Multiple nodules on chest x-ray
Cough
Dyspnea
Lung is most common site of metastases for soft tissue sarcomas from trunk and extremities
Good prognosis in patients with resectable tumors and in patients with metastases from uterine leiomyosarcoma
Spindle cell sarcomas
Most common types are leiomyosarcoma, myxofibrosarcoma, synovial sarcoma, osteosarcoma, malignant schwannoma
Epithelioid cell sarcomas
Most common types include epithelioid sarcoma, angiosarcoma, alveolar soft parts sarcoma
Pleomorphic cell sarcomas
Most common type is pleomorphic high-grade sarcoma (so-called malignant fibrous histiocytoma)
Small round blue cell sarcomas
Most common types include rhabdomyosarcoma, Ewing sarcoma/PNET, round cell liposarcoma, small desmoplastic round cell tumor
Immunohistochemistry is very helpful tool for differential diagnosis
Most important distinction is between sarcomatoid carcinoma (keratin positive) and true spindle cell sarcoma
Formation of sarcomatous nodules in the lung as a result of hematogenous spread from distant sites
Multiple nodules on chest x-ray
Cough
Dyspnea
Hemoptysis
Lung is most common site of metastases for soft tissue sarcomas from trunk and extremities
Most common primary source of lung metastasis from soft tissue sarcomas is from lower extremities
Most common types of metastatic sarcomas to the lung are
Leiomyosarcoma (21%)
Pleomorphic high-grade sarcoma (malignant fibrous histiocytoma) (18%)
Synovial sarcoma (14%)
Liposarcoma (12%)
Surgical approaches
Surgical excision for solitary or peripheral lesions
Adjuvant chemotherapy for multiple and bilateral lesions
Good prognosis in patients with resectable tumors and in patients with metastases from uterine leiomyosarcoma
Metastasectomy can double median survival and 3-year survival for patients with metastatic soft tissue sarcoma
Patient age > 50 years old is adverse prognostic factor
Location
Usually distributed in lower lobes, bilaterally
Size
Variable size, from microscopic to large masses (> 5 cm in diameter)
Best imaging tool to characterize the number of tumor nodules, location, and resectability
Bilateral nodules, mostly small and interstitial, most commonly in lower lobes
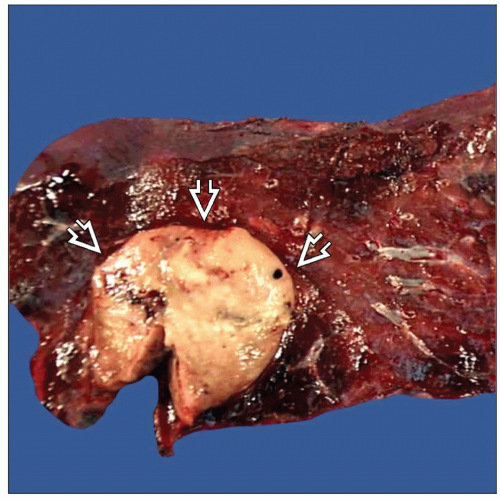
Gray-white, whorled rubbery tissue that bulges from cut surface
Can show extensive hemorrhage and necrosis
May show prominent cystic changes
Can have myxoid or mucinous cut surface or may be rubbery, like cartilage
Metastases of osteosarcoma may be gritty and hard
May vary depending on type of sarcoma
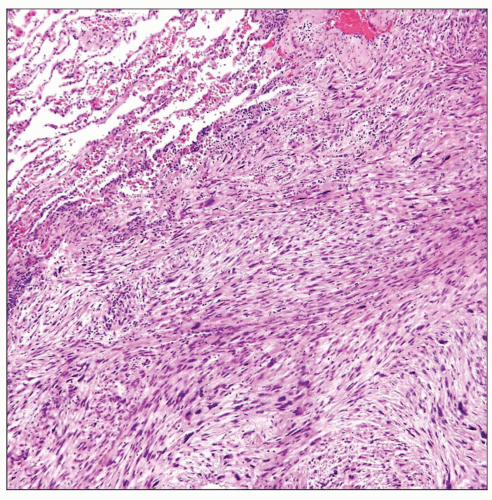
Spindle cell sarcomas
Fascicles of atypical spindle cells with variable cellularity, pleomorphism, and mitotic activity
Most common types: Leiomyosarcoma, myxofibrosarcoma, synovial sarcoma, malignant peripheral nerve sheath tumor, and osteosarcoma
Epithelioid cell sarcomas
Sheets of large round to polygonal atypical cells with abundant cytoplasm resembling a carcinoma
Most common types include epithelioid sarcoma, angiosarcoma, and alveolar soft part sarcoma
Pleomorphic cell sarcomas
Sheets of large pleomorphic or anaplastic tumor cells with atypical nuclei and abnormal mitoses
Most common type is pleomorphic high-grade sarcoma (so-called malignant fibrous histiocytoma)
Small round blue cell sarcomas
Sheets of atypical, undifferentiated small round blue cells
Most common types include rhabdomyosarcoma, Ewing sarcoma/PNET, small desmoplastic round cell tumor, and round cell liposarcoma
Very helpful tool for differential diagnosis
Most important distinction is between sarcomatoid carcinoma (keratin positive) and a true spindle cell sarcoma
Specific antibodies may be of value for further subtyping of tumor and defining cell lineage
Chromosomal translocations can be associated with specific types of sarcomas, i.e., t(x;18) in synovial sarcoma
Specific chimeric fusion products resulting from genetic translocations can be detected using molecular techniques FISH and PCR can be used to detect the EWSR-1 fusion product in Ewing sarcoma or the SYT-SXX fusion product in synovial sarcoma
Can resemble a sarcoma due to mixed spindle and epithelioid cell morphology
Prominent “nesting” pattern, intracellular melanin pigment, and large eosinophilic nucleoli are characteristic
Tumor cells react strongly with S100 protein and melanocytic-associated markers (HMB-45, Melan-A, tyrosinase, and MiTF)
Any type of soft tissue sarcoma can arise as a primary in lung; however, this is an extremely rare event
Thorough clinical history to rule out possibility of late or occult metastasis from soft tissue site is indispensable for diagnosis
Sheets of pleomorphic and atypical spindle cells, usually in association with preexisting adenocarcinoma or squamous cell carcinoma
Extensive sampling is recommended to identify well-differentiated adenocarcinoma or squamous cell carcinoma component
Spindle cells are strongly positive for epithelial markers (cytokeratins, EMA, MOC31, etc.)
Biphasic malignant neoplasm composed of a true malignant epithelial component (squamous or adenocarcinoma) and true sarcoma component
Epithelial component must stain with epithelial markers or show ultrastructural features of epithelial differentiation
Sarcomatous component must resemble well-defined types of sarcomas or be devoid of reactivity for epithelial markers
Biphasic malignant neoplasm with epithelial component resembling fetal lung and spindle cell sarcomatous component
Epithelial component is positive for cytokeratin and TTF-1
Sarcomatous component stains as specific subtype of sarcoma or is composed of primitive spindle cell sarcoma, NOS
Metastatic sarcomas to the lung are much more frequent than primary lung sarcomas
Obtaining prior history of soft tissue sarcoma elsewhere is most important step for establishing diagnosis of metastasis
Metastases of soft tissue sarcomas to the lungs can change their morphology at the metastatic site
Clinicopathologic correlation is most important step for establishing correct diagnosis
Immunohistochemistry | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree