Occlusive Disease Management: Iliac Angioplasty and Femoral Endarterectomy
Venita Chandra
DEFINITION
Multilevel atherosclerotic occlusive disease involving the distal aorta, iliac vessels, and common femoral arteries is a common occurring pathology seen often by vascular surgeons. Traditional approaches to this disease process involved open surgical reconstruction with an aortobifemoral bypass or iliofemoral bypass. Recently, however, there has been a paradigm shift toward endovascular and hybrid approaches. Combining femoral endarterectomy with endovascular iliac stenting is an increasingly common minimally invasive approach to this problem, providing an effective alternative to open strategies with the potential of shorter hospitalizations and decreased morbidity. Compared to iliac stenting alone, proper evaluation of femoral disease and, if indicated, a hybrid approach with concomitant femoral endarterectomy have been associated with increased durability of endovascular aortoiliac interventions.1
PATIENT HISTORY AND PHYSICAL FINDINGS
Aortoiliac and femoral occlusive disease can present, as with all peripheral arterial diseases (PADs), in a variety of ways.
The typical presentation of aortoiliac occlusive disease includes claudication of the buttock and upper thigh and erectile dysfunction. When multilevel vascular disease occurs, as in the case of combined aortoiliac and femoral occlusive disease, distal lower extremity symptoms such as calf claudication, rest pain, and tissue loss may ensue.
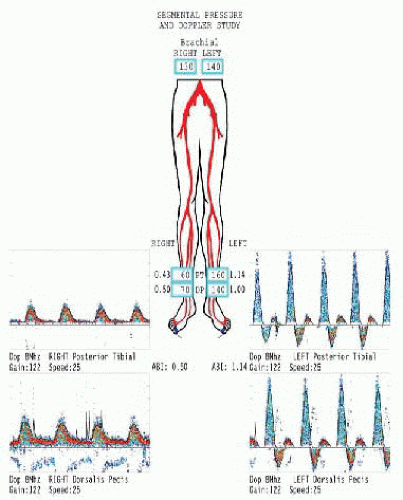
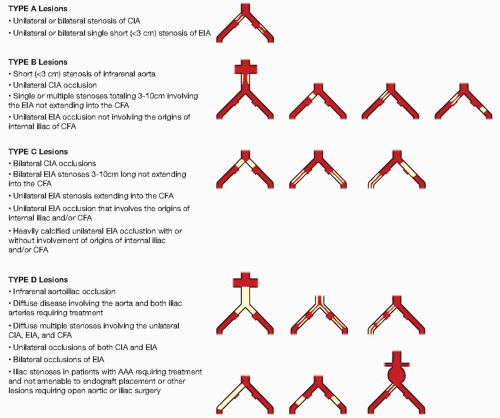
FIG 1 • Arterial waveforms and ABIs for a patient with aortoiliac disease. Note the monophasic waveforms on the right.
Typical physical exam includes the absence or diminution of femoral pulses. Other than the peripheral pulse assessment, the physical exam can demonstrate other signs of PAD such as cool digits and active wounds.
IMAGING AND OTHER DIAGNOSTIC STUDIES
The initial evaluation of a patient with PAD should involve noninvasive evaluation of peripheral blood flow with arterial waveforms and ankle-brachial indices (ABIs) (FIG 1). These studies provide objective data regarding the extent of occlusive disease; however, they do not provide adequate anatomic data for preoperative planning.
Once the degree and physiologic impact of the disease are determined by noninvasive testing, high-resolution anatomic imaging via either computed tomographic angiography (CTA) or magnetic resonance angiography (MRA) should be obtained for surgical planning.
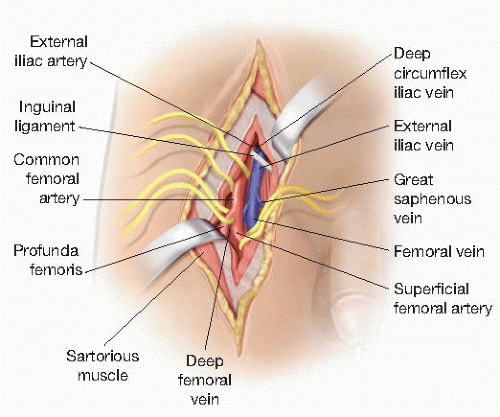
CTAs are currently the gold standard for preoperative planning. They have the advantage of providing information regarding the degree and location of stenosis as well as the anatomy of the arterial wall (including degree of calcification and presence of aneurysms). Three-dimensional reformatting can provide additional valuable information (FIG 2). CTAs, however, are limited by the fact that they involve the use of contrast as well as radiation exposure. MRAs avoid radiation exposure and contrast often, however, at the risk of reduced anatomic precision. Gadolinium magnetic resonance (MR) contrast also entails risk of long-term renal dysfunction.
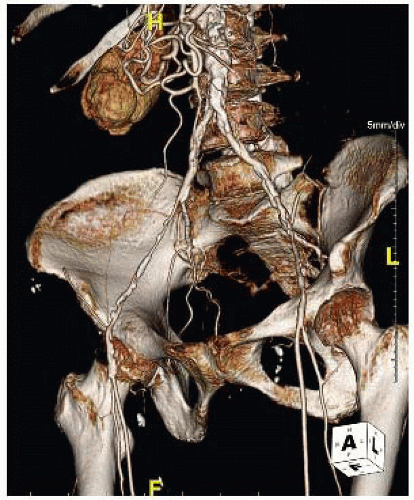
FIG 2 • CTA with 3-D reconstruction demonstrating diffuse aortoiliac as well as femoral occlusive disease.
Catheter-based diagnostic aortography also provides anatomic data; however, this study has a number of limitations including the fact that it is an invasive procedure with potential complications. In addition, arteriograms only provide an understanding of the luminal anatomy, occasionally obscuring features such as aneurysms, inclusion cysts, or periarterial inflammation. Particularly for aorto-iliac-femoral disease, preprocedural CTA has the ability to identify significant common femoral disease that may benefit from concomitant open endarterectomy at the time of catheter-based intervention. Alternatively, relying on catheter-based arteriography as the primary diagnostic modality may reduce overall contrast burden, radiation exposure, and need for additional procedures if common femoral level intervention is not required. In general, careful preprocedural physical examination and duplex imaging may suffice to help determine whether the additional cost, risk, and inconvenience of CTA are justified prior to catheter-based intervention for aortoiliac arterial occlusive disease.
SURGICAL MANAGEMENT
As with all patients with PAD, initial treatment approach should include comprehensive assessment and management of concomitant cardiovascular disease risk factors. Details regarding maximal medical management of PAD are beyond the scope or purpose of this chapter; at a minimum, however, consideration should be given to beginning statin and antiplatelet therapy prior to intervention, along with consideration of beta blockade and angiotensin receptor blocker or converting enzyme inhibitor therapy in selected patients.
Regardless of medical or anesthetic risk, however, all patients with critical limb ischemia should be considered candidates for revascularization when limb loss is a distinct possibility. Despite platitudes to the contrary, major limb amputation above or below the knee is not necessarily a “safer” surgical alternative to multilevel hybrid revascularization. Indications for intervention for intermittent claudication are somewhat more complicated, however. The risks of a procedure are weighed against the potential gain; typically, only patients with severe lifestyle-limiting claudication who have failed nonoperative strategies are offered surgical revascularization.
Preoperative Planning
Determining the anatomic distribution of disease is essential to obtaining optimal results. The imperative for precision imaging cannot be emphasized enough—if you cannot appreciate the full extent of disease, you cannot expect to comprehensively address it. As in all aspects of vascular surgery, the biggest disappointments, both during and after the procedure, usually arise from underestimating the extent of underlying disease.
The Trans-Atlantic Inter-Society Consensus (TASC) II guidelines provide a classification scheme based on anatomic patterns of disease (FIG 3).2 The recommendations of the TASC II guidelines is an endovascular management for TASC A and B iliac lesions, whereas open surgical reconstruction is recommended for TASC C and D lesions in good-risk patients. Frequently, however, patients with multilevel disease as seen in TASC C and D lesions have more virulent atherosclerotic processes that often make them poorer surgical candidates. In addition, the development of an increasingly sophisticated armamentarium of endovascular tools and strategies are leading more and more vascular surgeons to attempt endovascular revascularization, even for patients with TASC C or D lesions. Further updates of the TASC classification guidelines are under review and will likely be published in the near future, highlighting the dynamic nature of surgical management of this challenging condition.
Targeted perioperative risk assessment should be undertaken in appropriate patients, particularly those with reduced exercise tolerance, known or suspected congestive heart failure, clinically significant pulmonary disease, exerciseinduced angina, arrhythmias, or those with recent history of myocardial infarction. The presence of additional relevant comorbidities, including diabetes, reduced glomerular filtration rate, iodinated contrast allergies, thrombophilia or coagulopathic disorders, concomitant bacterial infection, or liver disease should also be identified and, when present, evaluated.
Positioning
Patients are generally placed in the supine position, either in a hybrid operating suite with fixed imaging capabilities or on a radiolucent table with a mobile imaging unit (C-arm) in a traditional operating room environment.
Positioning should be arranged in such as way as to ensure adequate exposure of the entire aortoiliac and femoral vasculature, with room on either side of the patient to rotate the imaging unit to various angles in order to obtain appropriate oblique images. In angiographic parlance, in many important circumstances (such as identifying and protecting the origin of the ipsilateral internal iliac artery), “one view is no view.”
TECHNIQUES
FEMORAL ENDARTERECTOMY
First Step
For extended femoral endarterectomy (often requiring exposure of the proximal deep femoral artery as well as the entire length of common femoral artery), optimal exposure is obtained via a longitudinal incision placed directly over the femoral artery (FIG 4). The inguinal ligament should be identified by palpation of the pubic tubercle and anterior superior iliac spine (an oblique line between these two structures is the typical course of the inguinal ligament) and used as a guide for femoral localization. Typically, the femoral artery is located approximately one-third the distance from the pubic tubercle to anterior superior iliac crest. Even when no pulse is palpable, a firm calcified linear mass can usually be palpated in this area. Alternatively, duplex ultrasound or fluoroscopic imaging may be used to ensure accurate placement of the incision. Failure to incise directly over the common femoral artery may increase risk for chronic lymphatic drainage, delayed or complicated wound healing, and femoral nerve or venous injury. Although oblique femoral incisions have gained in popularity, especially when used to obtain femoral access for proximal aneurysm repair, these often do not provide exposure sufficient for comprehensive endarterectomy as previously detailed.
The subcutaneous tissues are divided, ligating any lymphatic channels that are encountered. The inferior edge of the inguinal ligament is identified and the common femoral artery is exposed through the femoral sheath as it exits underneath the inguinal ligament.
Second Step
Full circumferential dissection of the distal external iliac artery (under the inguinal ligament), the common femoral artery, the superficial femoral artery, and the origin of the deep femoral artery and its initial branches are obtained sequentially (FIG 4).
The individual arteries should be assessed for areas of calcification and extensive plaque burden. Soft sections with minimal calcification, or plaque limited to the posterior arterial wall, should be identified for consideration of clamp placement as appropriate for the planned procedure.
The inguinal ligament may be divided for adequate exposure of the distal external iliac artery when necessary to ensure adequate endarterectomy When considering the relative margin of distal endarterectomy versus proximal stent placement, it is important to avoid stent placement across the inguinal ligament, as this may greatly reduce long-term patency of the procedure as well as complicate stent delivery through an ipsilateral retrograde sheath. In general, operators should err of the side of more extensive proximal endarterectomies as opposed to distal extension of external iliac stents.
Careful ligation of the circumflex iliac vein as it crosses over the external iliac artery under the inguinal ligament should be considered to prevent accidental tearing of the vessel during clamping.
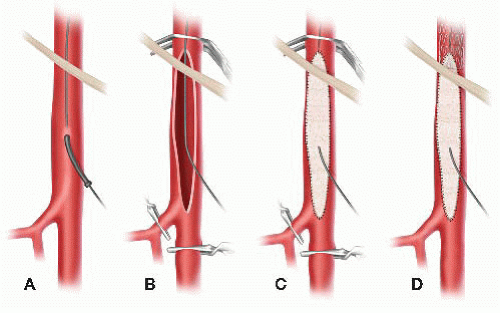
FIG 5 • Technique for concurrent femoral endarterectomy and iliac stenting. A. Direct puncture of common femoral artery and advancement of wire under fluoroscopic guidance. B. With wire across iliac lesion, clamp proximal and distal and proceed with arteriotomy. C. After endarterectomy, patch is sewn in. Prior to completion of patch center, the distal portion of the patch is punctured with an 18-gauge needle and the wire is passed through the patch. D. After completion of the patch, flow is restored and a sheath can be advanced over the wire and iliac stenting can proceed. For patients with distal external iliac disease, the iliac stents can be carried down into the proximal portion of the endarterectomy and patch.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access