Metaplastic, Dysplastic, and Premalignant Lesions
Metaplastic, dysplastic, and other premalignant proliferations are often precursors to lung cancers. These lesions are important to recognize for diagnostic purposes, for their importance in understanding the development of cancer, and for potential early therapeutic interventions. Premalignant lesions include squamous dysplasia and carcinoma in situ, atypical adenomatous hyperplasia, diffuse idiopathic pulmonary neuroendocrine-cell hyperplasia, and bronchiolar columnar-cell dysplasia.
Part 1 Squamous Metaplasia and Dysplasia and Carcinoma in Situ
Squamous metaplasia, squamous dysplasia, and carcinoma in situ are lesions of the bronchial epithelium that precede invasive carcinoma. Squamous metaplasia, the physiologic repair process of injured bronchial epithelium, is reversible, whereas squamous dysplasia and carcinoma in situ are specific preneoplastic lesions. The spectrum of histologic changes representing the stepwise progression of airway epithelium toward invasive carcinoma is often not identified in individual lung carcinoma cases.
Subpart 1.1 Squamous Metaplasia
Alvaro C. Laga
Timothy C. Allen
Philip T. Cagle
Squamous metaplasia is a frequent epithelial alteration of the tracheobronchial mucosa. Its histogenesis may be related to chronic inflammation and injury of the bronchial epithelium, which leads to replacement of the normal ciliated columnar epithelium by a squamous epithelium. Therefore, squamous metaplasia may be seen in purely inflammatory settings such as infection or bronchiectasis. Squamous metaplasia may also be a preneoplastic lesion. In this situation, squamous metaplasia may be the result of exposure to tobacco smoke, in which case it is potentially a precursor after many years to the morphologic
progression to bronchogenic carcinoma through varying degrees of dysplasia. Squamous metaplasia due to tobacco exposure may or may not progress to dysplasia and eventually carcinoma. Because of the “field effect” of tobacco smoke on the bronchial mucosa, multiple areas of squamous metaplasia may be seen in smokers, some of which may progress to dysplasia or eventually carcinoma, whereas others may not. Squamous metaplasia or varying degrees of dysplasia may be present at the margins of a carcinoma and a biopsy may be performed on it when one is not performed on the carcinoma itself. Early changes include a loss of the ciliated columnar epithelium, basal cell hyperplasia, and formation of a low columnar epithelium without cilia.
progression to bronchogenic carcinoma through varying degrees of dysplasia. Squamous metaplasia due to tobacco exposure may or may not progress to dysplasia and eventually carcinoma. Because of the “field effect” of tobacco smoke on the bronchial mucosa, multiple areas of squamous metaplasia may be seen in smokers, some of which may progress to dysplasia or eventually carcinoma, whereas others may not. Squamous metaplasia or varying degrees of dysplasia may be present at the margins of a carcinoma and a biopsy may be performed on it when one is not performed on the carcinoma itself. Early changes include a loss of the ciliated columnar epithelium, basal cell hyperplasia, and formation of a low columnar epithelium without cilia.
Cytologic Features
Small elliptical acidophilic squamous metaplastic cells with dark nuclei.
Aggregates of cells with similarly sized nuclei and focal keratinization are characteristic.
Histologic Features
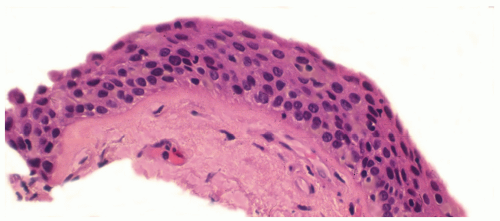
Mounds or aggregates of bland squamous epithelial cells lining the airways and/or airspaces.
Necrosis, keratin pearl formation, and invasion of surrounding parenchyma do not occur.
Regenerative atypical squamous metaplasia may occlude mucous bronchial glands with plugs of squamous epithelium.
Subpart 1.2 Squamous Dysplasia
Alvaro C. Laga
Timothy C. Allen
Philip T. Cagle
Squamous atypia of the bronchial mucosa may be the result of inflammation or injury to the bronchial mucosa, or it may be a step in the morphologic progression from normal bronchial epithelium to carcinoma due to tobacco smoke exposure. In squamous dysplasia, cellular atypia progresses through mild, moderate, and severe dysplasia toward carcinoma in situ, analogous to the progression of squamous metaplasia through increasing degrees of dysplasia to carcinoma in situ seen with cervical carcinoma. With increasing degrees of squamous dysplasia, the degree of cytologic atypia increases and the degree of thickness of the squamous metaplasia exhibiting dysplasia increases. Similar to squamous metaplasia, squamous dysplasia may be multifocal in the bronchial mucosa of smokers, with some foci potentially progressing to more severe degrees of dysplasia or carcinoma over an extended period of time. As with squamous metaplasia, squamous dysplasia due to tobacco smoke does not always progress to carcinoma, and squamous dysplasia may be seen at the periphery of a carcinoma. On occasion squamous dysplasia at the margin of a carcinoma may be sampled on endobronchial biopsy rather than the adjacent carcinoma.
Cytologic Features
Mild dysplasia may show small aggregates of cells with slight size variation, maintained polarity, and inconspicuous nucleoli.
In moderate dysplasia there is noticeable pleomorphism, and occasional cells may show loss of polarity. Nuclei are more hyperchromatic than in mild dysplasia but nucleoli are rarely found.
In severe dysplasia there is an increased nuclear to cytoplasmic ratio greater than in moderate dysplasia, there is loss of cell polarity, nuclear chromatin is greatly increased in all cells accounting for marked hyperchromatism, and prominent nucleoli may be found occasionally.
Histologic Features
Mounds or aggregates of atypical (dysplastic) cells lining the airspaces.
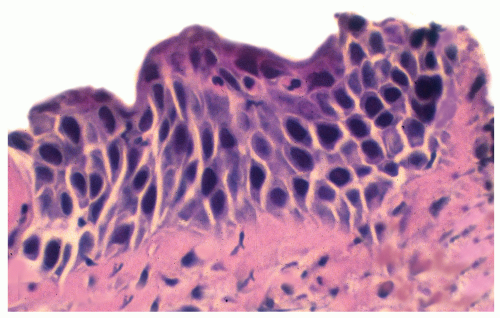
Mild dysplasia contains minimal architectural and cytologic changes, limited to the lower third of the epithelium, with rare to absent mitotic figures and vertically oriented nuclei.
Moderate dysplasia shows partial maturation of squamous cells from the base to the luminal surface, with the basilar zone occupying approximately two-thirds of the epithelium. It exhibits more cytologic atypia, with vertically oriented nuclei and mitotic figures present in the lower third of the epithelium.
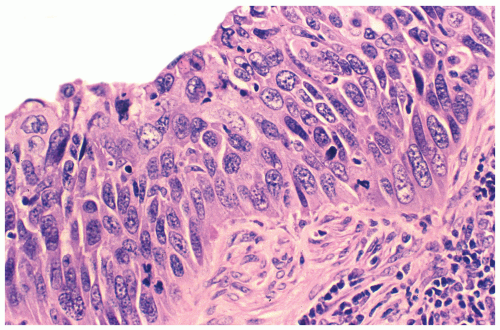
Severe dysplasia shows marked cellular pleomorphism with coarse chromatin and cell maturation and flattening present only in the upper third of the epithelium. Mitotic figures are present in the lower two-thirds of the epithelium.
Necrosis, keratin pearl formation, and invasion of surrounding parenchyma do not occur.
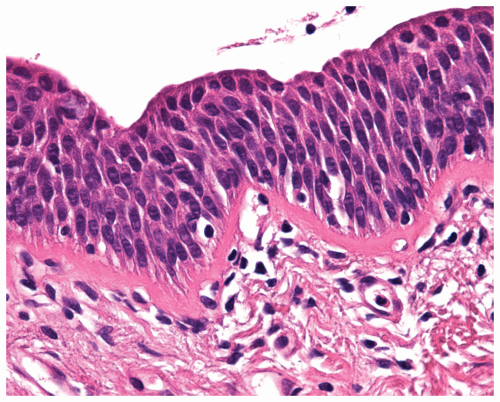 Figure 14.2 Moderate squamous dysplasia shows partial maturation of cells with vertically oriented nuclei. |
Subpart 1.3 Carcinoma in Situ
Alvaro C. Laga
Timothy C. Allen
Philip T. Cagle
In carcinoma in situ, cellular atypia has advanced from severe dysplasia to a full-thickness mucosal abnormality, with an intact basement membrane (no invasion). Grossly, bronchial mucosa may show slight granularity and papillation, or it may be indistinguishable from normal mucosa. Carcinoma in situ may overlap considerably with severe squamous dysplasia, and a range of dysplastic findings may occur in any specific case. Eventually, carcinoma in situ may invade the underlying submucosa as a superficially invasive carcinoma and then beyond as an invasive carcinoma.
Cytologic Features
Marked nuclear size and shape variation.
The nuclear membrane often shows irregularity, infolding, and thickening.
The nuclear-to-cytoplasm ratio is very high, and the cells are less cohesive than the cells of severe dysplasia.
Many single cells or loose aggregates are noted in cytologic preparations.
Histologic Features
Carcinoma in situ is characterized by full-thickness mucosal atypia with intact underlying basement membrane.
Cytologic atypia is marked, and cellular maturation is absent.
Mucosal thickening may occur, and bulbous masses of atypical cells may be present.
Carcinoma in situ may extend into submucosal gland ducts.
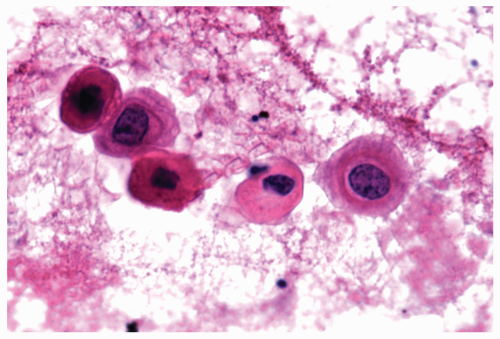 Figure 14.4 Cytology figure of carcinoma in situ shows single cells with a high nuclear to cytoplasmic ratio, irregular nuclear membrane, and large and prominent chromatin clumps. |
Part 2 Squamous Papilloma and Papillomatosis
Alvaro C. Laga
Timothy C. Allen
Philip T. Cagle
Squamous papillomas are rare endobronchial lesions, usually solitary and generally benign, that have been associated with human papilloma virus. Most are exophytic, but inverted variants very rarely occur. Exophytic squamous papillomas are generally wart-like lesions that often protrude into the bronchial lumen. Most present with airway obstruction, which may be incidental, and peripheral lesions may produce incidental cavitary solitary masses.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree