TABLE 9.1 Potential Side Effects in the Administration of Radiopharmaceuticals | ||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||
Alert the patient that he or she may be required to follow a study-specific preparation regimen before imaging determined by the type of nuclear medicine procedure (e.g., nothing by mouth [Latin: nil per os, NPO], no caffeine for 24 hours, hydration, bowel preparation).
Administer a radiopharmaceutical through one of several routes: oral, inhalation, intravenous, intramuscular, intrathecal, or intraperitoneal. On occasion, additional pharmaceuticals may be administered to enhance the function of the organ of interest.
A time delay may be necessary for the radiopharmaceutical to reach the organ of interest.
Imaging time depends on:
Specific study radiopharmaceutical used and the time that must be allowed for concentration in tissues
Type of imaging equipment used
Patient cooperation
Additional views based on patient history and nuclear medicine protocol
Patient’s physical size
 PROCEDURAL ALERT
PROCEDURAL ALERT
Benefits
Nuclear medicine yields functional data that are not provided by other modalities.
Nuclear imaging is relatively safe, painless (except for intravenous administration), and noninvasive.
Risks
Radiation exposure is minimal; toxicity is nil.
Hematoma at intravenous injection site.
Reactions to the radiopharmaceutical (hives, rash, itching, constriction of throat, dyspnea, bronchospasm, anaphylaxis [rare]).
Pregnancy (confirmed or suspected). Pregnancy is a contraindication for most nuclear imaging.
Lactating women may be advised to stop nursing for a set period (e.g., 2 to 3 days with 99mTc). Most radiopharmaceuticals are excreted in the mother’s milk.
Radiopharmaceutical uptake from a recent nuclear medicine examination could interfere with interpretation of the current study.
The presence of any prostheses in the body must be recorded on the patient’s history because certain devices can shield the gamma rays from imaging.
Current medications, treatments, and diagnostic measures (e.g., telemetry, oxygen, urine collection, intravenous lines)
Age and current weight. This information is used to calculate the radiopharmaceutical dose to be administered. If the patient is younger than 18 years of age, notify the examining department before testing. The amount of radioactive substance administered is adjusted downward for anyone younger than 18 years of age.
Allergies. Past history of allergies, especially to contrast substances (e.g., iodine) used in diagnostic procedures.
Explain the purpose, procedure, benefits, and risks of the nuclear medicine procedure.
Assess for allergies to substances such as iodine.
Reassure the patient that the procedure is safe and painless.
Inform the patient that the procedure is performed in the nuclear medicine department. Contact the department to determine the expected time and length of the procedure.
Have the patient appropriately dressed.
Obtain an accurate weight because the radiopharmaceutical dose may be calculated by weight.
If a female patient is premenopausal, determine whether she may be pregnant. Pregnancy is a contraindication to most nuclear imaging.
Irradiation of the fetus should be avoided whenever possible.
Nuclear medicine procedures are usually contraindicated in pregnant women. Lactating women may need to discard their breast milk for several days following the procedure.
These precautions are also to be followed for the radionuclide laboratory procedures and PET imaging.
Use routine disposal procedures for body fluids and excretions unless directed otherwise by the nuclear medicine department. Special considerations for disposal must be followed for therapeutic procedures.
Record any problems that may have occurred during the procedure.
Monitor the injection site for signs of bruising, hematoma, infection, discomfort, or irritation.
Assess for side effects of radiopharmaceuticals.
Be aware that depending on hospital policy, a valid consent form may be requested to be signed by the parents or legal guardians of the patient.
Explain the procedure and its purpose, benefits, and risks to the parents or legal guardians and to the patient. Reassure the patient that the test is safe and painless.
Assess for allergy to medications.
Have the patient appropriately dressed, ensuring that there are no metal objects on the patient during the procedure.
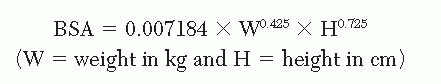
Obtain an accurate weight; the dose is calculated based on the patient’s weight. Because pediatric patients have a different body metabolism than adults, a lower dose is given. Use of a “body surface area” (BSA) formula is recommended. The most commonly used is the DuBois formula:
Remember that immobilization techniques are often used during the imaging of pediatric patients. Wrapping an infant or small child is often necessary. Head clamps, arm boards, or sandbags may be used for patient immobilization.
Administer sedative drugs to reduce patient motion during the examination. Disadvantages of sedation may include nausea and vomiting.
Start an intravenous line for administration of radiopharmaceuticals.
Do not leave patients unattended during the procedure.
Pediatric patients need constant reassurance and emotional support.
Patient urination is often difficult to control. A urinary catheter may be required.
Verify that the adolescent female patient is not pregnant.
Same as those stated for adults
Observe pediatric patients for adverse reactions to radiopharmaceuticals. Infants are more at risk for reactions.
Myocardial perfusion general imaging
There are two phases to this procedure: the rest imaging and the stress imaging. Either 201Tl, 99mTc sestamibi, or 99mTc tetrofosmin may be used.
Rest imaging
Perform an intravenous injection of the radioisotope. Allow a 30- to 60-minute delay for the radioisotope to localize in the heart.
Perform SPECT imaging.
Stress imaging
The patient undergoes an exercise or a pharmacologic cardiac stress test. At the peak level of stress, inject the patient with the radioisotope.
SPECT imaging may begin 30 minutes after injection.
Pharmacologic stress tests may be performed with any of three routine stressing agents:
Infuse dipyridamole over 4 to 6 minutes. Inject the radiopharmaceutical. Two minutes later, administer aminophylline, an antidote to the dipyridamole, at the nuclear medicine physician or cardiologist’s discretion. Patient monitoring may last 20 minutes. Contraindication: caffeine.
Infuse regadenoson over 20 seconds. Inject the radiopharmaceutical 3 minutes after the infusion.
Infuse dobutamine until the predicted heart rate is achieved. The infusion protocol lasts 3 minutes at each dose increment.
201Tl
During the cardiac stress test, the patient is monitored by a nuclear medicine physician, cardiologist, a registered nurse, an electrophysiologist, or an ECG technician.
Have the patient begin walking on the treadmill.
When the monitoring person determines that the patient has reached 85% to 95% of maximum heart rate, inject radioactive thallium. Take the patient for immediate imaging.
SPECT imaging begins within 5 minutes of injection.
Acquire a second image approximately 3 to 4 hours later, with the patient at rest, to determine redistribution of the thallium.
See Chapter 1 guidelines for safe, effective, informed intratest care.
99mTc sestamibi and 99mTc tetrofosmin
Follow myocardial perfusion general imaging procedures.
Observe standard precautions.
 PROCEDURAL ALERT
PROCEDURAL ALERT PROCEDURAL ALERT
PROCEDURAL ALERT
Imaging that is abnormal during exercise but remains normal at rest indicates transient ischemia.
Nuclear cardiac imaging that is abnormal both at rest and under stress indicates a past infarction.
Hypertrophy produces an increase in uptake.
The progress of disease can be estimated.
The location and extent of myocardial disease can be assessed.
6. Specific and significant abnormalities in the stress ECG usually are indications for cardiac catheterization or further studies.
Inadequate cardiac stress
Caffeine intake
Injection of dipyridamole in the upright or standing position or with isometric handgrip may increase myocardial uptake.
Explain test purpose and procedure, benefits, and risks. See standard nuclear medicine imaging pretest precautions.
Before the stress test has begun, start an intravenous line and prepare the patient. Perform a resting 12-lead ECG and blood pressure measurement.
Advise the patient that the exercise stress period will be continued for 1 to 2 minutes after injection to allow the radiopharmaceutical to be cleared during a period of maximum blood flow.
The patient should experience no discomfort during the imaging.
Alert the patient that fasting may be recommended for at least 2 hours before the stress test. Caffeine intake must be eliminated for 24 hours before the stress test.
For dipyridamole administration:
Fasting may be required before the stress test, and avoidance of any caffeine products for at least 24 hours before the test is necessary.
Blood pressure, heart rate, and ECG results are monitored for any changes during the infusion. Aminophylline may be given to reverse the effects of the dipyridamole.
See Chapter 1 guidelines for safe, effective, informed pretest care.
The stress study is contraindicated in patients who:
Have a combination of right and left bundle branch block
Have left ventricular hypertrophy
Are taking digitalis or quinidine
Are hypokalemic (because the results are difficult to evaluate)
Adverse short-term effects of dipyridamole may include nausea, headache, dizziness, facial flush, angina, ST-segment depression, and ventricular arrhythmia.
Observe the patient for possible effects of dipyridamole infusion.
Interpret test outcomes, counsel, and monitor appropriately.
Refer to nuclear scan posttest precautions.
Follow Chapter 1 guidelines for safe, effective, informed posttest care.
is associated with an area of increased radioactivity (hot spot) on the myocardial image. This test is useful when ECG and enzyme studies are not definitive.
Myocardial imaging involves a 4-hour delay before imaging after the intravenous injection of the radionuclide. During this waiting period, the radioactive material accumulates in the damaged heart muscle.
Alert the patient that imaging takes 30 to 45 minutes, during which time the patient must lie still on an imaging table.
See Chapter 1 guidelines for safe, effective, informed intratest care.
Imaging that is entirely normal indicates that an acute infarction is not present and the myocardium is viable.
Myocardial uptake of the PYP is compared with the ribs (2+) and sternum (4+). Higher uptake levels (4+) reflect greater myocardial damage.
Larger defects have a poorer prognosis than small defects.
Imaging can be performed at the bedside in the acute phase of infarction if the nuclear medicine department has a mobile gamma camera.
Explain the purpose, procedure, benefits, and risks of the nuclear medicine study. See standard pretest precautions.
Remember that imaging must occur within a period of 12 hours to 7 days after the onset of symptoms of infarction. Otherwise, false-negative results may be reported.
See Chapter 1 for additional guidelines for safe, effective, informed pretest care.
Interpret the outcome and monitor appropriately. If heart surgery is needed, counsel the patient concerning follow-up testing after surgery.
Refer to standard precautions and posttest care.
Follow additional guidelines in Chapter 1 for safe, effective, informed posttest care.
information about cardiac output, end-systolic volume, end-diastolic volume, ejection fraction, ejection velocity, and regional wall motion of the ventricles. Computer-aided imaging of wall motion of the ventricles can be portrayed in the cinematic mode to visualize contraction and relaxation. This procedure may also be performed as a stress test. MUGA images are not often performed on children.
This procedure may be performed with or without stress. A MUGA with the patient at rest could be performed at the bedside if necessary, if the nuclear medicine department has a mobile camera.
Label the patient’s own RBCs with 99mTc-PYP by any of several methods. Inject the blood once it is labeled. In children and adults, administer the 99mTc-labeled RBCs slowly through an intravenous line. For children younger than 3 years of age, sedation may be required for the injection and to allow the pediatric patient to hold still for the required 20 to 30 minutes. Alternatively, perform a cardiac flow study.
During an ECG, the patient’s R wave signals the computer and camera to take several image frames for each cardiac cycle.
Image the patient immediately after injection of the labeled RBCs.
See Chapter 1 guidelines for safe, effective, informed intratest care.
Congestive cardiac failure
Change in ventricular function due to infarction
Persistent arrhythmias from poor ventricular function
Regurgitation due to valvular disease
Ventricular aneurysm formation
Explain the purpose, procedure, benefits, and risks.
Follow standard nuclear medicine imaging pretest precautions.
See Chapter 1 for additional guidelines for safe, effective, informed pretest care.
Interpret MUGA outcomes and monitor appropriately for cardiac disease.
Refer to standard nuclear scan posttest precautions.
Follow basic Chapter 1 guidelines for safe, effective, informed posttest care.
pass” through the cardiac chambers in multiple rapid images. The first-pass study uses a jugular or antecubital vein injection of the radiopharmaceutical. A large-bore needle is used.
Use a three-way stopcock with saline flush for radionuclide injection into the jugular vein or the antecubital fossa. For a shunt evaluation, inject the radionuclide into the external jugular vein to ensure a compact bolus.
Have the patient lie supine with the head slightly raised.
Although the total patient time is approximately 20 to 30 minutes; the actual imaging time is only 5 minutes.
Perform resting MUGA imaging with a shunt study.
See Chapter 1 guidelines for safe, effective, informed intratest care.
Abnormal first-pass ejection fraction values are associated with:
Congestive heart failure
Change in ventricular function due to infarction
Persistent arrhythmias from poor ventricular function
Regurgitation due to valvular disease
Ventricular aneurysm formation
Abnormal heart shunts reveal:
Left-to-right shunt
Right-to-left shunt
Mean pulmonary transit time
Tetralogy of Fallot (seen most often in children)
Explain the purpose, procedure, benefits, and risks. An intravenous line is required.
See Chapter 1 for additional guidelines for safe, effective, informed pretest care.
Refer to standard nuclear scan pretest precautions.
Obtain a signed, witnessed consent form if stress testing is to be done.
Interpret test outcomes, monitor injection site, and counsel appropriately.
Refer to standard nuclear scan posttest precautions.
Follow basic Chapter 1 guidelines for safe, effective, informed posttest care.
Have the patient swallow radioactive iodine in a capsule or liquid form.
Determine an uptake 4 to 6 hours and 24 hours after dosing. Four hours after dosing, the thyroid (neck area) is imaged if you are using 123I for both the uptake and the image.
Normal scan time is about 45 minutes.
See Chapter 1 guidelines for safe, effective, informed intratest care.
Cancer of the thyroid most often manifests as a nonfunctioning cold nodule, indicated by a focal area of decreased uptake.
Some abnormal results are:
Hyperthyroidism, represented by an area of diffuse increased uptake
Hypothyroidism, represented by an area of diffuse decreased uptake
Graves’ disease, represented by an area of diffuse increased uptake
Autonomous nodules, represented by focal area of increased uptake
Hashimoto’s disease (chronic lymphocytic thyroiditis, an autoimmune disease), represented by mottled areas of decreased uptake
Imaging alone cannot definitively determine the diagnosis; uptake information is essential for a definitive diagnosis.
Thyroid imaging needs to be completed before radiographic examinations using contrast media (e.g., intravenous pyelogram, cardiac catheterization, CT with contrast, myelogram) are performed.
Any medication containing iodine should not be given until the nuclear medicine thyroid procedures are concluded. Notify the attending physician if thyroid studies have been ordered or if there are interfering radiographs or medications.
Instruct the patient about nuclear medicine imaging purpose, procedure, and special restrictions. Refer to standard nuclear medicine imaging pretest precautions.
Because the thyroid gland responds to small amounts of iodine, the patient may be requested to refrain from iodine intake for at least 1 week before the test. Patients should consult with a physician. Restricted items include the following:
Certain thyroid drugs
Weight-control medicines
Multiple vitamins
Some oral contraceptives
X-ray contrast materials containing iodine
Cough medicine
Iodine-containing foods, especially kelp and other “natural” foods
Alleviate any fears the patient may have about radionuclide procedures.
See Chapter 1 guidelines for safe, effective, informed pretest care.
Nuclear medicine thyroid imaging is contraindicated in pregnancy. Thyroid testing in pregnancy is routinely limited to blood testing.
This study should be completed before thyroid-blocking radiographic contrast agents are administered and before thyroid or iodine drugs are given.
Occasionally, tests are performed purposely with iodine or some thyroid drug in the body. In these cases, the physician is testing the response of the thyroid to these drugs. These stimulation and suppression tests are usually done to determine the nature of a particular nodule and whether the tissue is functioning or nonfunctioning.
If iodine has been administered, observe the patient for signs and symptoms of allergic reaction as needed.
Explain test outcomes and possible treatment.
Refer to standard nuclear medicine imaging posttest precautions.
Interpret test outcomes and counsel appropriately.
Follow Chapter 1 guidelines for safe, effective, informed, posttest care.
This procedure measures the rate of accumulation, incorporation, and release of iodine by the thyroid. The rate of absorption of the radioactive iodine, which is determined by the increase in radioactivity of the thyroid gland, is a measure of the ability of the thyroid to concentrate iodine from blood plasma. The radioactive isotopes of iodine used are 131I and 123I.
A fasting state is preferred. A complete history and listing of all medications is a must for this test. This history should include nonprescription as well as herbal medications and patient dietary habits.
Administer a liquid form or a tasteless capsule of radioactive iodine orally.
Measure the amount of radioactivity by an uptake calculation of the thyroid gland 4 to 6 and 24 hours later. There is no pain or discomfort involved.
Have the patient return to the laboratory at the designated time because the exact time of measurement is crucial in determining the uptake.
Increased uptake (e.g., 20% in 1 hour, 25% in 6 hours, 45% in 24 hours) suggests hyperthyroidism but is not diagnostic for it.
Decreased uptake (e.g., 0% in 2 hours, 3% in 6 hours, 10% in 24 hours) may be caused by hypothyroidism but is not diagnostic for it.
If the administered iodine is not absorbed, as in severe diarrhea or intestinal malabsorption syndromes, the uptake may be low even though the gland is functioning normally.
Rapid diuresis during the test period may deplete the supply of iodine, causing an apparently low percentage of iodine uptake.
In renal failure, the uptake may be high even though the gland is functioning normally.
This test is contraindicated in pregnant or lactating women, in children, in infants, and in persons with iodine allergies.
Whenever possible, this test should be performed before any other radionuclide procedures are done, before any iodine medications are given, and before any radiographs using iodine contrast media are taken.
The chemicals, drugs, and foods that interfere with the test by lowering the uptake are:
Iodized food and iodine-containing drugs such as Lugol solution, expectorants, cough medications, saturated solutions of potassium iodide, and vitamin preparations that contain minerals. The duration of the effects of these substances in the body is 1 to 3 weeks.
Radiographic contrast media such as iodopyracet (Diodrast), sodium diatrizoate (Hypaque, Renografin), poppy-seed oil (Lipiodol), ethiodized oil (Ethiodol), iophendylate (Pantopaque), and iopanoic acid (Telepaque). The duration of the effects of these substances is 1 week to 1 year or more; consult with the nuclear medicine laboratory for specific times.
Antithyroid drugs such as propylthiouracil (PTU) and related compounds. The duration of the effects of these drugs may last 2 to 10 days.
Thyroid medications such as liothyronine sodium (Cytomel), desiccated thyroid, thyroxine (Synthroid, levothyroxine sodium) (duration, 1 to 2 weeks)
Miscellaneous drugs such as thiocyanate, perchlorate, nitrates, sulfonamides, tolbutamide (Orinase), corticosteroids, para-aminosalicylate, isoniazid, phenylbutazone (Butazolidin), thiopental (Pentothal), antihistamines, adrenocorticotropic hormone, aminosalicylic acid, cobalt, and warfarin sodium (Coumadin) anticoagulants. Consult with the nuclear medicine department for duration of effects of these drugs as they vary widely.
The compounds and conditions that interfere by enhancing the uptake are:
Thyroid-stimulating hormone (thyrotropin)
Pregnancy
Cirrhosis
Barbiturates
Lithium carbonate
Phenothiazines (duration, 1 week)
Iodine-deficient diet
Renal failure
Explain test purpose and procedure; the test takes 24 hours to complete. Assess and record pertinent dietary and medication history.
Advise that iodine intake is restricted for at least 1 week before testing.
Refer to standard nuclear medicine imaging pretest precautions.
See Chapter 1 guidelines for safe, effective, informed pretest care.
Explain test outcomes and possible treatment.
Refer to standard nuclear medicine imaging posttest precautions.
Interpret test outcomes and counsel appropriately.
Follow Chapter 1 guidelines for safe, effective, informed, posttest care.
adrenal medullas. Adrenergic tumors have been called paragangliomas when they are found outside the adrenal medulla, but many practitioners refer to all neoplasms that secrete norepinephrine and epinephrine as pheochromocytomas. Because the only definite and effective therapy is surgery to remove the tumor, identification of the site using adrenal gland imaging, CT, and ultrasound is an essential goal of treatment.
Inject intravenously the radionuclide 131I or 123I metaiodobenzylguanidine (MIBG).
Take images at the physician’s discretion, usually 4 and 24 hours after injection.
Advise the patient that imaging may take 2 hours.
See Chapter 1 guidelines for safe, effective, informed intratest care.
Abnormal results give substance to the “rough rule of 10” for these tumors:
Ten percent are in children.
Ten percent are familial.
Ten percent are bilateral in the adrenal glands.
Ten percent are malignant.
Ten percent are multiple, in addition to bilateral.
Ten percent are extrarenal.
More than 90% of primary pheochromocytomas occur in the abdomen.
Pheochromocytomas in children often represent a familial disorder.
Bilateral adrenal tumors often indicate a familial disease, and vice versa.
Multiple extrarenal pheochromocytomas are often malignant.
The presence of two or more pheochromocytomas strongly indicates malignant disease.
Explain nuclear medicine imaging purpose, procedure, benefits, and risks.
Give Lugol’s solution (potassium iodine) 1 day prior to the injection, the day of the injection, and 4 days postinjection to prevent uptake of radioactive iodine by the thyroid gland (usually 4 drops of Lugol’s in orange juice).
Refer to standard nuclear medicine imaging pretest precautions.
See Chapter 1 guidelines for safe, effective, informed pretest care.
Interpret test outcome and counsel appropriately about the need for possible follow-up tests. Follow-up tests include:
Kidney and bone imaging to give further orientation to abnormalities discovered by MIBG scan.
CT procedure if MIBG imaging failed to locate the tumor.
Ultrasound of the pelvis if the tumor produces urinary symptoms.
Refer to standard nuclear medicine imaging posttest precautions.
Follow Chapter 1 guidelines for safe, effective, informed posttest care.
Administer 123I. Four hours later, image the neck.
Inject 99mTc sestamibi without moving the patient; after 10 minutes, acquire additional images. Computer processing involves subtracting the technetium-visualized thyroid structures from the 123I accumulation in a parathyroid adenoma.
Alert patient that total examination time is 1 hour.
See Chapter 1 guidelines for safe, effective, informed intratest care.
Explain the purpose, procedure, benefits, and risks of parathyroid imaging.
Assess for the recent intake of iodine. However, this finding is not a specific contraindication to performing the study.
Palpate the thyroid carefully.
Refer to standard nuclear scan pretest precautions.
See Chapter 1 guidelines for safe, effective, informed pretest care.
Refer to standard nuclear medicine imaging posttest precautions.
Interpret test outcome and monitor appropriately.
Follow Chapter 1 guidelines for safe, effective, informed posttest care.
To detect the presence or absence of unilateral kidney disease
For long-term follow-up of hydroureteronephrosis
To study the hypertensive patient to evaluate for renal artery stenosis. The captopril test is a firstline study to determine a renal basis for hypertension.
To study the azotemic (increase in urea in the blood) patient when urethral catheterization is contraindicated or impossible
To evaluate upper urinary tract obstruction
To assess renal transplant efficacy
Place the patient in either an upright sitting or supine position for imaging; the supine position is preferred for pediatric patients.
Inject the radiopharmaceutical intravenously. An intravenous diuretic (furosemide [Lasix]) or angiotensin-converting enzyme (ACE) inhibitor (enalapril/captopril) may also be administered during a second phase of the renogram.
Start imaging immediately after injection.
Alert patient that total examination time is approximately 45 minutes for a routine, one-phase renogram.
See Chapter 1 guidelines for safe, effective, informed intratest care.
 PROCEDURAL ALERT
PROCEDURAL ALERT
The test should be performed before an intravenous pyelogram.
A renogram may be performed in a pregnant woman if it is imperative to assess renal function.
Hypertension
Obstruction due to stones or tumors
Renal failure
Decreased renal function
Diminished blood supply
Renal transplant rejection
In pediatric patients, urinary tract infections in male neonates; the finding shifts to females after 3 months of age.
Explain the purpose, procedure, benefits, and risks of the procedure. Pediatric patients have a detectible glomerular filtration rate after 6 months of age. In the neonate, ultrasound is used in combination with nuclear medicine procedures for a more complete renal assessment. Refer to standard nuclear medicine imaging pretest precautions. An intravenous line is placed before imaging. Check for history of previous transplantation.
Unless contraindicated, ensure that the patient is well hydrated with two to three glasses of water (10 mL per kilogram of body weight) before undergoing the test.
See Chapter 1 guidelines for safe, effective, informed pretest care.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


