Neoplasms of the Parathyroid Glands
The dispersed neuroendocrine system includes two organs that are predominantly or exclusively composed of neuroendocrine cells; parathyroid glands are one and anterior pituitary is the other organ, discussed in Chapter 10.
ANATOMY AND HISTOLOGY OF NORMAL PARATHYROID GLANDS
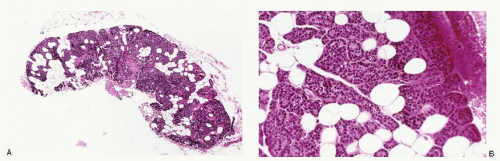
The parathyroid glands, derived from branchial pouches III and IV, are small, red-brown, flattened, ovoid structures, generally measuring 4 to 6 mm in length, 2 to 4 mm in width, and 1 to 2 mm in thickness, with an average combined weight of 120 mg. Most normal adults have four parathyroid glands, the superior pair located about 1 cm above the intersection of the recurrent laryngeal nerve and the inferior thyroid artery. The inferior parathyroids are typically found inferior, posterior, or lateral to the lower pole of the thyroid and sometimes high up on the anterior aspect of the thyroid lobe. The parathyroid glands are highly vascularized and thinly encapsulated. Histologically, the parathyroid gland shows a mixture of parenchyma and adipose tissue (Fig. 9.1A). The parenchyma consists of chief cells, varying numbers of oncocytic cells, and transitional oncocytic cells (Fig. 9.1B). The parenchymal cells are often arranged in a lobular pattern. The chief cells are polyhedral, 8 to 10 mm in diameter, with round central nuclei containing sharp nuclear membrane with coarse chromatin. Their cytoplasm is eosinophilic to amphophilic and often appears clear or vacuolated in formalin-fixed tissues. The cells are rich in glycogen and contain variable amounts of neutral lipid. The chief cells may form solid sheets; branching anastomosing cords; and sometimes small, acinar structures, which may contain eosinophilic periodic acid-Schiff (PAS)-positive material resembling colloid. The stroma contains mature fat cells, blood vessels, and varying amounts of connective tissue, the proportion of which changes with age. The immunoprofile of parathyroid parenchymal cells includes positive reactivity to parathyroid hormone and chromogranin.
The parathyroid cells secrete parathyroid hormone, which, along with the other two hormones, calcitriol (produced in the kidney) and calcitonin (produced in the thyroid), regulates calcium and phosphorus levels.
Neoplasms of the parathyroid mostly include adenomas and carcinomas. The latter are extremely rare. Parathyroid adenomas may also arise in ectopic locations such as thyroid or mediastinum.
PARATHYROID ADENOMA
Parathyroid adenomas are benign neoplasms of the parathyroid glands. They are functional and cause primary hyperparathyroidism due to increased secretions of parathyroid hormone resulting in increased levels of serum calcium. Roughly 80% to 85% of the cases of primary hyperparathyroidism are caused by adenomas. Parathyroid adenomas are more common in women with a male:female ratio of 1:3-4. They occur over a broad age range, the average being 55 years. More than 50% of patients may be asymptomatic and diagnosed incidentally because of high serum levels of calcium. When symptomatic, patients with hyperparathyroidism complain of weakness, fatigue, and muscle weakness. Late effects of hypocalcemia such as nephrolithiasis and osteitis fibrosa cystica are very infrequently encountered. Hypercalcemia may result in calcium deposition in various tissues and organs. With advances in biochemical techniques, serum abnormalities are detected sooner.
ASSOCIATION WITH HEREDITARY SYNDROMES
RADIOLOGIC FINDINGS
Several imaging modalities are used to localize parathyroid gland lesions. These include ultrasonography, CT scanning, MRI, thallium substation scanning, and the recent technetium-99m sestamibi imaging. Ultrasonography is the most frequently used modality for primary hyperparathyroidism. A normal parathyroid gland is typically not seen with ultrasound. A parathyroid adenoma or a carcinoma is seen as a round, elliptical, or oblong hypoechoic mass. These may contain cysts and calcifications. Hyperplastic glands are usually much smaller than adenomas. Ultrasound cannot localize ectopic parathyroids. Thyroid nodules or lymph nodes may be mislabeled as parathyroids.
GROSS AND MICROSCOPIC FEATURES
Parathyroid adenoma involves a single gland. A typical parathyroid adenoma is a thinly encapsulated, tan to reddish-brown neoplasm, homogeneous in consistence with a smooth external surface. Adenomas vary considerably in size and shape. They may be round, ellipsoid, bean or kidney shaped, or flattened and elongated (Fig. 9.2). Larger adenomas may undergo cystic change and may yield fluid contents at fine needle aspiration (FNA) biopsy. Histologically, adenomas are encapsulated neoplasms with compressed normal parenchyma outside the capsule. The growth pattern consists of closely packed chief cells arranged in anastomosing cords, nests, glandular formations, and sheets separated by a delicate network of sinusoids (Fig. 9.3). The dominant cell type is chief cells, often larger than their normal counterpart. The cell outlines are indistinct. Their cytoplasm ranges from faintly eosinophilic to clear and contains abundant glycogen deposits. The nuclei are round and central with dense chromatin and occasional nucleoli. A few cells may contain large, hyperchromatic nuclei.
The adenomas frequently contain cystic structures, which may be empty or filled with PAS-positive, eosinophilic, homogeneous material that strongly resembles colloid. The cells contain glycogen and fat. Argyrophilic granules in the cytoplasm of adenoma cells have been described.
IMMUNOPROFILE
The cells of parathyroid adenoma exhibit positive reactivity to parathyroid hormone, chromogranin A, and low molecular weight cytokeratin and negative reactivity to calcitonin, thyroglobulin, and vimentin.
CYTOPATHOLOGIC FEATURES
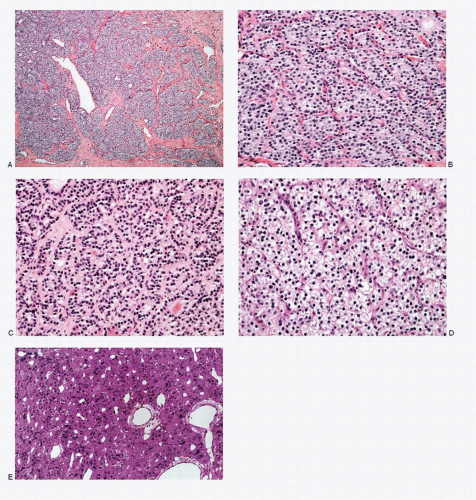
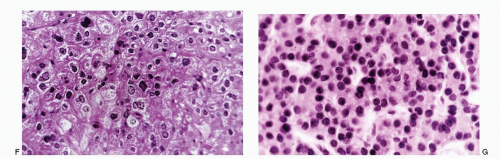
Specimens for the cytologic diagnosis mostly represent fine needle biopsies of the suspected, enlarged parathyroid glands. Not uncommonly, the aspirates are submitted as thyroid FNA biopsies. The aspirate is variably cellular consisting of a large population of small round to cuboidal epithelial cells displayed singly, in loosely cohesive groups, or in thick syncytial type tissue fragments with or without various architectural configurations (Figs. 9.4,9.5,9.6,9.7 and 9.8). They may be monolayered (two-dimensional, Fig. 9.6E), trabecular (Figs. 9.6B and 9.7C), with branching and interdigitating to enclose spaces (Figs. 9.5B,D and 9.6B), or follicular (Figs. 9.4C and 9.6C) or may appear papillary-like with complex branching and frayed edges (Fig. 9.7D). Frequently, the extreme crowding and overlapping of nuclei within a tissue fragment result in a three-dimensional pattern (Figs. 9.4A and 9.7C). Another characteristic feature of parathyroid adenomas is the branching network of capillaries. The neoplastic cells are often seen along the capillaries (Fig. 9.7C; see Fig. 9.12C). The parathyroid adenoma cells are round to cuboidal, slightly smaller than normal thyroid follicular cells, measuring 6 to 7 mm in diameter. Their nuclei are round and uniform, containing coarsely granular chromatin (salt-pepper type) and micronucleoli. Nuclear pleomorphism is occasionally
present. Nuclear molding has been described as a “hitherto unreported diagnostic feature” but has not been documented by others. The parathyroid chief cells have scanty, pale cytoplasm with ill-defined cell borders and are frequently displayed as stripped nuclei, presenting a lymphocyte-like pattern (Fig. 9.6B). Occasionally single vacuoles are noted within the cytoplasm. The oncocytic cells contain appreciable amounts of granular cytoplasm and morphologically resemble Hürthle cells of the thyroid but for their smaller size. Although a monomorphic cellular pattern is commonly seen in adenomas, pleomorphic size and shapes may occasionally be encountered.
present. Nuclear molding has been described as a “hitherto unreported diagnostic feature” but has not been documented by others. The parathyroid chief cells have scanty, pale cytoplasm with ill-defined cell borders and are frequently displayed as stripped nuclei, presenting a lymphocyte-like pattern (Fig. 9.6B). Occasionally single vacuoles are noted within the cytoplasm. The oncocytic cells contain appreciable amounts of granular cytoplasm and morphologically resemble Hürthle cells of the thyroid but for their smaller size. Although a monomorphic cellular pattern is commonly seen in adenomas, pleomorphic size and shapes may occasionally be encountered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree