute to elbow instability or wrist symptoms over time.
Olecranon fractures occur following a fall directly onto a flexed elbow. Nondisplaced fractures are treated with a splint in 45 to 90 degrees of flexion for a short time followed by range of motion exercises to prevent stiffness. Because the triceps inserts on the olecranon, the pull of the muscle often displaces the fracture, causing a loss of the ability to actively extend the elbow, and therefore should be fixed surgically. Simple transverse fractures can be fixed with a tension band construct, which consists of cerclage wiring passed through the ulna and wrapped in a figure-of-8 fashion around 2 pins placed proximally into the olecranon, creating a compressive force across the fracture to promote healing. Comminuted fractures are treated with plate and screw fixation. Because of the subcutaneous location of the olecranon, this hardware can be irritating to the patient and may need to be removed after the fracture has healed.
Forearm fractures are common injuries that result from high energy trauma or from falls onto an outstretched arm. Both bone forearm fractures often require surgery with plate and screw fixation. The radius has a bow and rotates around the straight ulna for proper pronation and supination of the forearm, and therefore this anatomic relationship needs to be restored to maintain function. An isolated fracture of the ulna shaft, or a “nightstick fracture,” occurs from a direct blow to the side of the forearm. These can usually be treated in a cast, though fractures that are angulated or displaced can be treated with open reduction and plate fixation. A Monteggia fracture is an ulna shaft fracture along with a radial head dislocation. The radial head dislocation may be missed without radiographs of the elbow and therefore a fracture of the ulna should raise suspicion of this injury. These injuries require surgery to fix the ulna fracture with plate and screw fixation and to reduce radial head. A Galeazzi fracture is a radial shaft fracture with disruption of the distal radioulnar joint (DRUJ) at the wrist. After the radius is fixed with plate and screw fixation, the DRUJ is assessed for stability and may need wires placed across the joint temporarily.
Pelvic fractures are indicative of high energy trauma and are associated with head, chest, abdominal, and urogenital injuries. Hemorrhage from pelvic trauma can be life threatening and patients can present with hemodynamic instability, requiring significant fluid resuscitation and blood transfusions. The bleeding that occurs is often due to injury to the venous plexus in the posterior pelvis, though it can also be due to a large vessel injury such as a gluteal artery. Immediate resuscitation is critical and these patients may require surgical exploration or interventional radiology embolization to stop the bleeding. An important first-line treatment in the emergency room is the application of a pelvic binder or sheet that is wrapped tightly around the pelvis to help control bleeding. An external fixator may also be placed in the operating room. Other associated injuries are bladder and urethral injuries that manifest with bleeding from the urethral meatus or blood in the catheter and need to be assessed with a retrograde urethrogram.
The pelvis is a ring structure made up of the sacrum and the two innominate bones that are held together by strong ligaments. Because it is a ring, displacement can only occur if the ring is disrupted in two places. This may occur either from fractures of the bones or tears of the ligaments. There are three main fracture patterns that occur from trauma to the pelvis. An anteroposterior force to the pelvis causes an “open book” injury pattern in which the pelvis springs open, hinged on the intact posterior ligaments with widening of the pubic symphysis. A lateral compression pattern results from a crush injury that causes fractures to the ileum, sacrum, and pubic rami. Vertical shear injuries are very unstable since they result from disruption of the strong posterior pelvic ligaments and are associated with significant blood loss and visceral injuries. Fractures of the sacrum may be difficult to see on x-ray and therefore CT scans are often needed to visualize the fracture pattern. The sacral nerves pass through foramen in the sacrum and therefore fractures that are close to this foramen can result in nerve injuries.
Treatment of pelvic fractures depends on the fracture pattern. Stable, minimally displaced fractures can be treated nonoperatively with protected weight bearing. Open book injuries in which the pubic symphysis is widened and the posterior pelvic ligaments are also injured need to be fixed surgically, which is typically performed with screws placed percutaneously through the ileum into sacrum to stabilize the pelvis posteriorly and a plate and screws over the pubic symphysis to stabilize it anteriorly. Displaced sacral fractures and iliac wing fractures are treated with screws or plates, while pubic rami fractures can usually be managed nonoperatively. While most pelvic fractures are caused by high energy trauma, elderly patients with osteoporotic bone can also suffer pelvic fractures after a fall, usually fracturing the pubic rami. Since these are stable injuries, they can be managed nonoperatively with protected weight bearing.
The acetabulum forms the socket of the hip joint, and fractures occur when the femoral head is driven into it in the setting of high energy trauma. CT scans are important to visualize the fracture pattern. These fractures often require surgery in order to restore a congruent, stable acetabulum, because incongruity of the hip can lead to early degenerative changes and osteoarthritis. These are best treated in the hands of experienced orthopedic trauma surgeons.
Hip dislocations almost always result from high energy trauma and most commonly occur posteriorly. They can cause injury to the sciatic nerve, which runs directly posterior to the hip joint, and may be associated with a fracture of the acetabulum or femoral head. Hip dislocations need to be emergently reduced because of the risk of osteonecrosis of the femoral head when reduction is delayed. They can usually be reduced in the emergency room with adequate sedation and muscle relaxation, but sometimes patients need general anesthesia to aid in the reduction. If this is unsuccessful, or if a fracture fragment gets trapped inside the joint, then an open reduction is performed. Hip dislocations that are associated with a femoral head fracture are at increased risk for osteonecrosis of the femoral head and posttraumatic osteoarthritis.
Hip fractures are an extremely common injury seen in orthopedics and are associated with significant morbidity and mortality. They most often occur in elderly patients after grounds level falls, are much more common in women than men, and occur more commonly in patients with osteoporosis. Patients who suffer hip fractures are at increased risk for many complications, including deep vein thrombosis, pulmonary embolism, pneumonia, deconditioning, pressure sores, and even death, as the mortality rate in the first year following a hip fracture is around 25%. One of the most important reasons for performing surgery is to prevent these complications, and getting patients out of bed and walking as soon as possible diminishes their risk. Therefore, surgery is almost always the treatment of choice for hip fractures, and the type of surgery performed is determined by the anatomic location of the fracture and the fracture pattern. Surgery should be performed as soon as possible, typically within 24 to 48 hours; however, since many of these patients suffer other comorbidities, they must be properly medically optimized before surgery. The goals of surgery are to minimize pain, restore hip function, and allow early mobilization, the importance of which cannot be overemphasized. The functional outcome for patients following a hip fracture is largely based on their level of mobility and independence before their injury. Many patients become less independent, may require assistive devices to help them walk, and some may require a long-term nursing or rehabilitation facility.
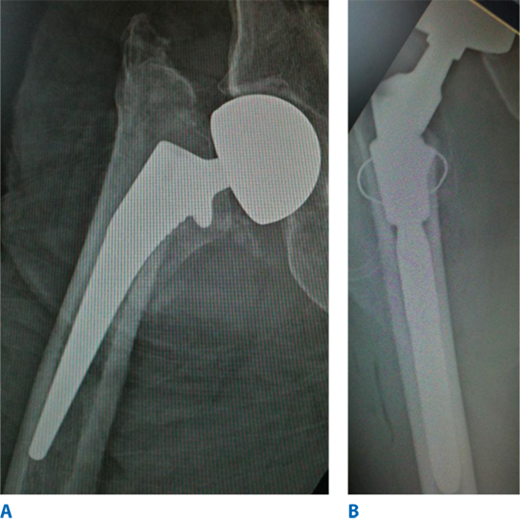
Femoral neck fractures occur with the capsule of the hip joint. The blood supply to the femoral neck and head comes from branches of the medial and lateral femoral circumflex arteries, which run along the femoral neck, and therefore fractures in this area put the vascular supply at risk and can lead to osteonecrosis. Femoral neck fractures that are nondisplaced have a low risk of disruption of blood flow and therefore can be treated with in situ internal fixation. Three cancellous screws are placed through a small incision over the lateral proximal femur, directed up through the femoral neck and into the femoral head. Patients can usually begin protected weight bearing immediately after surgery. Displaced femoral neck fractures will likely disrupt the blood supply and therefore need to be treated with a prosthetic replacement. Most commonly a hemiarthroplasty is performed in which the femoral neck and head are replaced with a metal stem into the femoral canal and a metal head (Fig. 43-5A). Patients who have severe osteoarthritis of the hip joint and had significant arthritic hip pain before their fracture may receive a total hip replacement, in which the acetabulum is also replaced with a prosthesis, typically a plastic cup inside a metal shell (Fig. 43-5B). Patients can begin weight bearing immediately after surgery.
Intertrochanteric Hip Fractures. Intertrochanteric hip fractures occur between the greater and lesser trochanters of the proximal femur. Because the blood supply to this area is abundant, osteonecrosis is uncommon and therefore these fractures can be fixed with internal fixation. Displaced fractures need to be realigned, and this involves placing the patient on a fracture table where traction and rotation can be applied to the affected leg to reduce the fracture. There are two devices that can be used. A sliding hip screw includes a large screw placed from the lateral cortex of the proximal femur across the fracture and into the femoral neck and head, followed by a side plate along with lateral cortex of the femur, which is then fixed to the shaft with screws. A cephalomedullary nail includes a nail placed down the medullary canal from the piriformis fossa and a large screw that engages the nail as it is passed from the lateral cortex up into the neck and head. Both devices form stable constructs (though the cephalomedullary nail is preferred for certain fracture patterns) and allow protected weight bearing postoperatively.
Subtrochanteric Hip Fractures. Subtrochanteric hip fractures occur in the proximal femoral shaft just distal to the lesser trochanter in an area of high biomechanical stresses. While they can occur in elderly patients after a fall, they are also seen in high energy trauma. Because of the forces of muscles attached to the fractured segments, they tend to be significantly displaced and it can be difficult to reduce these fractures. They are most often treated with a long cephalomedullary nail that includes a screw distally to lock the nail in place and prevent rotation of the femur. Fractures that cannot be reduced closed on a fracture table or that are severely comminuted require open reduction followed by a cephalomedullary nail or by a plate and screws that is placed over the lateral cortex of the femoral shaft. In most cases, protected weight bearing can begin soon after surgery.
Fractures of the femoral shaft are caused by high energy trauma and may be associated with other severe injuries. Long bone fractures, such as femoral shaft fractures, put these patients are risk for complications such as thromboembolic events and acute respiratory distress syndrome (ARDS), and therefore it is important to fix these quickly, typically within 24 hours. They are most commonly fixed with an intramedullary nail that can be placed antegrade (from the piriformis fossa or greater trochanter down the canal) or retrograde (through an incision into the knee joint and up the canal), with screws placed through proximal and distal holes to lock the nail in place, creating a stable fixation to allow weight bearing. Trauma patients who are hemodynamically unstable or who have other life-threatening injuries are treated temporarily with an external fixator until they can safely undergo surgery.
Distal femur fractures are the result of a fall from a height or from high-energy trauma. They can also occur in elderly patients with osteoporotic bone after a fall onto the knee. While nondisplaced fractures in the elderly may be treated nonoperatively with a hinged knee brace and motion exercises, most require surgery. These fractures can involve the articular surface of the knee joint, so anatomic reduction of the joint surface is crucial. They are fixed with plates and screws placed over the medial or lateral cortex, depending on the fracture pattern, and early knee range of motion is encouraged to prevent stiffness. These intra-articular fractures require the patient to be nonweight bearing until the fracture shows signs of healing.
Dislocation of the knee is a rare but devastating injury that can be limb-threatening. When the knee dislocates, the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) are torn, and various degrees of injury occur to the LCL, medial collateral ligament (MCL), posterolateral corner, joint capsule, and menisci. The danger however is due to the close proximity of the popliteal artery that runs directly behind the knee, which may kink or suffer a tear of the intimal wall when the knee dislocates. A neurovascular exam is extremely important, followed by immediate reduction of the knee and repeat exam of the pulses. If there is evidence of diminished or absent pulses, an angiogram must be performed, and vascular surgery may need to perform emergent vascular repair. With regard to the ligamentous injuries, an MRI will identify what structures have been torn. Because a dislocation causes so much damage to the knee, multiligamentous reconstruction is recommended in order to stabilize the knee joint. Stiffness and instability of the knee are common complications after this injury.
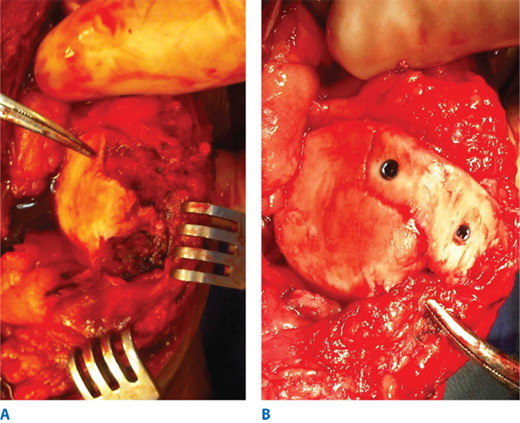
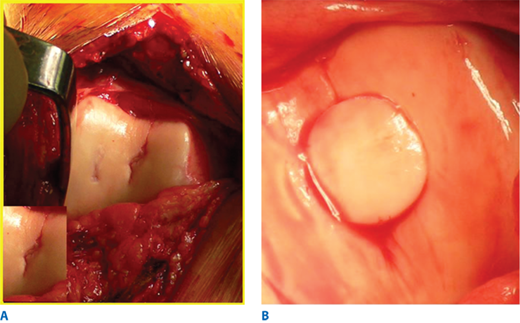
The extensor mechanism is comprised of the quadriceps tendon, the patella, and the patella ligament and functions to extend the knee. Injuries can result after a fall directly onto the knee or from forcible contraction of the quadriceps. It is important to examine the knee for the ability to actively extend the knee, since quadriceps tendon ruptures, patella fractures, or patella ligament ruptures can result in a loss of active knee extension, requiring surgery. Nondisplaced patella fractures can be treated nonoperatively with a cast or knee immobilizer, holding the knee in full extension, and weight bearing is permitted. Displaced or comminuted fractures require surgery with either tension band wiring or screws. Acute osteochondral fractures can be managed with internal fixation (Fig. 43-6A and B). Quadriceps tendon and patella ligament ruptures with loss of active knee extension are treated with suture repair. After surgery, the knee is held in extension and knee flexion is slowly increased over several weeks using a hinged knee brace.
Patella dislocations are common injuries that occur when the femur is forcibly internally rotated on an externally rotated tibia while the foot is planted on the ground. They typically dislocate laterally and often relocate spontaneously. Patients present with a significant knee effusion and on physical exam may elicit a positive apprehension test, in which a lateral force to the patella elicits pain and the sensation of an impending dislocation. Dislocated patellas can be reduced by extending the knee and manual reduction, and are treated with temporary knee immobilization. There is a high risk for recurrent dislocations, which may require surgical intervention. Osteochondral injuries to the trochlear groove and patella may be managed with the Draenert technique of autologous osteochondral transplant (Fig. 43-7A and B).
The tibial plateau is comprised of the articular surfaces and underlying cancellous bone of the medial and lateral plateaus of the proximal tibia. Fractures of the plateau result from axial loads sustained in falls from a height or high energy trauma, and are often associated with injuries to the menisci and cartilage of the knee. Fractures can involve the medial, lateral, or both plateaus with significant comminution, angulation, and depression, creating a challenging injury to fix. A CT scan is important to visualize the intra-articular involvement of the fracture. Minimally displaced fractures may be treated nonoperatively with strict nonweight bearing until the fracture heals. Fractures associated with displaced articular fragments require surgery in order to restore the smooth contour of the articular surface. They are treated with plates and screws placed medially, laterally, or both. Since there is often a depression of the cancellous bone, bone graft or bone substitutes may be needed to buttress the articular surface and restore the anatomic alignment of the tibia. Patients are kept strictly nonweight bearing for several weeks until the fracture begins to heal, though early range of motion is encouraged. Repair of ligament or meniscus injuries may also be indicated at the time of surgery. Knee stiffness and osteoarthritis are common complications of these injuries.
Tibial shaft fractures are the most common long bone fractures and they occur following high energy trauma, direct blows, and severe twisting injuries. Trauma and direct blows to the tibia result in transverse or comminuted fracture patterns, while torsional injuries cause spiral fractures. Fractures with minimal angulation can be treated with reduction and casting, followed by transition to a functional brace and slow return to weight bearing, and may need to be immobilized for several months since these fractures can be slow to heal. Most tibial shaft fractures, especially comminuted and angulated fractures, are treated with an intramedullary nail placed down the tibial canal, with interlocking screws placed proximally and distally, and weight bearing can begin soon after surgery. Plate and screw fixation can also be used, however since the tibia is subcutaneous, hardware placed along the shaft can increase the risk of wound breakdown, and therefore intramedullary nailing is the preferred treatment. Fibula shaft fractures often occur along with tibial shaft fractures, though they usually heal well without surgery.
The tibial plafond is the distal tibial articular surface of the ankle joint. Pilon fractures are typically high energy injuries from axial compression or a shear force. These injuries can cause significant soft tissue injury, severely comminuted intra-articular fragments, and wound healing problems, making these fractures very difficult to treat. Due to the soft tissue injury, these fractures are initially treated with external fixation until the swelling subsides, which may take several days to weeks. The goals of surgery are to restore the articular surface, fix the fibula in order to maintain and establish anatomic length, bone graft any cancellous bone defects, and stabilize the distal tibia with plate and screw fixation. Patients are kept nonweight bearing for many weeks until the fracture heals. Despite best efforts, patients may suffer from ankle pain and stiffness, arthritis, wound healing problems, infection, nonunion, and some patients eventually need ankle fusion in the future.
The ankle joint is a complex hinge joint comprised of the distal tibial plafond, medial malleolus, and lateral malleolus and their articulation with the talus. Several ligaments also contribute to the stability of the ankle joint, including the deltoid ligament medially, the syndesmotic ligaments between the tibia and fibula, and the anterior talofibular, posterior talofibular, and calcaneofibular ligaments laterally. Dislocations of the ankle joint result from a severe twisting injury and often occur with fractures. At times, dislocations can place significant pressure on the overlying skin and can cause neurovascular compromise, therefore prompt reduction is extremely important followed by splinting.
Ankle fractures are very common and result from a twisting injury to the ankle. The patterns of ankle fractures depend on the direction of force and the position of the foot and ankle at the time of injury. The goals of treating ankle fractures are to restore the anatomy of the ankle joint and to restore the length and rotation of the fibula. Initial treatment includes closed reduction and placement of a well-padded splint in order to protect the skin. Swelling can be a significant problem so elevation of the foot is encouraged. If surgery is to be performed, it is usually delayed 1 to 2 weeks until the swelling decreases to limit the risk of wound healing problems.
Isolated fractures of the lateral malleolus require anatomic reduction of the fracture in order to restore normal ankle joint congruity. The talus can sublux laterally following lateral malleolus fractures, and even 1 millimeter of talar shift decreases the surface contact between the talus and the tibia by 40%, increasing the risk of developing arthritis. Closed reduction and casting can be successful, however if the fracture cannot be adequately reduced, then open reduction internal fixation of the fibula is done with plate and screw fixation.
An isolated fracture of the medial malleolus is usually an avulsion-type injury. Minimally displaced fractures can be treated with a cast or walking boot, while displaced fractures are fixed with screws placed up through the tip of the malleolus.
Fractures to both the medial and lateral malleoli often require surgery. These injuries are more unstable and the talus will often sublux or completely dislocate laterally. They are treated by reducing and fixing both malleoli during surgery. Occasionally, the posterior articular surface of the distal tibia, or posterior malleolus, can be fractured as well, resulting in a trimalleolar ankle fracture. Often it is a small fragment and does not need to be fixed, however if it involves >25% of the articular surface it should be fixed with screws placed either anteriorly or posteriorly.
The syndesmosis is comprised of several ligaments between the distal tibia and fibula that provide stability to the ankle joint by resisting axial, rotational, and translational forces. The syndesmosis can be disrupted at the time of ankle fractures and requires special attention. Widening of the space between the distal tibia and fibula after fixing the fractures is indicative of a syndesmosis injury and it is treated with 1 or 2 screws placed laterally from the fibula into the tibia, parallel to the ankle joint. Patients are kept non-weight bearing for several weeks. The screws are often removed after 12 weeks, though they can be left in place and are typically asymptomatic.
Calcaneal fractures occur following a fall from a height and are often associated with other injuries, including lumbar spine fractures. These injuries are often intra-articular and can result in collapse of weight-bearing posterior facet of the calcaneous. CT scans are useful to better visualize the fracture pattern. Most fractures can be treated nonoperatively in a well-padded splint and patients are kept nonweight bearing for up to 12 weeks. Displaced intraarticular fractures can be treated surgically once the swelling subsides with lag screws or with a thin plate and screw fixation. Despite adequate treatment, calcaneal fractures can be debilitating injuries, leading to significant heel pain and arthritis.
Fractures of the talus commonly result from forced dorsiflexion of the ankle, causing the talar neck to impact on the anterior distal tibia. The blood supply to the talus can be jeopardized after a fracture and may lead to osteonecrosis, which is an unfortunately common complication following talus fractures. Nondisplaced fractures are treated with a cast and have a 15% risk of osteonecrosis, while displaced fractures are often treated surgically with screw fixation. There is a high risk of osteonecrosis, ranging from 30% to 100%, and a high risk of arthritis.
The tarsal bones, including the navicular, the cuboid, and the three cuneiform bones, link the hind foot to the metatarsals and provide mechanical stability to the arch of the foot. Isolated fractures to these bones are rare and are often treated nonoperatively with a cast or boot. The Lisfranc ligament, which connects the 2nd metatarsal head to the medial cuneiform, is an important stabilizer of the midfoot. Lisfranc injuries can be seen following torsional forces to the foot or from crush injuries. These injuries often require surgery since anatomic reduction is extremely important for a successful outcome. Metatarsal fractures similarly result from twisting or crush injuries and most can be treated nonoperatively with a hard-soled shoe and weight bearing as tolerated. The base of the 5th metatarsal, however, warrants close attention. Fractures at the metaphyseal-diaphyseal junction of the proximal 5th metatarsal (Jones fractures) can jeopardize blood flow and are at risk for nonunion. Therefore, Jones fractures need close follow-up to assess for healing and may need screw fixation. Injuries to the metatarsal-phalangeal joints and phalangeal fractures can be treated symptomatically or with buddy taping with weight bearing as tolerated in a hard-soled shoe.
INTRODUCTION
Sports medicine deals with the prevention and treatment of injuries related to sports and exercise. These injuries encompass various areas in the musculoskeletal system. In recent years, sports-related injuries have increased and the sports medicine field has been expanding. The growth in sports and sports-related injuries has likely to do with: a) that athletes participate in sport-specific training year round (and in multiple sports) rather than just seasonal training, b) that there has been an increase in “weekend warriors,” c) that patients have become more aware of physical fitness, are better educated, and have higher performance expectations, and d) that more people undertake recreational activities.
The orthopedic subspecialty of sports medicine treats a broad spectrum of patients, ranging from children who have just started participating in their first sports to the specialized care of professional athletes. Medical treatment of athletes, recreational or professional, can be complex as short- and long-term outcomes are influenced by the higher demand that athletes put on their bodies. Additionally, the orthopedic sports medicine specialist does not only treat the patient’s injuries, but also has to consider the return to activity in a later stadium. “Getting back in the game” is sometimes subject to pressure from third parties (e.g., team members, coaches, parents, fans), which makes treatment and the rehabilitation a challenging process.
Surgical intervention for ligament and cartilage injuries in sports medicine patients is usually done using arthroscopic techniques. The most frequently injured joints are the shoulder, hip and knee. Therefore, treatment of common injuries in these joints will be the scope of this paragraph.
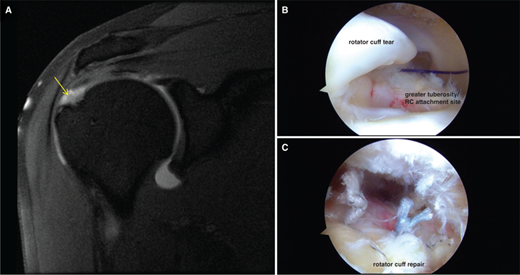
SHOULDER
Rotator cuff injuries are among the most common reasons to visit an orthopedic sports specialist. Often, these injuries are associated with either forceful or repeated overhead or pulling movements. The rotator cuff provides shoulder movement and glenohumeral joint stability and injuries typically lead to pain, weakness and restricted movement of the arm. Over recent years, the treatment of the rotator cuff injuries has considerably improved with regard to indication for surgery, surgical techniques and rehabilitation protocols. With the introduction of arthroscopy, shoulder surgery has become less invasive with all advantages associated. Currently, it has been established that arthroscopic techniques are equal or superior to open techniques for most indications. Controversies surrounding rotator cuff repair remain and include, but are not limited to, use of acromioplasty, enhancement of healing with orthobiologics (Fig. 43-8), single- vs. double-row fixation and the treatment of massive or large tears. Rehabilitation after surgery plays an important role to restore strength, motion and function and to enable the patient to return to sports. Typically, rehabilitation is made up of three consecutive stages: immobilization, passive exercise, and active exercise. Immobilization and passive exercise usually start in the first 4 to 6 weeks after surgery. Immobilization can be established by using a sling and passive exercise should be initiated by the therapist. The therapist moves the arm in different positions to improve range of motion (ROM) while providing support. After 4 to 6 weeks, active exercises can be gradually introduced. At 8 to 12 weeks, muscle strength and improvement of arm control are increased by starting a strengthening exercise program.
Figure 43-8.
Imaging and treatment of rotator cuff tears. A. MRI coronal T2 image showing a full-thickness and moderately retracted tear (arrow) of the supraspinatus tendon. B. Arthroscopic image showing the supraspinatus tendon tear as viewed from a posterior portal during the surgery. C. Arthroscopic image showing completion of repair of the supraspinatus tendon tear using suture anchors imbedded in the greater tuberosity of the humerus and attached sutures that capture and reduce the torn tendon to its native insertion site.
The most common etiology for shoulder instability is related to trauma, especially shoulder dislocation. After a shoulder has dislocated, it becomes vulnerable to repeat episodes of instability and may develop to being a chronic problem. Most of the shoulder’s stability is provided by the rotator cuff and shoulder capsule. The most common dislocation is in the anterior-inferior direction, although posterior dislocations do occur. Typically, patients with an anterior dislocation present with pain and an internally rotated shoulder. Younger patients are more susceptible to suffer from repeat dislocations than older patients.6,7,8 The position of the humeral head with respect to the glenoid and other bony pathology can be identified with radiographs. Views from different angles should be obtained to thoroughly evaluate; an anterior-posterior (AP) view, along with glenoid (axillary) view, and a “ Y” view of the shoulder are recommended in assessing this injury. Since most of the shoulder’s stability is provided by soft tissue, usually this is also injured. Following successful reduction magnetic resonance imaging (MRI) should be obtained to identify underlying causes and concomitant injuries.
Relocation of the shoulder is generally accomplished with the patient in supine position and the arm under gentle traction and slight abduction. Some sedation is helpful as it relaxes the patient’s musculature and relieves the pain. Whether or not to immobilize a first-time-dislocated shoulder or not, remains controversial, as well as the position of immobilization or the early surgical repair of capsulolabral structures. Prolonged immobilization is not recommended since this will often lead to substantial stiffness in the shoulder and does not appreciably decrease the redislocation rate. A small minority of patients with atraumatic multidirectional instability can generally be treated with shoulder rehabilitation. Unfortunately, many patients experience recurrent dislocations, in which case surgical stabilization of the shoulder should be considered. Many open stabilizing procedures have been described and, depending on etiology, many are still being applied such as the open Bankart repair, Latarjet procedure, remplissage and humeral head restoration. However, arthroscopic soft-tissue restoration has been the front-line treatment for recurrent instability. After surgery, the shoulder is temporarily immobilized with a sling. When the sling is removed, exercises to rehabilitate the ligaments, improve ROM and prevent from scarring, will be started. Strengthening exercises will gradually be added to the rehabilitation plan.
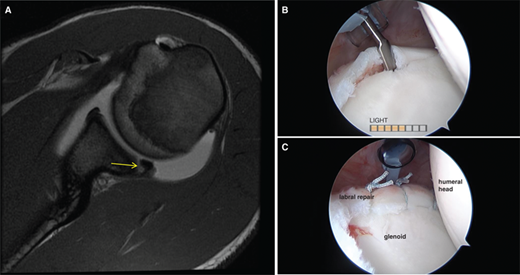
The labrum helps to deepen the socket and stabilizes the glenohumeral joint. Additionally, it serves as an attachment point for many of the shoulder ligaments, as well one of the biceps tendons. A superior labrum anterior and posterior lesion may occur in the superior part of the labrum, usually anterior and posterior to the attachment of the biceps tendon, with occasional involvement of the biceps tendon in certain cases. Injuries to the superior labrum can be caused by trauma or by repetitive shoulder motion. Radiographs are generally obtained to evaluate for concomitant injuries or osteoarthritic changes. The labrum itself, and other soft tissue, is better visualized with MRI with addition of a gadolinium arthrogram adding sensitivity for labral injury detection (Fig. 43-9).
Figure 43-9.
Imaging and treatment of a shoulder glenoid labrum tear. A. MRI axial T1 image showing a tear of the posterior superior labrum (arrow). B. Arthroscopic image with the patient in the lateral decubitus position showing detachment of the torn labrum away from the glenoid. C. Arthroscopic image demonstrating repair of the labrum to its attachment site using anchors in the glenoid and sutures that fixes the labrum to the glenoid.
Conservative and operative treatments have had mixed results depending on the patient’s age, activity level, type of tear and presence of concomitant injuries. If symptoms do not improve with adequate physical therapy and/or nonsteroidal anti-inflammatory drugs (NSAIDs), surgical intervention is usually indicated. Some SLAP injuries involve the biceps tendon, which may require either tenotomy or tenodesis.10,11
After surgical labrum repair, the shoulder needs to be immobilized to protect the repair and allow for healing. Usually a sling is used for 4 weeks after surgery. Then a physical therapy program will gradually start improving ROM and prevent from scar formation and stiffness to develop. As healing progresses, exercises to strengthen the shoulder muscles and the rotator cuff will gradually be added to the program around 4 to 6 weeks after surgery. Return to early interval throwing can generally be allowed around 3 to 4 months after surgery.
After minor trauma or repetitive injury, patients may experience pain and discomfort which can be due to irritation of the tissues in the subacromial space. In many cases these shoulder impingement syndromes are caused by simple bursitis or tendonitis of the long head of the biceps or supraspinatus tendon.5 Occasionally, impingement syndromes can progress to tears of the supraspinatus tendon, which can be confirmed by MRI or ultrasound.
The goal of treatment is to reduce pain and restore function. Initial treatment is generally nonsurgical and based on rest,NSAIDs, and physical therapy. If pain is not relieved, an injection of a local anesthetic and a cortisone preparation may be helpful.
If conservative treatment does not relieve pain, surgery is recommended, with the goal to excise the bursa and create more subacromial space. Generally, surgery is performed arthroscopically and encompasses bursectomy and subacromial decompression via acromioplasty. If the rotator cuff (supraspinatus tendon) is also injured, arthroscopic repair is usually indicated to restore function, sometimes is accompanied by a bony resection of the inferior portion of the acromion.
The acromioclavicular joint is a gliding synovial joint and not very mobile. The joint is stabilized by three ligaments: the superior acromioclavicular ligament, the inferior acromioclavicular ligament, and the coracoclavicular ligament. Injuries to these ligaments are commonly sustained playing contact sports such as football and ice hockey and may cause displacement of the joint. An acromioclavicular sprain is referred to as a shoulder separation and type I and II are usually treated symptomatic. Controversy exists however regarding early or delayed surgical reconstruction for type III tears. Frank tearing of the coracoclavicular ligaments, associated with significant displacement, is oftentimes reconstructed surgically.
KNEE
The knee is the largest joint in the human body and is a pivotal hinge joint, which allows flexion and extension as well as a medial and lateral rotation. The knee bears tremendous axial loads as well as torsional and sheer forces, making it vulnerable to both acute injury and the development of osteoarthritis. In sports, the major stabilizing structures such as the ACL and the medial collateral ligament (MCL) are frequently injured. Other frequent knee injuries are to the menisci, posterolateral corner, the posterior cruciate ligament (PCL) or patellofemoral.
The menisci are crescent-shaped pieces of fibrocartilage shaped that provide joint stability, shock absorption, load distribution, and proprioception. Sudden meniscal tears often happen during sports, usually during contact or while squatting and twisting the knee. Typical symptoms associated with meniscus injury are pain, stiffness and swelling, catching or locking of the knee, buckling or “ giving way” and impaired ROM. Radiographs are typically obtained to assess possible concomitant injuries, the presence of (early) osteoarthritis, and leg alignment. However, since menisci do not show on radiographs, an MRI is obtained to assess the status of the menisci and the soft tissue surrounding the knee joint (Fig. 43-10). Small tears on the outer edge of the meniscus may not cause symptoms and—provided the knee is stable—nonsurgical treatment may be sufficient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree