Meninges: Diagnosis
SURGICAL/CLINICAL CONSIDERATIONS
Goal of Consultation
Diagnosis of meningeal mass or other process
Provisional diagnosis aids in allocation of tissue for ancillary studies (molecular)
Change in Patient Management
Diagnosis of meningioma could result in complete resection for definitive treatment
Dependent on location of tumor and involvement of other structures (dural sinuses, bone)
Occasionally, dural margins may be sent for adequacy of excision
Other types of lesions will generally not undergo resection (metastasis, lymphoma, infectious or inflammatory process)
SPECIMEN EVALUATION
Gross
Nodular, plaque-like, or fragmented appearance, ± dural attachments
May be calcified or gritty in texture
Frozen Section
Initial specimen is often a small biopsy, which can be used for cytologic preparations and remainder frozen
If larger resection specimen is received, representative area can be frozen
Cytologic preparations are sometimes better for evaluation of meningiomas
If specimen is very fibrous and paucicellular on cytologic preparations, frozen section can be helpful
Cytology
May be difficult to smear
Touch preparations best for calcified lesions
Scrape preparations useful for fibrous lesions
Important adjunct to diagnosis of
Lymphoproliferative lesions
Bony or fibrous lesions difficult to cut (touch preparations helpful)
Cysts, as lining cells may be better preserved
May spare contamination of cryostat in cases suspected to be infectious
MOST COMMON DIAGNOSES
Meningioma and Variants
Meningioma, WHO grade I
Fibrous, meningothelial, transitional, psammomatous, secretory, angiomatous, microcystic subtypes
Meningothelial whorls, psammoma bodies may come off on touch prep
Syncytial groupings of cells with broad, flat, eosinophilic cytoplasm, nuclei with fine dusty chromatin, and smooth nuclear borders
Not necessary to distinguish among subtypes at intraoperative consultation
Atypical meningioma, WHO grade II
Frozen section or smear
Requires 4 mitoses/10 high-power fields or 3 of the following
Sheet-like growth (disordered architecture), small cell change, prominent nucleoli, hypercellularity, necrosis (in absence of embolization)
Or chordoid or clear cell morphology
Not necessary to distinguish grade at intraoperative consultation
Report as “meningioma with atypical features, grading deferred”
Anaplastic meningioma, WHO grade III
Frozen section or smear
≥ 20 mitoses/10 high-power fields
Or atypia in excess of that seen in grade II (resembling carcinoma, melanoma, or sarcoma)
Or rhabdoid or papillary features in most of tumor
Not necessary to define grade at intraoperative consultation
Report as “meningioma with atypical features, grading deferred” or “malignant neoplasm, type to be determined”
Solitary Fibrous Tumor
Identical to those arising in pleural or other soft tissue sites
Often called “hemangiopericytoma” in older neuropathologic literature
Frozen and smear
Epithelioid or spindle cells with intervening wire-like collagen
Staghorn vessels
Mitotic activity variable (> 4 mitoses/high-power field indicates “atypical solitary fibrous tumor”)
This tumor will usually undergo resection
Distinction from meningioma on frozen section is not critical for intraoperative management
Metastatic Carcinoma or Lymphoma
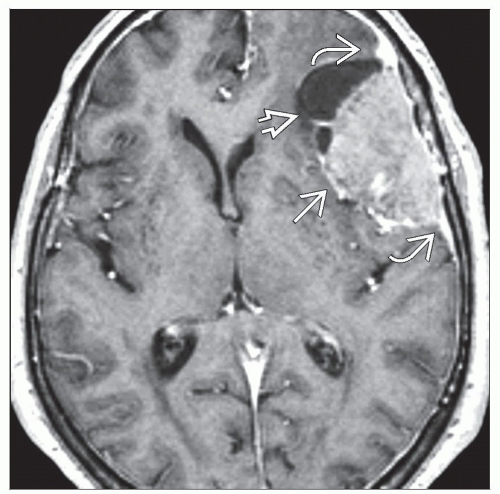
Single deposit may mimic meningioma
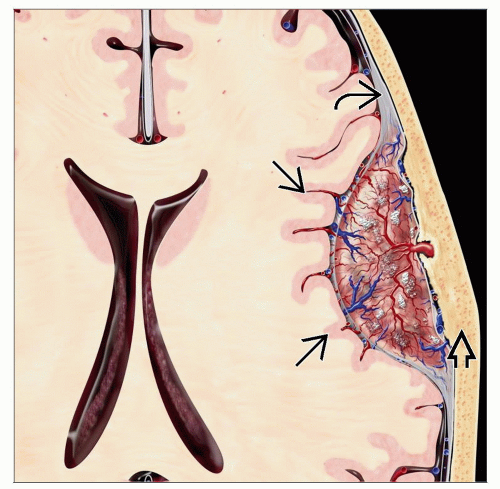
Leptomeningeal carcinomatosis or diffuse involvement by lymphoma has widespread enhancement on MR
Frozen and smear
Features of primary origin
Cytoplasmic clearing or vacuoles, glands indicate adenocarcinoma
Small cell vs. non-small cell for metastatic lung
Single-file cells for lobular breast carcinoma
Dyscohesive atypical lymphoid cells for lymphoma
History of prior malignancy is critically important for correct interpretation
Hemangioblastoma
Dural-based nodule in posterior fossa or spinal cord
Frozen section and smear
Multivacuolated cells (oil red O positive) amid fine capillary stroma
Often striking nuclear atypia without mitoses
Microcystic changes
Infection/Inflammatory Lesions
Pachymeningitis (inflammation of the dura mater) may have infectious or autoimmune cause
Tuberculosis (in developing world)
Smear and frozen: Typical necrotizing granulomas with giant cells
Idiopathic hypertrophic pachymeningitis is usually autoimmune
Smear and frozen: Abundant lymphoplasmacytic infiltrates, collagen deposition
Sarcoidosis
Hard granulomas with giant cells
In leptomeninges, almost always infectious cause, although paraneoplastic process is in differential
Bacterial
Neutrophilic exudates in acute bacterial meningitis
Lymphocytes and giant cells in tuberculous meningitis
Fungal
Mononuclear or mixed inflammatory infiltrates
Organisms (Cryptococcus, Coccidioides, rarely, Aspergillus or Candida) detectable on smear and frozen
Viral
Mononuclear infiltrates
In herpes encephalitis, biopsy may include involved brain, showing macrophages and necrosis
Viral cytopathic effect rarely visible
Material should be sent for specific cultures
Cysts
Infrequently sent for intraoperative consultation, as imaging and gross appearance to surgeon are sufficient for diagnosis
Lining cells may be scarce, relative to contents
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree