Operations for Zenker’s Diverticulum
Zenker’s diverticulum is an outpouching of the cervical esophagus. Mucosa of the esophagus protrudes through an anatomically weak area between the cricopharyngeus inferiorly and the thyropharyngeus, both parts of the inferior pharyngeal constrictor, superiorly. Although this weak spot is posterior, the diverticulum generally is approached through the left neck, where it presents most commonly.
The pathogenesis of Zenker’s diverticulum is not fully understood. Spasms of the cricopharyngeus muscle are believed to cause functional obstruction with secondary protrusion of the esophageal mucosa through a weak area. Cricopharyngeal myotomy (division of the muscle) is a critical component of successful repair. When the diverticulum is small, myotomy alone may suffice. However, a large diverticulum generally requires excision of the sac, as well as myotomy. In this chapter, two procedures are described. The first is the classic open single-stage diverticulectomy with cricopharyngeal myotomy. The second is an endoscopic transoral stapling procedure.
Steps in Procedure—open Diverticulectomy
Make incision along anterior border of left sternocleidomastoid muscle
Expose anterior border of sternocleidomastoid
Retract sternocleidomastoid muscle and carotid sheath laterally
Retract omohyoid muscle medially or divide it
Divide middle thyroid vein and mobilize thyroid medially
Expose posterior trachea and esophagus
Identify esophagus by palpation and seek diverticulum
Place Babcock clamps on diverticulum and retract it cephalad
Divide cricopharyngeus muscle
Amputate diverticulum with stapler or sutures
Close muscle over suture line
Place small, soft drain and close incision in layers
Hallmark Anatomic Complications—Open Diverticulectomy
Inadequate myotomy
Injury to esophagus
Leakage from suture or staple line
List of Structures
Pharynx
Inferior pharyngeal constrictor
Cricopharyngeus
Thyropharyngeus
Esophagus
Sternocleidomastoid muscle
Omohyoid muscle
Sternohyoid muscle
Thyroid gland
Thyroid cartilage
Middle thyroid vein
Inferior thyroid artery
Carotid sheath
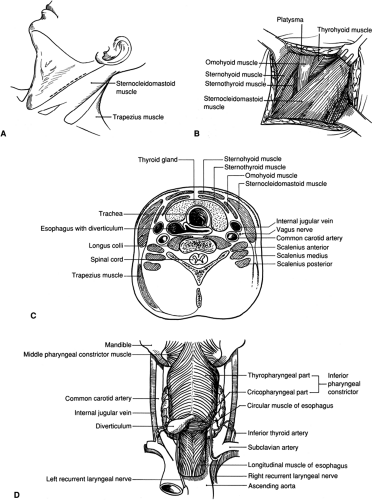
Open Diverticulectomy—Position of the Patient and Skin Incision (Fig. 12.1)
Technical Points
Position the patient supine with the head turned slightly to the right. Make an incision along the anterior border of the ster-nocleidomastoid muscle. An alternative collar-type incision is preferred by some surgeons for an improved cosmetic result. This incision is made at the level of the cricoid cartilage, and skin flaps are elevated to expose the anterior border of the sternocleidomastoid muscle.
Anatomic Points
A pharyngoesophageal (Zenker’s) diverticulum is a pulsion diverticulum through the inherently weak area of the hypopharynx and upper esophagus. These diverticula occur most commonly
in the region of the cricopharyngeus, a part of the inferior pharyngeal constrictor. A more precise description of the location of such diverticula is impossible owing to the variability in the exact anatomy of the region or to our lack of understanding of the etiology of this disease. Several features of the distal pharynx and proximal esophagus provide an anatomic basis for such pulsion diverticula. Some investigators believe that there is a zone of potential weakness between the cricopharyngeus muscle and the immediately superior thyropharyngeus muscle (again, a part of the inferior constrictor muscle). Other surgeons believe that the zone of weakness is between the superior and inferior parts of the cricopharyngeus itself. (Allegedly, the upper constrictor part is innervated by vagal fibers passing through the pharyngeal plexus, whereas the lower sphincteric part receives its vagal innervation through the recurrent laryngeal nerve.) A third hypothesis is that these diverticula arise in the inverted triangular area bounded laterally by diverging longitudinal esophageal muscle fibers passing to their attachment on the cricoid and superiorly by the inferior border of the cricopharyngeus. In this triangle (the so-called Laimer’s area), circular muscle fibers are the sole dynamic covering of the esophagus. Finally, some researchers believe that the diverticulum arises at the point where the pharyngeal branches of the superior or inferior thyroid artery penetrate the pharyngeal wall. Regardless of the exact location of the diverticulum’s origin, most frequently it protrudes toward the left; thus, the initial incision typically is on the left side of the neck.
in the region of the cricopharyngeus, a part of the inferior pharyngeal constrictor. A more precise description of the location of such diverticula is impossible owing to the variability in the exact anatomy of the region or to our lack of understanding of the etiology of this disease. Several features of the distal pharynx and proximal esophagus provide an anatomic basis for such pulsion diverticula. Some investigators believe that there is a zone of potential weakness between the cricopharyngeus muscle and the immediately superior thyropharyngeus muscle (again, a part of the inferior constrictor muscle). Other surgeons believe that the zone of weakness is between the superior and inferior parts of the cricopharyngeus itself. (Allegedly, the upper constrictor part is innervated by vagal fibers passing through the pharyngeal plexus, whereas the lower sphincteric part receives its vagal innervation through the recurrent laryngeal nerve.) A third hypothesis is that these diverticula arise in the inverted triangular area bounded laterally by diverging longitudinal esophageal muscle fibers passing to their attachment on the cricoid and superiorly by the inferior border of the cricopharyngeus. In this triangle (the so-called Laimer’s area), circular muscle fibers are the sole dynamic covering of the esophagus. Finally, some researchers believe that the diverticulum arises at the point where the pharyngeal branches of the superior or inferior thyroid artery penetrate the pharyngeal wall. Regardless of the exact location of the diverticulum’s origin, most frequently it protrudes toward the left; thus, the initial incision typically is on the left side of the neck.
A skin incision that parallels the anterior border of the sternocleidomastoid muscle will divide twigs of the transverse cervical (anterior cutaneous) nerve, a branch of the cervical plexus containing sensory fibers of C2 and C3. The main trunk of this nerve is located immediately posterior to the middle of the sternocleidomastoid muscle. It bends anteriorly, passing in the plane deep to the platysma and superficial to the sternocleidomastoid muscle, on whose surface it branches to supply most of the skin of the anterior neck. The platysma muscle, innervated by the cervical branch of cranial nerve VII, should be divided in the same direction as the skin. An attempt should be made to spare the larger ramifications of the transverse cervical nerve. The alternative, a collar incision, is made through the skin and platysma in a horizontal (transverse) plane. As is the case with any skin incision, those that are parallel to cleavage lines or skin creases tend to produce a more cosmetically acceptable scar. Deep to the platysma, ramifications of the transverse cervical nerve will again be divided, but it should be easy to avoid major divisions of the transverse cervical nerve.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree