Nipple-Areolar Reconstruction
Anita R. Kulkarni
Amy K. Alderman
Andrea L. Pusic
DEFINITION
Nipple-areolar reconstruction (NAR) is typically performed as the final stage of breast reconstruction after mastectomy. The nipple is reconstructed to give three-dimensional projection, and the areola is reconstructed separately to mimic a natural nipple-areolar complex (NAC).
PATIENT HISTORY AND PHYSICAL FINDINGS
NAR is an elective stage of breast reconstruction that can be performed after any type of primary breast mound reconstruction. Published studies indicate that approximately 50% of breast reconstruction patients elect to undergo NAR.1,2
NAR is performed at least 3 months after breast reconstruction is complete. This allows the final breast shape and position to be obtained prior to placement of the NAC.
NAR can also be performed in a delayed fashion at any time a patient decides, including months or years after breast mound reconstruction.
SURGICAL MANAGEMENT
There are many described techniques for nipple reconstruction, including nipple sharing, local flaps, cartilage grafts, dermal grafts, and prostheses.3 Local flaps are the most popular option and are described in detail in this chapter.
Reconstructed nipples lack the rigid ductal and smooth muscle elements of a natural nipple; therefore, the long-term maintenance of nipple projection continues to be the most challenging aspect of NAR.4
Multiple autologous and prosthetic materials (auricular cartilage, rib cartilage, toe pulp, acellular dermal matrix, calcium hydroxylapatite, polytetrafluoroethylene implants, etc.) have been attempted to give permanent rigidity to the nipple; however, no single technique has demonstrated definitive superiority.3
Areolar reconstruction is primarily done by skin grafting, tattoo, or both.
The first described technique in this chapter is a skate flap for nipple reconstruction with a full-thickness skin graft for areolar reconstruction. This procedure is typically done in the operating room under sedation or general anesthesia.
The second described technique is a C-V flap for nipple reconstruction, which can be used in combination with a tattoo for areolar reconstruction. This procedure can be done in the office under local anesthesia.
Preoperative Planning
In unilateral NAR, the position, size, and shape of the opposite nipple are taken into consideration to design the reconstruction in addition to anatomic landmarks. In bilateral NAR, anatomic landmarks and standard measurements are used to position and design the NAC.
Anatomically, the NAC is located at the anterior-most projecting part of the breast mound at the level of the inframammary fold, centered on the reconstructed breast mound.
The nipple has an average projection of 5 mm and the areola has an average diameter of 35 to 45 mm.
POSITIONING
In the operating room, patients are positioned supine with arms at 90 degrees secured to arm boards. Both breasts are prepped into the field to allow for evaluation of symmetry. Patients are secured to the operating table to allow upright evaluation intraoperatively.
In the clinic, patients are positioned supine with arms at sides.
Skate Flap (Nipple) and Full-Thickness Skin Graft (Areola)
The patient is placed in supine position with arms abducted at 90 degrees. Arms are secured on arm boards.
The NAC position is selected at the anterior-most projecting part of the reconstructed breast with the patient in an upright position. In unilateral nipple reconstruction, the NAC is placed symmetrically to the opposite side (FIG 1).
A donor site is chosen for the full-thickness skin graft, which will be used to reconstruct the areola. Commonly used sites include the lateral edge of the mastectomy scar, the lower abdomen, and the groin crease. Additionally, the areolar graft can be taken adjacent to any of the patient’s existing scars.
A 38- or 42-mm nipple sizer is used to mark the areolar skin graft. An ellipse is drawn tangent to the areolar graft to allow linear closure of the donor site.
The areolar skin graft is scored with a knife prior to harvest. The ellipse is then excised as a full-thickness skin graft (FIG 2).
The areolar graft is aggressively defatted with a small sharp scissor, leaving only full-thickness skin behind (FIG 3).
The skate flap is designed at the previously marked site (FIG 4).
A 1- to 1.5-cm circle is drawn at the planned location of the nipple.
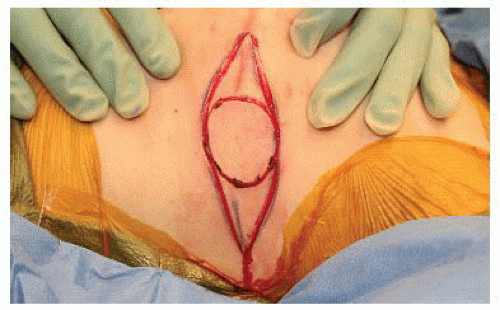
FIG 2 • Areolar skin graft is marked with a 38-mm nipple sizer. An ellipse is drawn tangentially to facilitate linear closure.
A 38- or 42-mm nipple sizer is used to mark the areola centered around the nipple.
A horizontal line is drawn across the circle at the superior edge of the marked nipple.
The upper portion of the circle is crosshatched to mark the area that will be de-epithelialized.
The lower portion of the circle will be raised as the “skate flap” to create the new nipple.
The epidermis is scored along all incisions.
The crosshatched semicircle is de-epithelialized (FIG 5).
The flap is then raised from the edges at the level of the middermis. The deepest layer of dermis is left down in order to provide a vascularized bed for the areolar skin graft (FIG 6).
The flap remains attached to the deep dermis at the marked nipple. The flap is raised in a slightly deeper plane at the center in order to include some fat with the flap to provide bulk (FIG 7).
The corners of the flap are centralized and sutured to the underlying dermis using 5-0 Vicryl Rapide (FIG 8).
The edges of the flap are sutured together using interrupted 5-0 Rapide (FIG 9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



