Neurogenic Thoracic Outlet Syndrome Exposure and Decompression: Supraclavicular
Robert W. Thompson
nChandu Vemuri
DEFINITION
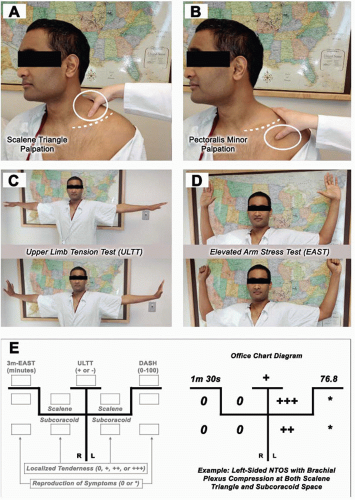
Thoracic outlet syndrome (TOS) is a group of conditions caused by compression of one of the neurovascular structures that serve the upper extremity.1, 2, 3 Neurogenic thoracic outlet syndrome (NTOS) is the most frequent of these, occurring in 85% to 90% of thoracic outlet patients. It is caused by compression and irritation of the brachial plexus nerves within the supraclavicular scalene triangle and/or underneath the pectoralis minor muscle tendon in the subcoracoid space (FIG 1). NTOS tends to occur in patients between the ages of 15 and 40 years, typically manifesting as neck and upper extremity pain, paresthesias, and functional limitations in the ipsilateral arm. Although relatively uncommon, clinical recognition and appropriate treatment are crucial to optimizing outcome in young active individuals with NTOS-related disability.4
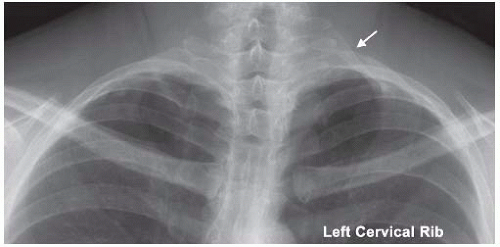
The causes of NTOS include anatomic variations (anomalous scalene musculature, aberrant fibrofascial bands, and/or cervical ribs) and previous neck or upper extremity injury, which promotes scalene/pectoralis muscle spasm, fibrosis, and other pathologic changes.4 These muscular alterations, in turn, lead to compression and irritation of the adjacent brachial plexus nerves. The presence of a cervical rib is often cited as a risk factor for NTOS; however, few NTOS patients (approximately 10%) have a definable cervical rib, and development of NTOS symptoms are rare in cervical rib patients in the absence of predisposing injury.5
NTOS often occurs in individuals involved in occupational or recreational activities requiring repetitive overhead activities with the arms and/or heavy lifting, occasionally aggravated by injury (e.g., motor vehicle collisions or falls upon the outstretched arm). Other predisposing conditions include lowgrade repetitive strain injury (e.g., prolonged keyboard use), poor posture, and dysfunctional shoulder girdle mechanics.
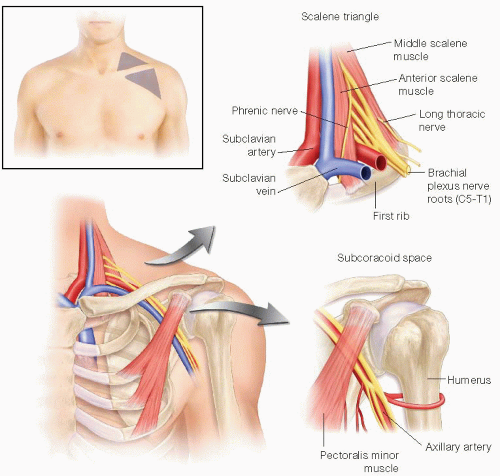
FIG 1 • Anatomy of the thoracic outlet, with emphasis on the supraclavicular scalene triangle and the infraclavicular subcoracoid space.
Surgical treatment for NTOS may be effectively accomplished by several different approaches, including transaxillary 1st rib resection and anterior (supraclavicular) decompression. The supraclavicular approach has long been a mainstay in the surgical
treatment of NTOS, providing excellent exposure for safe and definitive decompression of the relevant neurovascular structures as well as the flexibility to manage the entire spectrum of circumstances that may be encountered intraoperatively.6, 7, 8, 9, 10
Table 1: Differential Diagnosis of Neurogenic Thoracic Outlet Syndrome | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
DIFFERENTIAL DIAGNOSIS
NTOS-related symptoms may mimic or overlap those observed in other upper extremity neurologic and musculoskeletal disorders, expanding the differential diagnosis (Table 1).11,12 Successful intervention requires differentiation of NTOS from other cervical-brachial syndromes as well as optimal patient and procedural selection.13
NTOS should be readily differentiated from venous TOS, which produces marked arm swelling, cyanotic discoloration, and distention of subcutaneous veins around the shoulder and chest wall. Venous TOS often presents clinically as axillarysubclavian vein “effort-related thrombosis” (Paget-Schroetter syndrome). NTOS should also be distinguished from arterial TOS, which causes either fixed subclavian artery obstruction or poststenotic aneurysm formation. The former may precipitate arm or hand pain with exercise (“arm claudication”), the latter aneurysm thrombosis and distal embolization, hand ischemia, rest pain, and/or digital ulceration and necrosis.
Some NTOS patients exhibit severe upper extremity pain and hypersensitivity, with digital swelling and discoloration, suggesting the presence of sympathetic nerve overactivity. In such cases, the coexistence of reflex sympathetic dystrophy (complex regional pain syndrome [CRPS]) should be determined by assessing the symptomatic response to a temporary cervical sympathetic (stellate ganglion) anesthetic block.
PATIENT HISTORY AND PHYSICAL FINDINGS
Symptoms attributable to brachial plexus nerve compression include pain, numbness, and tingling (paresthesia) in the neck, shoulder, arm, and hand. The distribution of symptoms in the hand often extends beyond that expected for either the median or ulnar nerves, involving all fingers. Patients with NTOS attributable to compression at the pectoralis minor tendon often describe upper anterior chest and axillary pain. The intensity of symptoms of NTOS can vary with the extent of upper extremity activity and are usually reliably exacerbated with arm elevation and abduction.
Many NTOS patients experience relatively mild symptoms, with gradual progression in severity punctuated by periodic exacerbations. Others experience steady, progressive worsening of symptoms and related disability. Hand muscle weakness and atrophy (Gilliatt-Sumner hand) are rare, typically following long-standing brachial plexus compression due to an associated cervical rib or similar bony anomaly.
Physical examination typically identifies reproducible tenderness to palpation over the supraclavicular scalene triangle and/or the infraclavicular subcoracoid space (FIG 2).
Most NTOS patients experience recurrent upper extremity symptoms in response to provocative positional maneuvers, such as the upper limb tension test (ULTT) or the 3-minute elevated arm stress test (EAST) (FIG 2). Positional dampening of the radial artery pulse at the wrist during arm abduction and external rotation (Adson’s test) is nonspecific and inaccurate and is generally not useful in establishing or excluding a diagnosis of NTOS.
Directed physical examination is performed to determine the presence of cervical spine degenerative disease or peripheral nerve compression (carpal tunnel and cubital canal syndromes) as potential alternative sources of NTOS-like symptoms as well as evidence of arterial or venous compromise to the affected extremity. Signs of increased upper extremity sympathetic tone are also sought, including digital swelling, discoloration, and skin hypersensitivity (allodynia).
Documentation of patient-reported symptoms and quantification of disability prior to treatment are accomplished by completion of standardized outcomes measurement tools such as the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire and quality-of-life instruments.14 Repeated use of these instruments at various intervals before and after treatment has provided increasing insight into the relative value of alternative management strategies.15
IMAGING AND OTHER DIAGNOSTIC STUDIES
Although imaging and other diagnostic studies may provide helpful ancillary information, there is no definitive test to confirm or exclude the diagnosis of NTOS. Diagnosis remains quintessentially clinical and dependent on experienced pattern recognition.
Plain anteroposterior chest radiographs will identify a cervical rib when present. No other currently available imaging study adds significant value to the clinical diagnosis of NTOS (FIG 3).
Conventional electrophysiologic tests (electromyography and nerve conduction studies) are often performed to exclude peripheral nerve compression disorders or cervical radiculopathy. These tests are usually negative or nonspecific in NTOS and cannot be used to establish or exclude the diagnosis.
Vascular laboratory studies (Duplex ultrasound) may detect alterations in upper extremity blood flow attributable to subclavian artery compression during arm elevation. However, positional subclavian artery compression may represent an incidental and unrelated vascular finding and does not establish a diagnosis of neurogenic or arterial TOS. As they do not assess the presence or severity of brachial plexopathy, vascular laboratory studies add little specificity beyond the clinical diagnostic criteria.
Performance of image-guided anterior scalene and/or pectoralis minor muscle anesthetic blocks may assist the clinical diagnosis of NTOS.16 A positive block, characterized as temporary relief or improvement in the presenting
symptoms, strongly supports the clinical diagnosis of NTOS. A positive block may predict symptomatic relief from surgical decompression and is therefore highly useful in selecting candidates for 1st rib resection. Unfortunately, however, failure of temporary symptom resolution following muscle blockade does exclude the diagnosis of NTOS and should not preclude consideration of surgical management in otherwise compelling clinical candidates.
Initial treatment for NTOS is based on physical therapy to relieve scalene/pectoralis minor muscle spasm, improve
posture, enhance functional limb mobility, strengthen associated shoulder girdle musculature, and diminish repetitive strain exposure in the workplace. Incorrect approaches to physical therapy can result in worsening of symptoms and failure of conservative management. In many NTOS patients, significant symptomatic improvement may be experienced in response to physical therapy, particularly in the first 4 to 6 weeks. Because NTOS is commonly chronic, however, and subject to acute symptomatic “flare ups” (often related to overuse activities or new injury), such patients should continue prescribed physical therapy exercises during long-term follow-up. Patients that fail a conscientious and effective physical therapy, as well as alternative conservative measures, are referred for consideration of surgical intervention.
SURGICAL MANAGEMENT
Supraclavicular decompression (scalenectomy, 1st rib resection, and brachial plexus neurolysis) is recommended on the basis of (1) sound clinical diagnosis of NTOS, (2) substantial resulting disability (interference with daily activities and/or work), and (3) an inadequate response to standard physical therapy. Supraclavicular decompression may also provide relief from persistent or recurrent NTOS symptoms following prior surgery, particularly when continued conservative measures prove ineffective.
For patients with symptoms referable to the subcoracoid space, release of the pectoralis minor tendon should be included in the supraclavicular thoracic outlet decompression procedure. Pectoralis minor tenotomy may also be performed as a stand-alone procedure when nerve compression symptoms are limited to this area.17,18
Decompression should be performed as a staged, sequential procedure in patients with bilateral NTOS symptoms. The initial supraclavicular decompression, with or without pectoralis minor tenotomy, is performed on most symptomatic or dominant extremity. If symptoms remain present or progress, contralateral supraclavicular decompression may be performed within 6 to 12 weeks of the initial procedure. Normal phrenic nerve function should be verified on the side of the previous procedure, by chest fluoroscopic examination, before contralateral intervention.
Preoperative Planning
The supraclavicular surgical site is marked in the preoperative holding area, including the subcoracoid space when concomitant pectoralis minor tenotomy is planned. Prophylactic antibiotics are administered within an hour of the planned procedure.
Positioning
After the induction of general endotracheal anesthesia, the patient is positioned supine with the head of the operating table elevated 30 degrees. The neck is extended and turned to the opposite side; a small inflatable pillow is placed behind the shoulders; and the neck, chest, and affected upper extremity are prepped into the field. The arm is wrapped in stockinette to permit free range of movement during the operation and then held comfortably across the abdomen (FIG 4). Lower extremity sequential compression devices are used for thromboprophylaxis. Neuromuscular blocking agents are not used following the initial induction of anesthesia.
 FIG 4 • Patient position and planned incisions for left-sided supraclavicular thoracic outlet decompression with pectoralis minor tenotomy. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree