Mesenteric Revascularization with Superior Mesenteric Artery Embolectomy and Other Strategies
Rachael Nicholson
Jose E. Torres
Acute occlusion of the superior mesenteric artery (SMA) can be a result of embolic or thrombotic phenomena. No matter the offending cause, prompt evaluation and intervention is warranted because of the high morbidity and mortality associated with ischemic bowel. Etiology will often determine the approach to intervention. Options for restoration of blood flow fall within the wide spectrum of open, hybrid, and endovascular techniques, including open embolectomy, mesenteric bypass, retrograde stenting of the SMA, and endovascular revascularization.
SCORE™, the Surgical Council on Resident Education, classified superior mesenteric artery embolectomy as an “ESSENTIAL UNCOMMON” procedure.
STEPS IN PROCEDURE
SMA Embolectomy
Vertical midline abdominal incision
Retract omentum and transverse colon cephalad
Small bowel caudad and to right
Mobilize the ligament of Treitz
Palpate the middle colic artery and trace it to the root of the mesentery to locate the SMA
Incise the peritoneum longitudinally along the course of the SMA
Dissect the SMA, preserving branches, and loop with silastic bands
Assure systemic heparinization
Transverse arteriotomy with a 11-blade knife and extend it a few millimeters with Potts scissors
Pass an appropriately sized Fogarty catheter proximally, inflate the balloon and pull back to extract clot
Repeat distally
Flush the lumen with heparinized saline
Close the arteriotomy with interrupted 6-0 monofilament suture
If there is concern for narrowing the lumen, consider a vein patch for closure
Assess Doppler signals
Proximal and distal to the arteriotomy site
Site of arteriotomy
Intestinal branches
Evaluate the bowel for viability and consider a second look laparotomy depending on the appearance of the bowel
Pitfalls and Complications
Bowel perforation
Necrotic bowel
Ischemic stricture
Gastrointestinal bleed
Short gut syndrome
Abdominal compartment syndrome
Loss of abdominal domain
SMA dissection, thrombosis, spasm
Distal embolization
Percutaneous access complications of hemorrhage, pseudoaneurysm, dissection and thrombosis
List of structures
Superior mesenteric artery
Aorta
Middle colic artery
Transverse colon
Duodenum
Ligament of Treitz
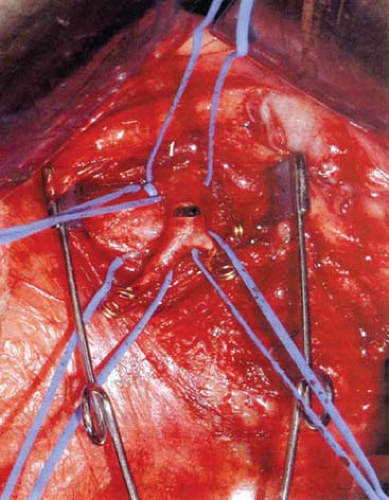
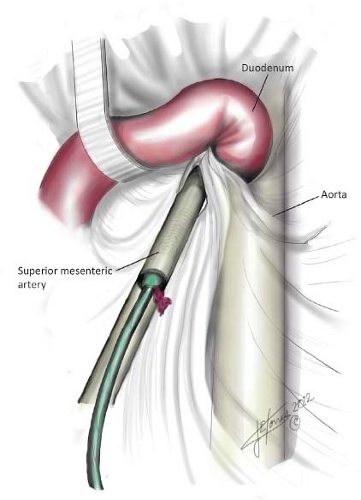
Exposure of Superior Mesenteric Artery (Fig. 89.1)
Technical Points
Optimal exposure is provided by a vertical midline incision. Retract the transverse colon and omentum upward, and the small intestine, including mesentery, downward and to the right to expose the SMA. Mobilize the ligament of Treitz to provide wide exposure. Normally, the artery is easy to locate by its size and pulsation; however, when occluded it may be a bit difficult to find. Palpate the middle colic artery and trace it to the root of the mesentery to locate the SMA. Incise the peritoneum on the mesentery longitudinally along the course of the SMA (Fig. 89.1). Dissect the SMA, preserving its branches. Pass silastic vessel loops around the proximal artery, distal artery, and any branches in the field. The patient should already be systemically heparinized, but if not, administer heparin. Make a transverse arteriotomy with a 11-blade knife and extend it a few millimeters with Potts scissors. Typically, clot will be encountered in the artery (Fig. 89.2).
Pass an appropriately sized Fogarty catheter proximally (typically a 3-French catheter), inflate the balloon and pull back to extract clot (Fig. 89.3). Flush the vessel with heparinized saline and place a small Yassargil clamp proximal to the arteriotomy once blood return is established. In a similar manner, pass the Fogarty catheter distally to remove clot. Extreme care should be taken not to overinflate the balloon with this maneuver, as the mesenteric vessels are fragile and easily injured. Flush the vessel with heparinized saline and place a small Yassargil clamp distal to the arteriotomy once blood return is established. Close the arteriotomy with interrupted 6-0 monofilament suture. Flash the clamps and flush the lumen with heparinized saline prior to the suture line being tightened.
If the artery is stenotic or there is concern for narrowing the lumen, a longitudinal arteriotomy should be used rather than a transverse one. A limited endarterectomy can be performed if there is a stenotic lesion by using a Freer elevator to remove the plaque. The distal endpoint of the endarterectomy site is inspected and any loose ends of intima are being trimmed and/or tacked using a 6-0 or 7-0 Prolene suture. The arteriotomy is closed by using a small piece of vein, usually harvested from the greater saphenous vein. The vein is opened longitudinally after being flushed with heparinized saline. Any valves are removed with fine Potts scissors. The vein is cut to length and sewn to the arteriotomy with 6-0 Prolene suture starting by tacking the vein patch in place at each apex and then running the suture line toward the middle of the patch on either side. Prior to the suture line being tied, the clamps are flashed and then reapplied. The lumen is flushed with heparinized saline and the suture line is then tightened.
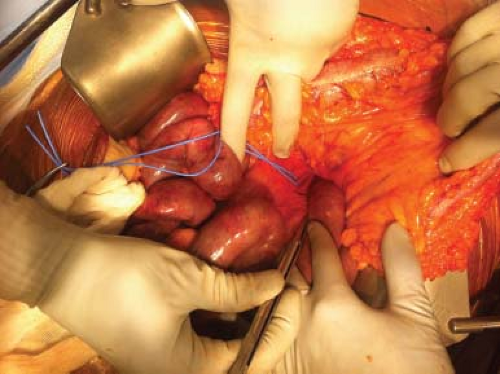 Figure 89.1 Exposure of SMA with transverse colon reflected cephalad, silastic loop around SMA, and proximal small bowel to the patient’s left |
Assess Doppler signals proximal and distal to the arteriotomy site as well as at the site itself. There should be Doppler signals within the intestinal branches and along the mesenteric and antimesenteric borders of the bowel. Evaluate the bowel for viability and consider a second look laparotomy depending on the appearance of the bowel.
Anatomic Points
The SMA supplies the distal duodenum, small intestine, large intestine to the splenic flexure, and the head and body of the
pancreas. It arises anteriorly from the aorta at the level of the first lumbar vertebral body at an acute angle, making it a particularly susceptible target for emboli relative to the celiac and inferior mesenteric arteries which originate off the aorta in more perpendicular conformations. Proximally, it lies posterior to the pancreas and then travels anterior to the fourth portion of the duodenum. Its first branch is the inferior pancreaticoduodenal artery, which has an anterior and posterior branch that anastomose with the anterior and posterior superior pancreaticoduodenal arteries, derived from the gastroduodenal artery, to form the pancreaticoduodenal arcades, providing a collateral pathway to the celiac artery distribution. There are then between 10 and 15 jejunal and ileal branches which come off the SMA as it travels toward the right lower quadrant. These branches create a series of arcades as they divide at right angles which then communicate with adjacent jejunal branches. Successive arcades then divide to supply the anterior and posterior surfaces of the intestine, oriented perpendicular to the long axis of the bowel.
pancreas. It arises anteriorly from the aorta at the level of the first lumbar vertebral body at an acute angle, making it a particularly susceptible target for emboli relative to the celiac and inferior mesenteric arteries which originate off the aorta in more perpendicular conformations. Proximally, it lies posterior to the pancreas and then travels anterior to the fourth portion of the duodenum. Its first branch is the inferior pancreaticoduodenal artery, which has an anterior and posterior branch that anastomose with the anterior and posterior superior pancreaticoduodenal arteries, derived from the gastroduodenal artery, to form the pancreaticoduodenal arcades, providing a collateral pathway to the celiac artery distribution. There are then between 10 and 15 jejunal and ileal branches which come off the SMA as it travels toward the right lower quadrant. These branches create a series of arcades as they divide at right angles which then communicate with adjacent jejunal branches. Successive arcades then divide to supply the anterior and posterior surfaces of the intestine, oriented perpendicular to the long axis of the bowel.
Although its origin can vary, the middle colic artery usually comes off the SMA as its second major branch. It travels anteriorly and divides into right and left branches, the former connecting with the ascending branch of the right colic and the left branch anastomosing with the ascending branch of the left colic. The middle colic can be followed during embolectomy to locate the SMA, by lifting the transverse colon and tracing the middle colic artery to the root of the mesentery where it originates off the SMA.