Morphea/Scleroderma
Sudeep Gaudi, MD
Drazen M. Jukic, MD, PhD
Key Facts
Terminology
Scleroderma limited to skin, subcutaneous tissue, and underlying muscle and bone
Etiology/Pathogenesis
Environmental trigger in a genetically predisposed individual lends to launch of cytokine-driven profibrotic cascade following microvascular injury
Clinical Issues
Classified into 5 subtypes according to varying clinical presentations
Possibly complicated by muscular atrophy, joint contractures, and limb length discrepancies
Macroscopic Features
Smooth, indurated plaques with variable postinflammatory pigmentary alteration
Microscopic Pathology
Early superficial and deep perivascular predominantly lymphocytic infiltrate
Subsequent resolution of inflammation and development of obliterative sclerotic dermal collagen bundles
Top Differential Diagnoses
Systemic scleroderma
Scleredema
Graft vs. host disease (GVHD), sclerodermiform chronic variant
Scleromyxedema
Radiation dermatitis
Nephrogenic fibrosing dermopathy
Lichen sclerosus et atrophicus
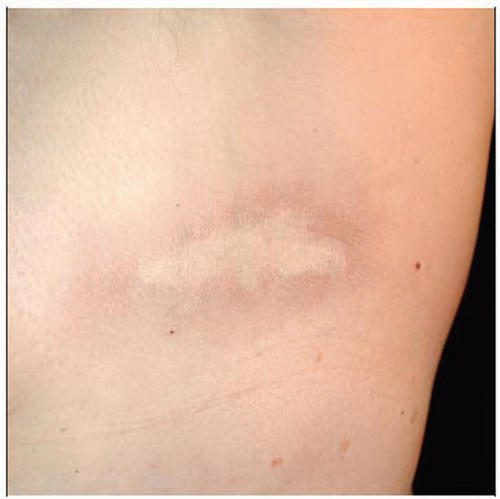 A lesion of morphea en plaque is characteristically located on the trunk under an area of pressure (bra line). Note the violaceous peripheral rim (“lilac ring”) and white, sclerotic center. |
TERMINOLOGY
Synonyms
Morphea: Localized scleroderma
Definitions
Most common subtype of scleroderma (group of fibrosing disorders that result from imbalance between collagen production and destruction)
Clinically heterogeneous disease process that is localized to the skin and subcutaneous tissues with possible involvement of underlying muscle and bone
Underlying central nervous system may also be affected in cases of face and head involvement
ETIOLOGY/PATHOGENESIS
Multifactorial
Precise etiology remains mystery
Evidence suggests microvascular injury induces profibrotic cytokines following environmental insult in genetically predisposed individual
These cytokines lead to increased collagen production and decreased collagen destruction
Genetic
Possible host factors include autoimmunity and microchimerism
Environmental
Possible insults include radiation, trauma, medications, and infection (potential link to certain Borrelia species, particularly in Europe)
CLINICAL ISSUES
Epidemiology
Incidence
0.4-2.7 per 100,000 people
Age
Prevalence is equal in adults and children
Approximately 90% of afflicted children present between 2 and 14 years of age
Mean age of presenting adults is mid-40s
Gender
About 2-4x more common in females than males
Ethnicity
Affects all races, but more common in whites
Approximately 70-80% of patients examined in ethnically heterogeneous clinical populations are white
Presentation
Circumscribed (a.k.a. morphea en plaque)
Most common subtype in adults
Patients typically present with less than 3 plaques, predominantly located on trunk in areas of pressure (e.g., around waist, under bra line)
Lesions tend to soften over period of 3-5 years
Superficial variant: More common; limited to epidermis and dermis
Deep variant (morphea profunda): Affects dermis and subcutaneous tissue, with variable involvement of underlying fascia and muscle; overlying epidermis may not be involved
Linear
Most common subtype in children
En coup de sabre variant: Linear induration of paramedian forehead; affects dermis with variable involvement of underlying muscle, bone, and ocular and central nervous systems
Parry-Romberg variant: Also known as progressive hemifacial atrophy; patients develop atrophy of dermis, subcutaneous tissue, and underlying muscle and bone of unilateral face
Limb variant: Linear induration of limbs; affects dermis, subcutaneus tissue, and underlying muscle and bone causing muscle atrophy, limb length discrepancies, and joint contractures
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




