Neck Exploration for Trauma
Kevin D. Helling
Carlos A. Pelaez
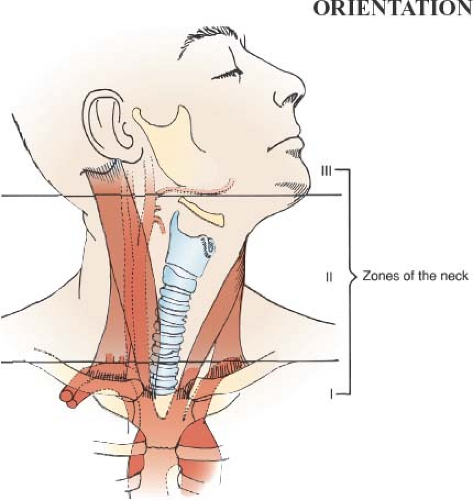
Traumatic injuries to the neck can be complicated and difficult to treat as they threaten both life and function. Due to the close proximity of multiple important structures, a systematic approach to exploration and repair must be employed. In order to accomplish this, the neck is divided into three zones numbered in a caudocranial fashion (Fig. 13.1).
Zone I lies between the cricoid cartilage superiorly and the thoracic inlet (clavicles and sternal notch) inferiorly. Injuries in this area of the neck can also extent into the chest and mediastinum. Therefore, the surgeon must have high index of suspicion for injuries at this level and also be prepared to explore the chest and mediastinum. Hemodynamically
unstable patients are taken directly to the operating room, whereas stable patients should first undergo further evaluation to characterize their injuries. Computed tomography with angiography (CTA) is a useful method to evaluate for vascular injuries. Angiography is also diagnostic and provides therapeutic options. Chest radiography is done to look for associated hemopneumothorax. Esophageal contrast studies with or without endoscopy, as well as bronchoscopy, are necessary to complete the nonoperative evaluation. These studies may be selectively omitted if the CTA reveals the path of penetration to be remote from the aerodigestive tract. Positive findings direct operative repair. If operative intervention is required, exposure can be difficult and usually requires a combination of incisions to gain access to the neck and mediastinum. Most injuries can be managed by a median sternotomy with extension to the neck over the anterior aspect of the sternocleidomastoid muscle. A supraclavicular incision, removal of the clavicle or a trapdoor thoracotomy (where an incision is made from midclavicular to the sternal notch, then carried along the midline onto the sternum to the fourth intercostal space, and out along the fourth interspace to the midaxillary line) are sometimes required. These approaches are described at the end of the chapter.
unstable patients are taken directly to the operating room, whereas stable patients should first undergo further evaluation to characterize their injuries. Computed tomography with angiography (CTA) is a useful method to evaluate for vascular injuries. Angiography is also diagnostic and provides therapeutic options. Chest radiography is done to look for associated hemopneumothorax. Esophageal contrast studies with or without endoscopy, as well as bronchoscopy, are necessary to complete the nonoperative evaluation. These studies may be selectively omitted if the CTA reveals the path of penetration to be remote from the aerodigestive tract. Positive findings direct operative repair. If operative intervention is required, exposure can be difficult and usually requires a combination of incisions to gain access to the neck and mediastinum. Most injuries can be managed by a median sternotomy with extension to the neck over the anterior aspect of the sternocleidomastoid muscle. A supraclavicular incision, removal of the clavicle or a trapdoor thoracotomy (where an incision is made from midclavicular to the sternal notch, then carried along the midline onto the sternum to the fourth intercostal space, and out along the fourth interspace to the midaxillary line) are sometimes required. These approaches are described at the end of the chapter.
Zone II extends from the angle of the mandible superiorly to the cricoid cartilage inferiorly. Injuries to this zone that penetrate the platysma generally warrant exploration, and prompt surgery is required in unstable patients. Injuries superficial to the platysma require only local exploration and irrigation. Massive hemorrhage possible as a result from injury to the common carotid artery or its branches, vertebral artery, jugular vein, or a combination of them. Initial control of bleeding can be accomplished by manual pressure; blind clamp application for hemorrhage control is to be condemned. Stable patients may undergo further preoperative evaluation by duplex ultrasonography, CTA or angiography, followed by radiographic or endoscopic hypopharyngeal and esophageal evaluation. The larynx and trachea must be examined by fiberoptic or rigid endoscopy if appropriate signs or symptoms are present, such as cervical subcutaneous emphysema, stridor, respiratory difficulties, hemoptysis, or hoarseness. A selective approach to exploration may be appropriate if diagnostic studies yield negative results. Zone II injuries are explored through a neck incision over the anterior border of the sternocleidomastoid muscle.
Zone III extends from the skull base superiorly to the angle of the mandible inferiorly. Operative exposure can be difficult. If possible, patients with injuries in zone III should undergo preoperative imaging to allow better operative strategy and planning. Unstable patients should be taken expeditiously to the operating room. A Fogarty or Foley catheter may be gently inserted into the wound and its balloon inflated to the point of hemorrhage control. If this results in hemodynamic improvement, diagnostic and therapeutic arteriography may then be possible. In the case of profound bleeding, operative management is focused on obtaining proximal and distal control of the bleeding vessel. Obtaining distal control near the skull base or vertebrae may be exceedingly difficult if not impossible. Placement of bone wax into the bleeding orifice can accomplish distal control in injuries in which the distal end of the vessel cannot be reached to ligate or repair the vessel. When nonoperative evaluation is pursued, fiberoptic endoscopic evaluation of the pharyngeal area should be conducted as well.
SCORE™, the Surgical Council on Resident Education, classified neck exploration for trauma as a “COMPLEX” procedure.
STEPS IN PROCEDURE
Position the patient with neck extended and the head turned laterally
Place a roll under the shoulders for better support
Prepare and drape the neck and chest in case sternotomy or thoracotomy is required
Perform an oblique incision through the skin and platysma, along anterior border of sternocleidomastoid muscle, curving posteriorly as the incision approaches the angle of the mandible to avoid injury to the marginal mandibular nerve
Retract sternocleidomastoid muscle laterally to expose carotid sheath
Explore carotid sheath if hematoma is encountered
Retract thyroid medially after dividing middle thyroid vein
Expose and inspect esophagus and trachea by retracting the carotid sheath laterally
Close incision in layers
Obtain hemostasis of all small muscles and subcutaneous bleeders
Place drain if contaminated wound or any concern for possible esophageal injury
LIST OF STRUCTURES
Platysma
Sternocleidomastoid muscle
Trachea
Esophagus
Thyroid gland
Carotid sheath
Carotid artery (common, internal, and external)
Internal jugular vein
Facial vein
Vagus nerve
Recurrent laryngeal nerve
Neck exploration can be thought of as a means of systematically inspecting two main compartments in the neck. The vascular compartment includes the common carotid, internal carotid, external carotid, and vertebral arteries, as well as the internal jugular vein and its branches. The visceral compartment includes the pharynx and esophagus, larynx and trachea, thyroid, parathyroids, and associated structures. Even when preoperative clinical findings or diagnostic studies point to injury of a specific structure, a complete and systematic examination of all structures should be performed.
Positioning of the Patient and Skin Incision (Fig. 13.2)
Technical and Anatomic Points
Position the patient supine with the head turned slightly away from the injury or neutral if cervical spine injury is possible. Recently, the routine use of cervical spine collar in isolated penetrating neck trauma has been called into question due to the propensity of the collar to obscure injuries, and the surgeon must evaluate the entire circumference of the neck to avoid missing wounds, hematomas, tracheal abnormalities, or spinal
defects. Once the head is positioned appropriately, prepare and drape both sides of the neck and the entire chest, as exploration of the mediastinum through partial or complete median sternotomy or anterolateral thoracotomy may be necessary. Prepare and drape both groins to allow vascular access and harvest of the saphenous veins in the event they are needed for vessel repair.
defects. Once the head is positioned appropriately, prepare and drape both sides of the neck and the entire chest, as exploration of the mediastinum through partial or complete median sternotomy or anterolateral thoracotomy may be necessary. Prepare and drape both groins to allow vascular access and harvest of the saphenous veins in the event they are needed for vessel repair.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree