Oligodendroglioma
Alexandros D. Polydorides, MD, PhD
Key Facts
Clinical Issues
2-5% of all primary brain tumors, 5-25% of gliomas
Most occur in adults, 5-7% arise in infancy/childhood
90% in supratentorial white matter (50-65% frontal)
Long symptomatic period (seizures) before diagnosis
Slow growing, indolent, but often recur locally
Common leptomeningeal or CSF spread
Gross total resection, adjuvant chemoradiation
1p/19q deletion: Favorable response, prognosis
Resected, well-differentiated lesions: Good prognosis
Image Findings
Well circumscribed, heterogeneous, may enhance
Hemorrhagic, cystic, calcified
Macroscopic Features
Soft, gelatinous, gray-pink, calcified (gritty)
Microscopic Pathology
Diffusely infiltrating glioma of cerebral cortex
Monomorphic: Round nuclei, small nucleoli
Clear perinuclear vacuolization (“halo”)
Processing artifact, absent in frozen sections
Arborizing microvascular pattern (“chicken wire”)
Microcalcifications, microcysts, extracellular mucin
Perineuronal satellitosis, subpial aggregates
Circumscribed “clones” within tumor
Focal “minigemistocytes”: Astrocytic appearing
Prominent, eccentric pink cytoplasm
Anaplastic oligodendroglioma (WHO grade III)
Hypercellularity, atypia, nuclear pleomorphism
Increased mitoses, necrosis, vascular proliferation
Mixed glioma (oligoastrocytoma)
Both astrocytoma, oligodendroglioma components
TERMINOLOGY
Synonyms
Malignant = anaplastic oligodendroglioma
Definitions
Diffusely infiltrating glioma, mostly in subcortical white matter of cerebral hemispheres, composed of neoplastic cells resembling oligodendrocytes
WHO grades: II (well differentiated), III (anaplastic)
Chromosome 1p/19q deletion portends better response to chemotherapy and improved prognosis
Mixed glioma (oligoastrocytoma): Phenotypic features of both oligodendroglioma and astrocytoma
ETIOLOGY/PATHOGENESIS
Environmental Exposure
In rats, induced experimentally with nitrosoureas
Human cases reported after prior irradiation
Viral sequences (SV40, JC, BK) identified in some cases
Histogenesis
Morphologic characteristics suggest transformation of oligodendrocytes, but evidence is circumstantial
Originating cell may be immature glial precursor
Dedifferentiation of putative bipotential stem cell
Oligodendrocyte type 2 astrocyte progenitor
May explain occasional immunoreactivity for GFAP
Possible common precursor in oligoastrocytoma
Oligodendrocytes may be related to neurons
Some tumors have neurosecretory-like granules
Some staining for Hu protein, NMDA receptor 1
Ultrastructural findings suggest distinct neoplasm
Genetics
Translocation between chromosomes 1 and 19
Results in 1p/19q codeletion
Incidence varies (40-90%)
Not entirely sensitive or specific
May be present in some astrocytomas
Corresponding gene mutations not yet identified
Several gene candidates exist
As yet, undetected point mutations may also exist
Occasional reports of familial clustering
TP53 mutation generally rare in oligodendrogliomas
LOH seen in < 10-15% of cases
Virtually mutually exclusive with 1p/19q deletions
Mixed glioma histogenesis is unclear
In 1 study both components had 1p/19q deletion
CLINICAL ISSUES
Epidemiology
Incidence
0.2-0.3 per 100, 000 population annually
Approximately 2-5% of all primary brain tumors
5-25% of all intracranial gliomas
Age
Most occur in adults
Peak in 4th-6th decade; mean age: 40-45 years
Infratentorial lesions tend to occur slightly earlier
5-7% arise in infancy/childhood
Gender
Variable, slight male preponderance (3:2 to 2:1)
Site
Throughout neuraxis, mostly in cerebral hemispheres
90% in supratentorial white matter
50-65% involve frontal lobe
Remaining lobes: Temporal > parietal > occipital
50% involve multiple lobes, 20% bilateral
Rare lesions in cerebellum, brainstem
Unusual spinal/leptomeningeal lesions in children
Presentation
Natural History
Most are generally slow growing, indolent
Local recurrence is most common cause of death
Relapse less likely in lesions with 1p/19q deletion
Malignant progression (dedifferentiation) may occur
Less commonly than in astrocytomas
Leptomeningeal or CSF spread is common (1-14%)
Extracranial metastases: Bone, lung, liver
More common than in other gliomas
Especially in higher grade lesions
Oligodendrogliomatosis
Diffuse leptomeningeal spread
May be component of gliomatosis cerebri
Treatment
Surgical approaches
Generally thought unresectable (infiltrating glioma)
But surgery is mainstay of treatment
For diagnosis, reduction of mass effect
Attempt at gross total resection
At least of radiologic abnormality
Adjuvant therapy
In unresected or higher grade lesions
Radiation &/or chemotherapy (PCV, thiotepa)
Favorable response in 1p/19q deleted lesions
Not in largely excised well-differentiated lesions
Unless neoplasm recurs
Prognosis
Well-differentiated lesions carry good prognosis
Survival rates: 5-year (˜ 75%), 10-year (˜ 60%)
After gross total resection
Rates are 1/2 if subtotal resection or higher grade
Better than astrocytomas of comparable grade
Prognosis still guarded: Recurrence after > decade
1p/19q deletion significantly improves prognosis
Median postoperative survival ˜ 10-15 years
(vs. ˜ 2-5 years without codeletion)
Survival advantage also in anaplastic lesions
But may not apply to pediatric lesions
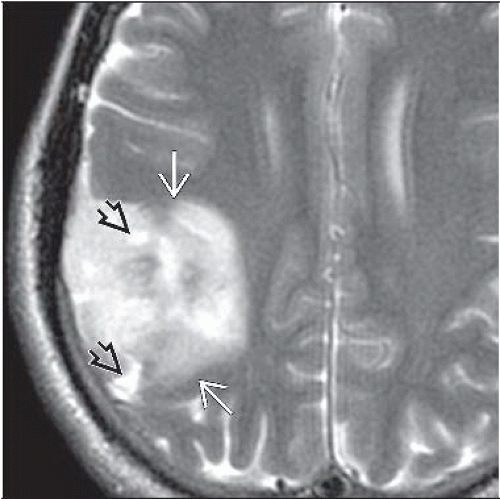
IMAGE FINDINGS
MR Findings
Hypointense on T1WI, hyperintense on T2WI
Variable mass effect, little peritumoral edema
Well-circumscribed margin with brain parenchyma
Heterogeneous: Hemorrhage, cystic degeneration
CT Findings
Superficially seated, usually large intracortical lesion
Rare, deep-seated lesions may cross corpus callosum
Hypo- or isodense, well demarcated
Absent or minimal contrast enhancement
Higher grade (anaplastic) lesions may enhance
But lack rim or ring pattern of glioblastoma
Calcification common (30-90%) but not diagnostic
Usually intracortical and curvilinear, gyriform
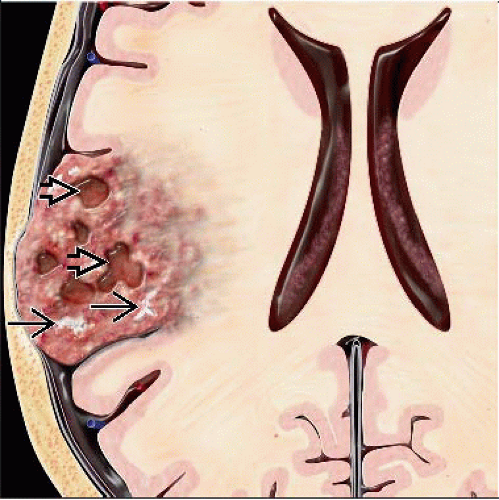
MACROSCOPIC FEATURES
General Features
Soft, gelatinous, gray-pink
May be densely calcified (gritty)
Thickened and expanded cerebral cortex
But relatively well circumscribed overall
Often superficial, may infiltrate leptomeninges
May create marked desmoplastic reaction
Cystic degeneration, intratumoral hemorrhage
Higher grade lesions are more cellular, “fleshy”
But lack central necrosis of glioblastoma
Size
Mean size at presentation: 3.5 cm
MICROSCOPIC PATHOLOGY
Histologic Features
Generally diffusely infiltrating glioma
Obscures normal architecture, gray-white junction
Despite relatively sharp macroscopic interface
Prominent, circumscribed “clones” within tumor
Nodules of ↑ cellularity, atypia, mitotic activity
MIB-1 labeling index is higher
Less common growth patterns
Cohesive ribbons, nests, or clusters of cells
Parallel palisades of tumor cells with long nuclei
Sarcoma-like areas, especially in higher grade lesions
“Secondary structures” often form
Perineuronal satellitosis
Atypical tumor cells orbit large cortical neurons
In larger numbers than normal oligodendroglia
Perivascular collections, rare focal pseudorosettes
Subpial aggregates
Microcalcifications very common (90% of tumors)
Perivascular or stromal laminated calcospherites
In tumor and surrounding cortex
Bone may form in highly calcified lesions
However, not specific for oligodendrogliomas
Characteristic microvascular pattern
Interconnected delicate blood vessels
Geometric branching: Short arcs, angular segments
May arborize, likened to “chicken wire”
Separate out lobules of tumor cells
Glomeruloid microvascular proliferations absent
Extracellular mucin or microcysts are common
Protein-rich, amphophilic, PAS(+) fluid
Peripheral vacuolization
Resembles dysembryoblastic neuroepithelial tumor
Not true cysts (not lined by epithelium)
Cytologic Features
Very monomorphic/monotonous appearance
Uniform cell density, moderate cellularity
Distributed in delicate eosinophilic matrix
Scant rim of cytoplasm
Round nuclei of similar size and shape
Delicate, open, and bland chromatin
Small prominent nucleoli
Artifactual swelling due to fixation/preparation
Clear perinuclear vacuolization (“halo”)
Likened to “fried eggs” or “honeycomb”
Absent in cytology smears and frozen sections
Focally, cells may resemble astrocytes
Faintly gliofibrillar appearance
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree