An open neck exploration for hyperparathyroidism (HPT) is defined as exposure of an abnormal parathyroid gland or glands using standard operative techniques through a single incision without endoscopic or videoscopic assistance. This includes bilateral neck exploration for patients with multiglandular disease and unilateral focused parathyroidectomy with intraoperative parathyroid hormone (PTH) monitoring for a single adenoma localized preoperatively.
Primary HPT and malignancy account for 80% of all causes of hypercalcemia.
Primary HPT accounts for 50% to 60% of all cases of hypercalcemia diagnosed in an ambulatory setting and approximately 30% of cases diagnosed in a hospital setting.
There are many less common causes for hypercalcemia (Table 1).
In patients with primary HPT, 85% to 90% will have a single adenoma, 5% to 10% hyperplasia, 3% to 4% double adenoma, and less than 1% carcinoma.
Table 1: Causes of Hypercalcemia | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||
Primary HPT occurs in 1 out of every 500 women and 1 out of every 2,000 men. It most commonly occurs in women between the ages of 50 and 60 years.
Most patients with primary HPT are diagnosed as a result of the incidental hypercalcemia detected on blood work that is obtained for an unrelated medical problem. Patients often have nonspecific symptoms such as fatigue, weakness, constipation, and depression.
Patients with primary HPT may present with plethora of clinical manifestations (Table 2). Nephrolithiasis is the most common metabolic complication of primary HPT occurring in 15% to 20% of patients; however, only 2% to 5% of patients with kidney stones have primary HPT.
Approximately 3% of patients may present with hyperparathyroid crisis manifested by severe hypercalcemia (serum calcium >14 mg/dL), nausea, vomiting, dehydration, and central nervous system dysfunction including coma.1
Primary HPT is associated with a higher risk of cardiovascular disease and mortality that decreases after parathyroidectomy.2
A prior history of head or neck radiation in childhood, radioiodine treatment, and long-term lithium therapy are associated with a greater prevalence of primary HPT.
In 5% of patients, primary HPT is an inherited syndrome, underscoring the importance of obtaining a thorough family history. Familial HPT is inherited as an autosomal dominant
syndrome with primary HPT occurring as an isolated entity or as part of multiple endocrine neoplasia (MEN) I, MEN IIA, or the hyperparathyroidism-jaw tumor syndrome (Table 3). Patients with hyperparathyroidism-jaw tumor syndrome have more severe hypercalcemia and a 10% to 15% incidence of parathyroid cancer.
Table 2: Clinical Manifestation of Primary Hyperparathyroidism
Renal
Psychiatric
Nephrolithiasis
Nephrocalcinosis
Polyuria
Renal insufficiency
Depression
Lethargy
Memory loss
Confusion
Hallucinations
Coma
Skeletal
Neuromuscular
Generalized bone or joint pain
Osteopenia
Osteoporosis
Gout
Pseudogout
Pathologic bone fracture
Osteitis fibrosa cystica
Fatigue
Weakness
Malaise
Gastrointestinal
Cardiovascular
Constipation
Peptic ulcer disease
Pancreatitis
Nausea
Vomiting
Abdominal pain
Exacerbation of hypertension
Cardiac calcification
Left ventricular hypertrophy
Decreased QT interval
Conduction abnormalities
Heart block
Table 3: Familial Hyperparathyroidism
A. Familial isolated hyperparathyroidism
B. MEN I
Primary hyperparathyroidism
Gastroenteropancreatic tumors
Pituitary adenoma
Adrenocortical and thyroid tumors
Lipomas
Meningiomas
Facial angiofibromas
Bronchial, gastric, and thymic carcinoid tumors
C. MEN IIA
Medullary thyroid cancer
Pheochromocytoma
Primary hyperparathyroidism
Lichen planus amyloidosis
Hirschsprung disease
D. Hyperparathyroidism-jaw tumor syndrome
Ossifying fibromas of the mandible or maxilla
Renal cysts, hamartomas, and Wilms tumor
Uterine adenosarcoma, adenofibroma, leiomyoma, adenomyosis, and endometrial hyperplasia
In most patients with primary HPT, the physical examination is normal. Less than 5% of patients with primary HPT will have a palpable parathyroid tumor. Patients with hyperparathyroid crisis are more likely to have a palpable neck mass.
A palpable neck mass in patients with primary HPT should raise suspicion for parathyroid cancer or an associated thyroid nodule.
Rare patients may have band keratopathy, a condition characterized by calcium phosphate deposition in the cornea, which can be identified by slit lamp examination.
A diagnosis of primary HPT is made by an elevated serum calcium level and an elevated or inappropriately normal intact serum PTH level.
Up to 20% of patients have normocalcemic primary HPT with a serum calcium level in the normal range. Most patients with normocalcemic primary HPT are diagnosed as a result of evaluation for kidney stones, osteoporosis, or osteopenia. Vitamin D deficiency, excess phosphate intake, low calcium set point, and hypo- or hypermagnesemia may be contributory factors to normocalcemic HPT.
Patients with primary HPT may have low or low normal serum phosphate and high serum chloride, alkaline phosphatase, and uric acid levels. Alkaline phosphatase is elevated in patients with bone disease.
Patients may also have a mild metabolic acidosis, which occurs because of the inhibitory effect of PTH on phosphorus and bicarbonate reabsorption in the kidney.
Prior to the introduction of sensitive immunoradiometric and chemiluminescence assays for measurement of intact PTH levels, a chloride to phosphorus ratio greater than 33:1 was used to make the diagnosis of primary HPT.
Blood urea nitrogen, serum creatinine, and glomerular filtration rate should be measured and followed, because renal insufficiency is a known complication of primary HPT.
Bone mineral density should be measured at the lumbar spine, hip, and distal radius using dual energy x-ray absorptiometry.
A calcium:creatinine clearance ratio should be determined if familial hypocalciuric hypercalcemia (FHH) is suspected. FHH is a rare autosomal dominant disorder characterized by asymptomatic hypercalcemia, hypocalciuria, and variable PTH elevation that results from a higher renal setpoint for calcium secretion. Patients with FHH have one or more firstdegree relatives with hypercalcemia, a calcium:creatinine clearance less than 0.01, and a 24-hour urine calcium less than 100 mg. Parathyroidectomy is not indicated.
Once a diagnosis of primary HPT has been established, imaging should be performed to localize an abnormal parathyroid gland or glands. When an abnormal parathyroid gland can be localized preoperatively, a focused parathyroidectomy can be performed with intraoperative PTH measurement to confirm cure of the primary HPT. This minimizes dissection, shortens the operation, and reduces cost.
Localization studies should only be performed once a diagnosis of HPT has been established and a decision to proceed with surgical therapy has been made. The role of localization studies is to help determine the site of the incision and where in the neck to begin the exploration.
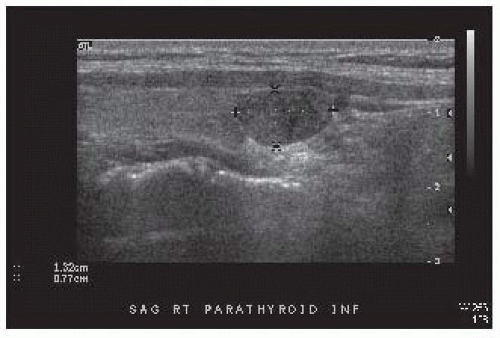
Office-based, high-resolution ultrasonography is the initial imaging study performed. A parathyroid adenoma appears as a homogeneous, hypoechoic, oval- or bean-shaped mass posterior to the thyroid gland (FIG 1). Occasionally, a parathyroid adenoma may be multilobulated. Ultrasound is also of value in identifying concomitant nodular thyroid disease.
Technetium-99m-sestamibi with single-photon emission computed tomography (SPECT) is a combined functional and anatomic imaging study, which is obtained prior to operation. It is particularly beneficial for identifying ectopic parathyroid glands (FIG 2).
Four-dimensional computed tomography and positron emission tomography/computed tomography (PET/CT) fusion imaging are other potentially valuable imaging studies to help localize abnormal parathyroid glands but are usually reserved for patients with persistent or recurrent HPT.
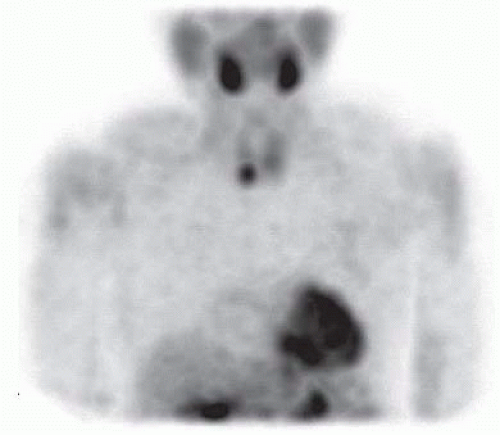
FIG 2 • Technetium-99m-sestamibi image demonstrating abnormal radiotracer accumulation inferior to the inferior pole of the right lobe of the thyroid gland.
Intraoperative PTH monitoring is most valuable in patients with discordant lesions on ultrasound and technetium-99m-sestamibi. It has been suggested that intraoperative PTH monitoring is unnecessary in patients with concordant lesions detected on ultrasound and technetium-99msestamibi imaging.
All patients with primary HPT should be presented with option of surgical therapy, because parathyroidectomy is the only curative treatment. The classical symptoms of primary HPT (nephrolithiasis, osteoporosis, osteitis fibrosa cystica, and neuromuscular dysfunction) are well-established indications for surgery.
In patients with asymptomatic primary HPT, indications for surgical therapy have been defined by the 2008 revised consensus guidelines sponsored by the National Institutes of Health3 (Table 4). Parathyroidectomy is recommended in all patients younger than 50 years of age because at least 25% will develop one or more complications of HPT during their lifetime, which can be irreversible. Significant hypercalcemia, renal dysfunction, reduction in bone mineral density, and inability or unwillingness to participate in subsequent medical surveillance and follow-up are other indications for parathyroidectomy in patients with asymptomatic primary HPT.
Table 4: Indications for Surgical Therapy in Patients with Asymptomatic Primary Hyperparathyroidism as Established by the 2008 Revised National Institutes of Health Consensus Guidelines
Serum calcium >1 mg/dL above the upper limit of the normal range
Glomerular filtration rate <60 mL/min
Decreased bone density: T score of -2.5 or less at lumbar spine, femoral neck, hip, or distal radius
Age <50 years
When routine follow-up and medical surveillance is problematic or not possible
Open neck exploration for primary HPT is performed as an outpatient procedure under general anesthesia or local anesthesia with sedation. Various intraoperative adjuncts may be used including ultrasound, PTH monitoring, and radio guidance.
Intraoperative ultrasound may be used to help determine the best site for the incision.
Intraoperative PTH monitoring may be used to help determine that all hyperfunctioning parathyroid tissue has been excised and to confirm cure of primary HPT.
Administration of technetium-99m-sestamibi prior to operation and use of a gamma probe intraoperatively is used by some surgeons to help localize abnormal parathyroid tissue and confirm ex vivo that a sestamibi-avid parathyroid gland has been removed and that no sestamibi-avid glands remain in the neck. Some of the limitations of this technique include that hyperplastic parathyroid glands are most often not sestamibi-avid, and thyroid nodules may also retain sestamibi, producing false-positive results.
For a single adenoma localized preoperatively, a unilateral focused parathyroidectomy with intraoperative PTH monitoring to confirm cure of primary HPT is performed.
Bilateral neck exploration is indicated for patients with negative preoperative imaging or when bilateral disease is detected preoperatively and for patients with a higher likelihood of multiglandular disease such as patients with MEN I, MEN IIA, or lithium-associated HPT. It may also be necessary for patients with associated thyroid disease. Bilateral neck exploration may also be preferentially used in all patients with primary HPT.
Patients with a double adenoma are treated with resection of the two enlarged glands.
Patients with parathyroid hyperplasia are preferentially treated with subtotal parathyroidectomy, leaving a wellvascularized parathyroid remnant that approximates the weight and size of one normal parathyroid gland. A bilateral transcervical thymectomy is also performed because of a 5% to 15% incidence of supernumerary parathyroid glands, which are most commonly found in the thymus. Alternatively, a total parathyroidectomy and parathyroid autotransplantation into the brachioradialis muscle of the nondominant forearm may be performed (see Part 5, Chapter 42).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree