Open Repair of Ventral Hernias
Evgeny V. Arshava
Ventral hernias are classified as either spontaneous (epigastric, umbilical, Spigelian, lumbar) or postoperative. Most ventral hernias are postoperative (incisional) and occur at the site of previous laparotomy incisions. Many asymptomatic and minimally symptomatic hernias, especially with large defects in high risk patients, may be safely observed. Most symptomatic hernias are usually repaired electively. Others present with an acute incarceration and may need to be operated on urgently. Always optimize medical comorbidities, encourage smoking cessation and, if necessary, weight loss before the elective operation.
Multiple repairs have been described and none are perfect. Choice of repair depends on the size of the defect, tissue quality, comorbidities of the patient, previous surgical history and circumstances of the operation. Small defects may be closed by reopening the incision, clearing and reapproximating the fascial edges as one would close the laparotomy incision. Frequently, multiple defects may be present; thus, it is important to explore the entire incision. If the fascial defect is large and closure cannot be accomplished without excessive tension, synthetic or biologic implants may need to be used for a durable repair. A variety of such implants are available, each with its own advantages and disadvantages. It is important to be familiar with characteristics of these different products, since one mesh does not serve all purposes.
Tailor the implant to the specific patient and circumstances of the operation. For example, synthetic materials are contraindicated in the contaminated field (active infection, bowel resection, or history of infection) at the site. To cite another example, mesh without nonadhesive layer should not be used in direct apposition to the bowel.
The technique of separation of components lengthens the musculoaponeurotic flaps, allowing them to reach the midline, and may be used in combination with or as an alternative to placement of an implant.
This chapter highlights the anatomy of the abdominal wall and describes contemporary open approaches to the management of ventral hernias. The wide variety of techniques available attests to difficulties with recurrence even after the most meticulous repair. Literature sources discussing further details on various techniques, outcomes and materials are referenced at the end.
Laparoscopic ventral hernia repair is an increasingly popular alternative to an open herniorrhaphy with improved outcomes in selected patients (see Chapter 49). The laparoscopic approach should not be used for hernia defects larger than 10 cm.
SCORE™, the Surgical Council on Resident Education, classified open repair of ventral hernia as an “ESSENTIAL COMMON” procedure. SCORE™ classified component separation abdominal wall reconstruction and repair of miscellaneous hernias as “ESSENTIAL UNCOMMON” procedures.
STEPS IN PROCEDURE
Make incision over the hernia (usually through old scar) with extension beyond it
Try to stay in preperitoneal plane to avoid damage to adherent bowel
Raise skin flaps in all directions for adequate exploration and identification of all defects
Reduce the hernia and free the fascial edges from adhesions. Preserve the hernia sac if possible
Choose method of repair—avoid the use of prosthetic material if reasonable
Primary Repair
Close the facial defect in the direction of the least tension
Repair by Separation of Components
Widely develop skin flaps or alternatively perform short lateral counter incisions
Create relaxing incisions through the EOA
Close fascia in the midline
Place closed suction drains under skin flaps
Repair with the Prosthetic or Biologic Implant
Secure the mesh to fascia
Close fascia over implant if possible
Umbilical Hernia Repair
Make incision in umbilical crease or excise the stretched skin as needed
Identify and reduce hernia contents. Preserve sac if possible
Close fascia in the direction of least tension
Use prosthetic for a large defect
Tack underside of umbilicus to fascia to recreate normal appearance
HALLMARK ANATOMIC COMPLICATIONS
Surgical site infection
Injury to bowel during dissection
Recurrence due to excessive tension during closure or to unidentified secondary defects
The anatomy of the abdominal wall is complex. The abdominal wall layers are shown in Figure 47.1.
The terminology used in the literature for description of subcutaneous tissue is not consistent and may be confusing. The superficial fascia (Scarpa’s) is a distinct fibrous layer identifiable during dissection and imaging. This membranous layer stretches across entire abdomen and continues on to the back toward the spinous processes. It is less distinct along the midline and around umbilicus. In most individuals, the superficial adipose layer (frequently referred to as Camper’s fascia) is thicker, consists of large fat lobes with high structural stability and elastic properties, and is encased in between the perpendicular oriented fibrous septa. The deep adipose layer has smaller fat lobes that deform much easier and may not be well developed in slender individuals. Obliquely oriented deep fibrous septa make this layer more amenable to surgical separation during dissection and are prone to traumatic separation (degloving) from the underlying muscle.
Paired rectus abdominis muscles, “masters of the abdomen,” form the spine of the abdominal musculature. They stretch from the xiphoid process and fifth, sixth, and seventh ribs to the symphysis crest. They are joined in the midline by the linea alba. The linea alba is a continuous aponeurotic bridge, stretched from the xiphoid process to the symphysis pubis that joins musculoaponeurotic structure of both sides. It is recognized by the intersection of crossing fibers (“decussation”) from each side. Overall, the linea alba is wider above the umbilicus, making initial laparotomy access on virgin abdomen easiest in this location. Insignificant pyramidalis muscles are found next to the lower part of the recti muscles, attach to the pubic crest and insert to the linea alba as well.
The external oblique muscle is the most superficial of the three flat lateral muscles. Superiorly, the muscular part attaches to the lower eight ribs intertwining with the bellies of the serratus anterior and latissimus dorsi muscles. Inferiorly, muscle fibers descend onto the iliac crest. While its muscular part occupies the lateral region of the abdomen, its aponeurosis extends medially, joining the fibers from the opposite side in the midline at the linea alba. Superiorly, aponeurosis extends over the costal margin, fusing with the origin of lower fibers of the pectoralis major muscle. Inferiorly, aponeurosis extends from pubic tubercle to the anterior superior iliac spine forming the inguinal ligament.
The internal oblique muscle is thinner and smaller than the external one. Its muscle fibers arise and run in a fan-like manner from the lower three ribs, thoracolumbar fascia, iliac crest and the lateral half of the inguinal ligament. Its aponeurosis is narrow. In the inguinal canal, it gives origin to the cremaster muscle. Medially, it continues into a narrow aponeurosis along the lateral border of rectus muscle.
The transversus abdominis muscle is the most internal of the flat muscles. Its muscle fibers arise from the cartilages of the lower six ribs, lumbodorsal fascia, iliac crest and lateral third of the inguinal ligament. Medially it forms aponeurosis, almost as wide as an external oblique one. Above the internal ring, the dense lower edge of the transversus aponeurosis is supplemented by the mostly fleshy lower edge of the internal oblique muscle to form the falx inguinalis and the “roof” of the inguinal canal.
Together all three flat abdominal muscles form the sheath of the rectus muscles. The tendinous line along the lateral edge of rectus muscle stretches from the cartilage of the ninth rib to the pubic tubercle and is called linea semilunaris. In the upper abdomen, the aponeuroses of the internal oblique muscle split at the linea semilunaris into anterior and posterior layers and fuse around each rectus muscle with other flat muscles forming a dense sheath joined together by the linea alba. In the lower abdomen, all three aponeuroses pass completely anterior to the rectus muscle. This transition occurs along the concave arcuate (semicircular) line (Fig. 47.10A). The top of this arch is usually located 3 to 5 cm below the umbilicus. The absence of the posterior rectus sheath below the arcuate line makes the structure of the lower abdomen relatively deficient. The point of intersection of arcuate and semilunaris lines is the classic location of Spigelian hernias (discussed briefly in the end).
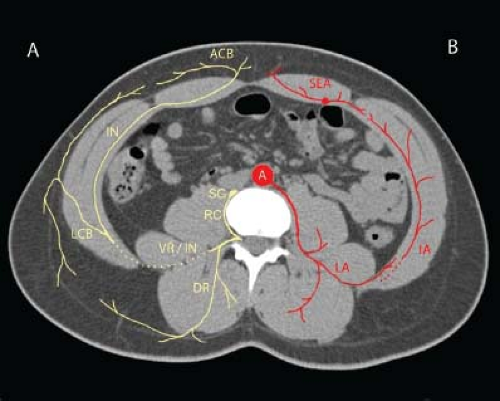
The abdominal wall is innervated by the lower five intercostal nerves (T7 to T11), subcostal (T12), iliohypogastric (T12 / L1) and ilioinguinal (L1) nerves. The intercostal nerves travel within the chest between the innermost intercostal and internal intercostal muscles. Within the abdominal wall, this plane naturally continues between the internal oblique and transversus abdominis muscles (Fig. 47.2A). The subcostal, ilioinguinal and iliohypogastric nerves, before piercing the the transversus abdominis muscle, travel within the abdomen on top of the quadratus lumborum muscle. Along the anterior axillary line, intercostal nerves give off the lateral cutaneous branches that penetrate the musculature and branches within the subcutaneous plane. Intercostal and other nerves, as they travel between internal oblique and transversus abdominis muscles, innervate flat muscles. Medially, the nerves penetrate posterior rectus sheath, innervate rectus muscle and then exit through the anterior sheath under the skin as sensory anterior cutaneous branches.
The rectus abdominis muscles are supplied by the superior and inferior epigastric vessels that travel within the rectus sheath and anastomose in the periumbilical area. Below the arcuate line, the inferior epigastric vessels lie directly on the posterior surface of rectus muscle and may be subject to injury during open or laparoscopic procedures.
The flat muscles of the abdomen are supplied by the rich network of lower intercostal, subcostal, musculophrenic, lumbar and deep circumflex iliac arterial and venous branches. This network is located between internal oblique and transversus abdominis muscles, giving off perforating vessels to surrounding tissues. This network also anastomoses with epigastric vessels through perforators in the rectus sheath. Such abundant blood supply makes bleeding complications much more likely than ischemic (Fig. 47.2B).
It is thus clear that oblique and lateral transverse incisions through flat muscles divide nerves and may not only produce sensory disturbances, but also denervate muscles and may result in bothersome bulges. This is the anatomic reason that the division of the external oblique aponeurosis during components separation, with preservation of the internal oblique muscles, does not disturb underlying nerves and blood supply of the abdominal wall.
Ventral Hernia Repair
Selected small hernias may be repaired under local and spinal anesthesia. Large defects require general anesthesia with muscle relaxation and appropriate lines and tubes. Meticulous skin preparation and draping are essential. Consideration using transparent incise drapes, especially if there is a possibility of using the synthetic mesh. Appropriate intravenous antibiotics should be completed within 1 hour prior to the incision. Mechanical bowel preparation may be considered for some cases to decrease abdominal distention. Preoperative computed tomography of the abdomen may be very helpful for preoperative planning in complex cases to evaluate the location of the fascial defects, integrity of the linea semilunaris, rectus and oblique muscles in order to choose the appropriate method of repair.
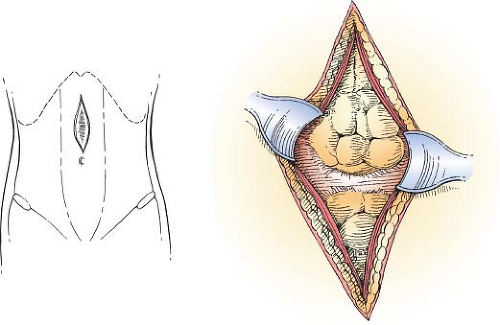
Exposure of Fascia and Definition of the Defect (Fig. 47.3)
Most commonly the skin incision is performed over the existing scar. Elliptic excision of the wide scar frequently facilitates healing of the wound and improves the postoperative appearance. In cases of palpable Spigelian and epigastric hernia, it may be acceptable to orient the incision transversely in the direction of the relaxed skin tension lines. In selected cases, abdominal panniculectomy may be performed simultaneously during the same operation.
Deepen the incision cautiously until the hernia sac is encountered. Often, the sac lies quite close to the skin surface and may be adherent to the old scar. Usually the plane around the hernia is avascular and easy to dissect. Herniation of the preperitoneal fat in the absence of true sac looks somewhat like a lipoma and is easily “shelled out” of the surrounding tissues as well. Dissect circumferentially around the sac and then down to the fascia to visualize the hernia neck. Clean the intact fascia around the edge of the defect, raising flaps of subcutaneous tissue and skin as far as needed. In most cases, the entire length of the old incision should be explored in order not to miss frequently coexisting multiple defects. Lateral defects, which may occur at points where previous retention sutures may have cut through the fascia, must be ruled out as well.
If possible, dissect the sac away from the fascia. Preserve or repair the sac and reduce it with the hernia. This allows totally extraperitoneal repair, if mesh is to be used. Frequently this is not possible and the hernia sac needs to be excised. Debride the hernia sac and scar tissue until healthy fascia is exposed circumferentially around entire defect. Both for primary and mesh repair, it is critical to clean the underside of the fascia carefully so that the bowel is not caught in a stitch during the repair.
Generally, multiple adjacent defects should be joined into a single one by dividing the intervening bridges.
Primary Closure of the Hernia Defect
If the defect is of a small (less than 3 cm) or long, but narrow, and there is no tension, it can be closed with nonabsorbable sutures in the direction of the least tension. Use of the running or interrupted closure depends on the surgeon’s preference. Either way suture length/wound length ratio should be at least 4:1. Be careful to avoid tension. If tension is required to appose the fascial edges, the repair will most likely fail. Remember that it is difficult to assess the tension of the repair under the conditions of muscle relaxation associated with general or spinal anesthesia. Therefore, if there is any tension or question about quality of the tissues, consider performing components separation or mesh repair.
Mesh Repair of Ventral Hernia (Figs. 47.4–47.6)
Use of mesh is associated with the improved success of repair of large ventral and recurrent incision hernia compared to primary closure technique. The most important prognostic factor for success may be the width of mesh overlap with the hernia defect. The circumferential, at least 5-cm overlap, is required for best outcomes.
The reduction of hernia and mobilization of the fascial edges are identical to primary repair.
Mesh can be used in several positions (Fig. 47.4). Neither overlay (Fig. 47.4A) nor inlay (Fig. 47.4B) positions are reliable and best avoided due to high failure rate. The underlay
position is associated with the lower recurrence rates and is currently the recommended approach. The so called “sandwich” (combination of the overlay and underlay meshes) repairs are rarely used at the present time.
position is associated with the lower recurrence rates and is currently the recommended approach. The so called “sandwich” (combination of the overlay and underlay meshes) repairs are rarely used at the present time.
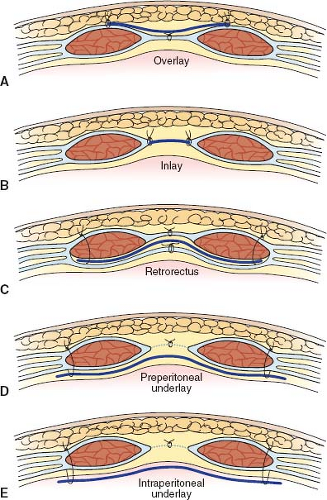 Figure 47.4 Mesh positions: A: Overlay (onlay). B: Inlay. C: Retrorectus. D: Preperitoneal (extraperitoneal) underlay. E: Intraperitoneal underlay. |
The underlay position may be further classified on the basis of its relationship to the peritoneum and fascia as intra- and extra-peritoneal and retrorectus positions. Erosion of the mesh into bowel and development of enteric fistulae may occur even years after the index operation. Thus, to decrease the risks of this devastating complication, do not place synthetic mesh, lacking a nonadherent layer or coating, in the intraperitoneal position against the viscera.
Retrorectus Mesh Repair
The classic retrorectus repair (Fig. 47.4C) is a very durable method with a low recurrence rate and avoids the contact of viscera with nonprotected meshes such as straight polypropylene and polyester. The edges of the rectus sheaths are incised with electrocautery on both sides of the defect for the full length of the defect. Dissect the plane to the lateral edge of the muscle between the posterior rectus sheath and muscle above the arcuate line and between the muscle and the peritoneum below it.
Sometimes, the integrity of the rectus muscle has been significantly compromised by previous operations and the width of the retrorectus plane is not sufficient for an optimal 4- to 5-cm mesh underlay. In such cases, the plane of the dissection needs to be continued outside of the rectus sheath. Two options exist for such cases. For the extraperitoneal position, incise the posterior rectus sheath medial to linea semilunaris and continue the plane of dissection between the peritoneum and the transversus abdominis muscle. For the intermuscular approach, incise the lateral edge of the rectus sheath and continue dissection in the plane between the transversus abdominis and internal oblique muscles. Note that the perforating vessels and nerve branches are encountered at the lateral edge and intermuscular extension of the retrorectus approach may permanently denervate the rectus muscles. To assure the adequate underlay both above and below the defect, continue dissection, if needed, behind the xiphoid and pubis. It is best to completely dissect the plane for mesh deployment before closing the posterior sheath to be able to repair defects in the peritoneum from inside of the abdomen and avoid injury to the underlying bowel.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree