Medical Microbiology and Immunology
Steven D. Mahlen
Elmer W. Koneman
Christopher J. Papasian
Rangaraj Selvarangan
▪ Questions and Answers
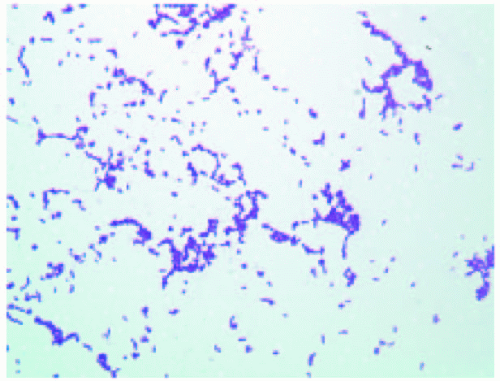
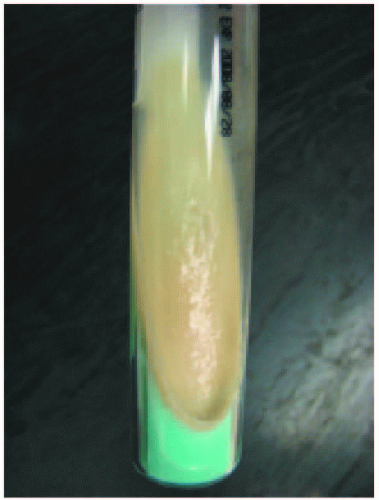
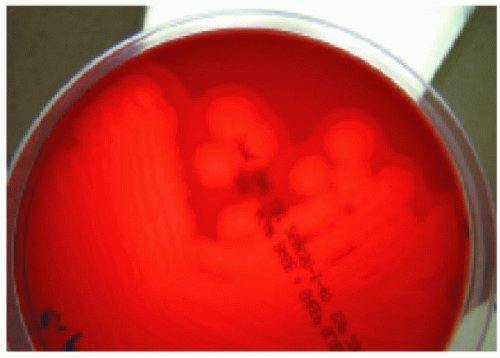
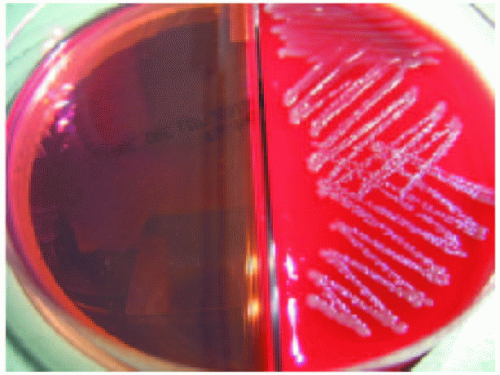
1. A 2-week-old neonate was brought to the emergency department with probable meningitis. A lumbar puncture was performed, with the following cerebrospinal fluid (CSF) labs: normal glucose, high protein, and pleocytosis with neutrophilic predominance. No organisms were observed on a Gram stain of the CSF. On culture the following day, however, there were many regular, short, non-spore-forming Gram-positive rods on both sheep blood agar and chocolate agar. The organisms were softly beta-hemolytic on blood agar and catalase positive. A Gram stain of the organism from a colony is shown in Figure 14.1. What is the likely identification of this isolate?
a. Streptococcus agalactiae
b. Erysipelothrix rhusiopathiae
c. Listeria monocytogenes
d. Corynebacterium jeikeium
e. Bacillus cereus
View Answer
1. c. Listeria monocytogenes is an important cause of meningitis in neonates. Neonatal infection caused by L. monocytogenes is similar to that caused by Streptococcus agalactiae (group B streptococcus). Both organisms cause an early-onset sepsis syndrome usually acquired in utero, and late-onset meningitis that occurs a few weeks after birth. S. agalactiae is catalase negative and is a Gram-positive coccus. Erysipelothrix rhusiopathiae is catalase negative and usually causes cutaneous infections or endocarditis in individuals who have had exposure to animals or animal products. Corynebacterium jeikeium is a pleomorphic Gram-positive rod that is nonhemolytic on blood agar and most often causes infections such as septicemia and wound infections in immunocompromised patients. Bacillus cereus is a spore-forming Gram-positive rod that can cause a variety of infections, including food poisoning and serious eye infections. L. monocytogenes is a catalase positive, beta-hemolytic Gram-positive rod that also exhibits the following characteristics: motile only at 25°C, forms a block-type CAMP test pattern, hippurate hydrolysis positive, and H2S negative.
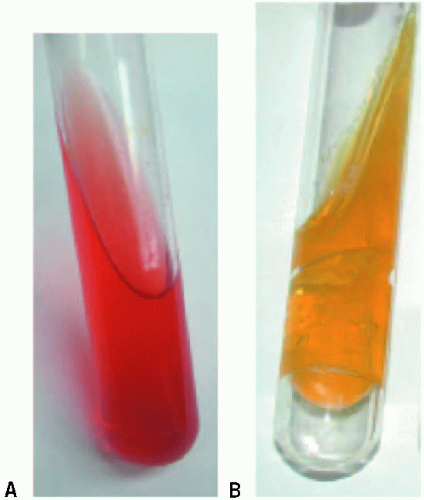
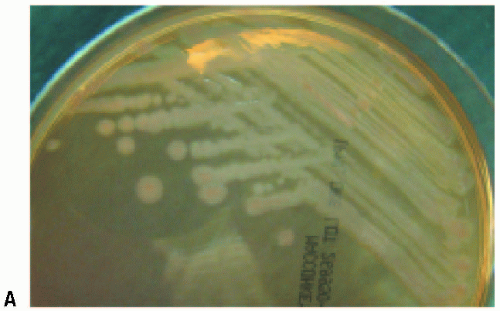
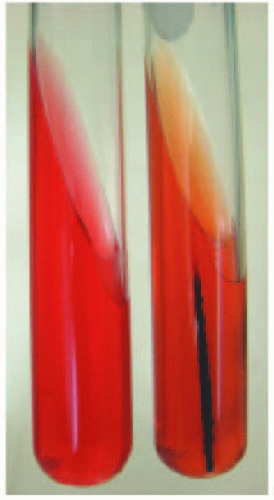
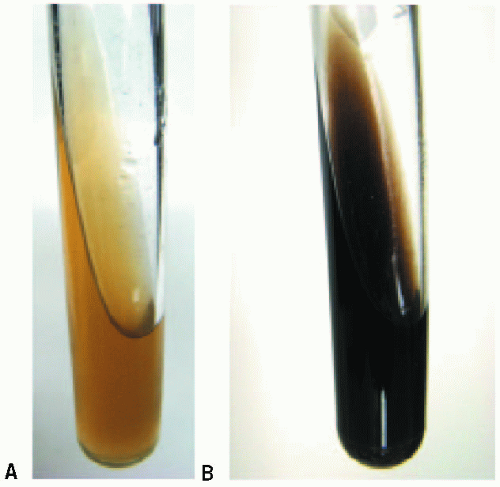
2. An uninoculated triple sugar iron (TSI) agar slant is shown in Figure 14.2A. What is the most appropriate description of the inoculated TSI agar slant shown in Figure 14.2B?
a. Sugar(s) utilized: glucose only; H2S production: negative; gas production: positive
b. Sugar(s) utilized: glucose, lactose, and/or sucrose; H2S production: negative; gas production: positive
c. Sugar(s) utilized: glucose, lactose, and/or sucrose; H2S production: positive; gas production: positive
d. Sugar(s) utilized: glucose and lactose only; H2S production: negative; gas production: positive
e. Sugar(s) utilized: glucose and sucrose only; H2S production: negative; gas production: positive
View Answer
2. b. The TSI agar slant is used to show whether gram-negative bacteria can ferment glucose, lactose, and/or sucrose, form gas, and form H2S. The ingredients of TSI agar include: the carbohydrates glucose, lactose, and sucrose, peptones, the pH indicator phenol red, sodium thiosulfate for H2S production, and ferrous sulfate to detect H2S. The concentration of lactose and sucrose is ten times higher than the concentration of glucose. If glucose is the only sugar fermented, acid is produced throughout the medium and initially the whole agar slant is yellow (phenol red turns yellow in the presence of acid). However, because the glucose concentration is so low, the organism will then utilize the peptones present in the medium and release basic products. Peptone utilization occurs aerobically, so the slant reverts to a red color; the butt of the medium remains yellow. This fermentation pattern is called K/A. If lactose or sucrose is fermented in addition to glucose, acid conditions are maintained throughout the medium because of the high concentrations of lactose and sucrose, so the pattern is A/A. If H2S is produced by the organism in question, the butt will turn black. H2S is only produced in an acid environment S, if the butt is black, it is assumed to be “A” for acid production. If gas is produced, gas bubbles will be observed in the butt of the tube.
3. A male patient from southeast India presents with large, painless ulcerative genital lesions and a beefy red penile lesion that has not healed in 6 months. A Wrights stain of a biopsy specimen reveals bipolarstaining rods in macrophages. Bacterial cultures of the biopsy specimen are negative. What is the likely causative agent of these lesions?
a. Haemophilus ducreyi
b. Chlamydia trachomatis
c. Treponema pallidum
d. Klebsiella granulomatis
e. Neisseria gonorrhoeae
View Answer
3. d. Klebsiella (formerly Calymmatobacterium) granulomatis is the causative agent of granuloma inguinale, or Donovanosis. This disease is most likely a sexually transmitted disease, characterized by painless ulcerative genital lesions. The primary lesion often becomes a beefy red granulomatous ulcer. The disease is rare in the United States but is more prevalent in southeast India, Papua New Guinea, the Caribbean, Brazil, parts of Africa, southeast Asia, and among Aboriginals in Australia. The organism does not grow on culture media, and is usually diagnosed by observing Donovan bodies (bipolar-stained rods) in macrophages or mononuclear cells. Haemophilus ducreyi causes chancroid, and can be cultured on solid media. Neisseria gonorrhoeae, a cause of urethritis, disseminated infections, and several other diseases, can also be cultured on solid media. Chlamydia trachomatis causes chlamydia and is usually diagnosed by cell culture in McCoy cells or by probe hybridization assays. Treponema pallidum is the causative agent of syphilis and does not grow on solid media. It is a spirochete, and is usually diagnosed by nontreponemal and treponemal tests.
4. Which of the following rapid tests best differentiates members of the genus Staphylococcus from members of the genus Streptococcus?
a. Catalase
b. Oxidase
c. Indole
d. Coagulase
e. Pyrase
View Answer
4. a. Staphylococci are catalase positive, while streptococci are catalase negative. Catalase is a test that can be performed in a few seconds to rapidly differentiate these two genera. The test consists of adding a drop of 3% hydrogen peroxide to colony material. If bubbling is observed, the test is considered positive.
5. Methicillin resistance in staphylococci:
a. is encoded by mecA
b. is best detected by disc diffusion by using a cefoxitin disc
c. means that all β-lactam antibiotics cannot be used for therapy
d. is enabled by an alteration in the target of β-lactam antibiotics
e. all of the above
View Answer
5. e. Methicillin resistance in staphylococci is encoded by mecA. Methicillin resistant organisms are resistant in vivo to all β-lactam antibiotics. The target of β-lactam antibiotics are the penicillin-binding proteins (PBPs) found in the cell wall of bacteria. The product of mecA is an altered PBP called PBP2′ or PBP2a. β-lactam antibiotics do not bind well, so they are ineffective. There are a number of ways to detect methicillin resistance. The polymerase chain reaction can be used to directly detect mecA from either colony material or directly from specimens. Many laboratories, though, use disk diffusion to determine susceptibilities, and cefoxitin has been found to be the most sensitive indicator of methicillin resistance by this method.
6. How is Chlamydia trachomatis typically cultivated?
a. On standard bacteriologic culture media, such as sheep blood agar
b. In MRC-5 cells
c. Coculture of infected peripheral blood mononuclear cells (PBMCs) with activated, allogeneic, noninfected PBMCs
d. In McCoy cells
e. In LLC-MK2 cells
View Answer
6. d. The most common method to cultivate Chlamydia trachomatis, an obligate intracellular pathogen, is cell culture in McCoy cells. McCoy cells, which are primarily used only to isolate C. trachomatis, are derived from a mouse fibroblast cell line. Other cell lines have also been used to cultivate C. trachomatis, including HeLa 229, HEp-2, HL, BGMK, Vero, and L cells. C. trachomatis cannot be cultivated on bacteriologic culture media. MRC-5 cells are used to cultivate many different viruses, including herpes simplex virus, CMV, and VZV. Coculture of infected peripheral blood mononuclear cells (PBMCs) with activated, allogeneic, noninfected PBMCs is used for HIV, HTLV-1/2, and other viruses. LLC-MK2 cells are used for several viruses, including mumps, parainfluenza, and several types of enterovirus.
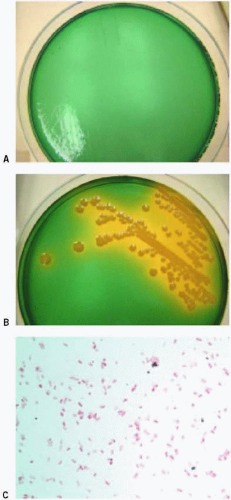
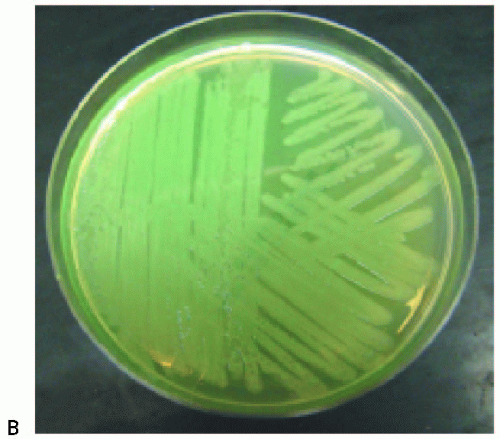
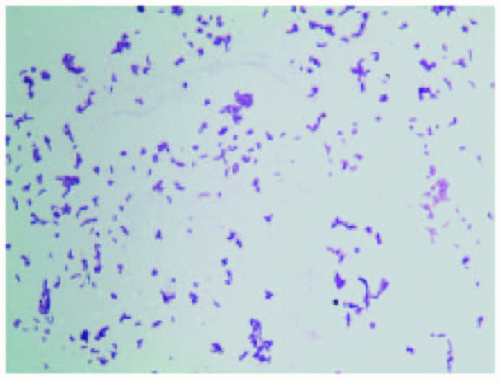
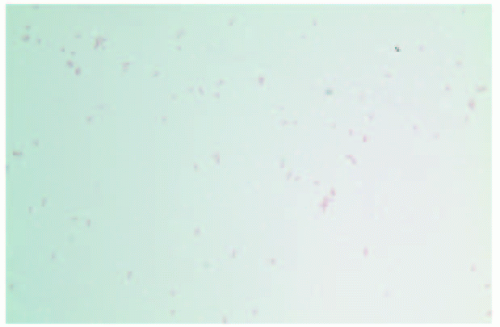
7. An oxidase-positive, curved gram-negative rod is isolated on thiosulfate citrate bile salts sucrose (TCBS) agar from a patient with gastroenteritis. The patient had eaten improperly cooked seafood. The isolate is shown in Figure 14.3B on TCBS agar, and an uninoculated TCBS agar plate is shown in Figure 14.3A. A Gram stain of the organism from a colony is shown in Figure 14.3C. What is the most likely identification of the isolate?
a. Campylobacter jejuni
b. Plesiomonas shigelloides
c. Vibrio cholerae
d. Vibrio parahaemolyticus
e. Shigella dysenteriae
View Answer
7. c. Thiosulfate citrate bile salts sucrose (TCBS) agar is a selective medium that is commonly used for isolating Vibrio species. TCBS agar usually inhibits other bacteria besides Vibrio species. The medium differentiates sucrose-fermenting species, such as V. cholerae, from non-sucrose-fermenting species. When sucrose is fermented, yellow colonies and a yellow precipitate are observed (Fig. 14.3B; compare to uninoculated TCBS plate, Fig. 14.3A). Besides V. cholerae, sucrose-fermenting species include V. alginolyticus, V. metschnikovii, a few strains of V. vulnificus, and other species. Nonsucrose-fermenting species include V. mimicus, V. parahaemolyticus, most strains of V. vulnificus, V. damsela, and other species.
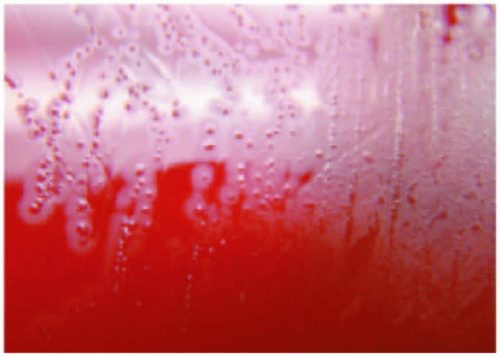
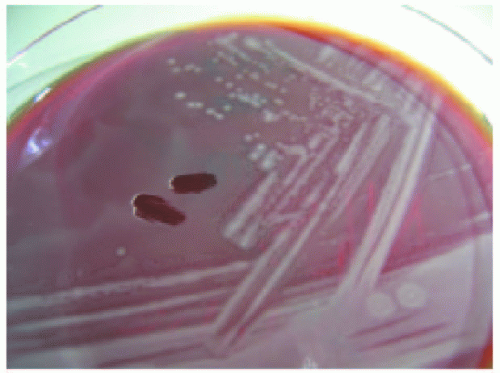
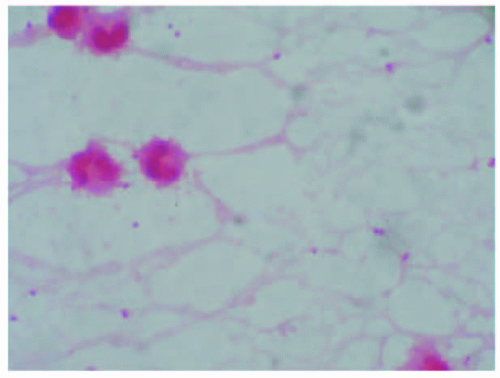
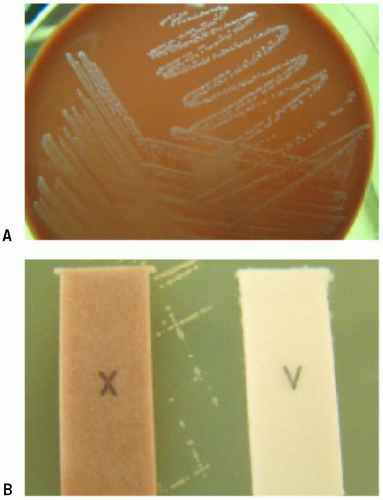
8. A patient is seen in the emergency department with a wound infection on his right hand. He had been in a fight a few days ago and suffered a clenched fist injury on the same hand when he struck someone else in the face. A wound culture is submitted to the laboratory, and small, Gram-negative coccobacilli are observed on both sheep blood agar and chocolate agar after 48 hours. The colonies are small, pit the agar, and smell like bleach; colonies are shown on sheep blood agar in Figure 14.4. The isolate is oxidase positive, indole negative, and did not grow on
MacConkey agar. What is the likely identity of the isolate?
MacConkey agar. What is the likely identity of the isolate?
a. Eikenella corrodens
b. Cardiobacterium hominis
c. Pasteurella multocida
d. Pseudomonas aeruginosa
e. Haemophilus influenzae
View Answer
8. a. Eikenella corrodens is an inhabitant of the human oral cavity and the gastrointestinal tract. It is associated with human bite wounds, clenched fist injuries, oral surgery, and cellulitis among drug addicts when they lick needles before injection. It also causes endocarditis, and is part of the “HACEK” group of bacteria. E. corrodens isolates are well known for their strong bleachlike odor and the fact that colonies may pit the agar (Fig. 14.4). Cardiobacterium hominis, another member of the HACEK group, may also pit the agar, but it is indole positive and does not smell like bleach. Pasteurella multocida is usually associated with animal bite wounds. Haemophilus influenzae usually does not grow on sheep blood agar, and requires X and V factors. Pseudomonas aeruginosa grows well on MacConkey agar, and colonies are readily apparent in 24 hours.
9. Based on the sputum Gram stain from a patient with pneumonia shown in Figure 14.5, which of the following genera most likely would NOT be in the differential?
a. Mycobacterium
b. Gordonia
c. Nocardia
d. Arcanobacterium
e. Tsukamurella
View Answer
9. d. The Gram stain depicts a beaded, branching, Grampositive rod, which was later found to be a Nocardia species. Generally, bacteria with high lipid contents in their cell walls, such as organisms from the genera Mycobacterium, Nocardia, Gordonia, and Tsukamurella, do not stain completely with the Gram stain, and often appear beaded. Any time a beaded, branching organism is observed in a direct clinical Gram stain, one of these genera should be suspected (Mycobacterium species may appear beaded, but may not show branching). All of these genera could also cause pulmonary disease. Arcanobacterium species could also cause pulmonary diseases, but they stain as Gram-positive rods, and do not appear beaded.
10. Mutations in which of the following gene products may be responsible for fluoroquinolone resistance in bacteria?
a. Penicillin-binding protein 2
b. DNA gyrase
c. Dihydrofolate reductase
d. DNA polymerase
e. RNA polymerase
View Answer
10. b. Resistance to fluoroquinolones in bacteria can arise from mutations in DNA gyrase, an enzyme that relaxes supercoiled DNA during DNA replication. Resistance to fluoroquinolones can also be caused by outer membrane mutations that result in a diminished uptake of the antibiotic, or by activation of an efflux pump that removes the antibiotic from the cytoplasm of the organism.
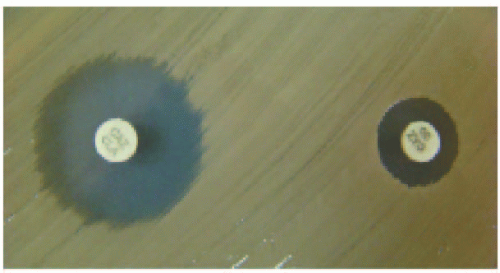
11. An anaerobic, pale-staining, pleomorphic Gram-negative rod is isolated from a patient with an intra-abdominal abscess. Growth of the isolate in the presence of kanamycin (K disk), colistin (Cl disk), and vancomycin (Va disk), and 20% bile (no marking) is shown in Figure 14.6. What is the most likely identity of the isolate?
a. Fusobacterium nucleatum subsp. nucleatum
b. Bacteroides fragilis
c. Prevotella bivia
d. Fusobacterium necrophorum subsp. necrophorum
e. Bilophila wadsworthia
View Answer
11. b. Bacteroides fragilis is the most common anaerobe isolated from infections involving anaerobic bacteria. B. fragilis is isolated frequently from many types of infections, including intra-abdominal infections, pleuropulmonary infections, pelvic infections, skin and soft tissue infections, and bacteremia. It grows in the presence of 20% bile, and is usually resistant to kanamycin, colistin, and vancomycin (Fig. 14.6). Most other anaerobic Gram-negative rods will not grow in the presence of 20% bile, except Bilophia wordsworthia and Fusobacterium mortiferum–varium. B. wordsworthia and the commonly isolated Fusobacterium species can be differentiated from B. fragilis by their sensitivity to kanamycin and colistin.
12. A faintly staining Gram-negative rod was isolated on buffered charcoal yeast extract (BCYE) agar from a patient with community-acquired pneumonia. The colonies were white in color, as shown in Figure 14.7, and took 4 days to grow. The isolate was biochemically inert. A direct Gram stain of sputum from the patient revealed 3+ white blood cells and no bacteria.
Based on this information, what is the likely identify of this isolate?
Based on this information, what is the likely identify of this isolate?
a. Pseudomonas aeruginosa
b. Bordetella pertussis
c. Legionella pneumophila
d. Stenotrophomonas maltophilia
e. Burkholderia pseudomallei
View Answer
12. c. Legionella pneumophila is a thin, poorly staining Gram-negative rod that primarily causes pneumonia but may also be involved in extrapulmonary infections. It is frequently not observed on direct Gram stains from patient sputum. The medium of choice to culture L. pneumophila and other Legionella species is BCYE agar. Colonies are often white to bluish white in color, and isolates are biochemically nonreactive. Many laboratories use 16S rRNA gene sequencing to definitively identify Legionella species. Pseudomonas aeruginosa, Stenotrophomonas maltophilia, and Burkholderia pseudomallei all grow well on standard bacteriology media in about 24 hours or less, and react to several biochemicals. Bordetella pertussis is usually cultured on Regan-Lowe agar or Bordet-Gengou agar, and colonies resemble mercury drops.
13. A catalase-positive, coagulase-negative Gram-positive coccus is isolated from a clean catch urine sample from a female with symptoms of a urinary tract infection. The isolate is PYR test negative and resistant to novobiocin. The organism is shown on sheep blood agar in Figure 14.8. What is the most likely identity of the isolate given the list below?
a. Enterococcus faecalis
b. Staphylococcus aureus
c. Staphylococcus epidermidis
d. Staphylococcus saprophyticus
e. Streptococcus agalactiae
View Answer
13. d. Staphylococcus saprophyticus is a relatively infrequent cause of urinary tract infection (UTI), but nearly all women are symptomatic when the organism is cultured from their urine. It is the most frequent coagulase-negative staphylococcus isolated from UTIs. S. epidermidis, another coagulase-negative staphylococcus, is isolated from urine infrequently, but about 90% of patients are asymptomatic when the organism is cultured. S. saprophyticus is resistant to novobiocin, while S. epidermidis is sensitive. S. aureus is coagulase positive, while both Enterococcus faecalis and Streptococcus agalactiae are catalase negative.
14. Which of the following statements about the Venereal Disease Research Laboratory (VDRL) test is correct?
a. It is a serologic assay designed to detect treponemal antibodies.
b. It is the confirmatory assay for a positive rapid plasma reagin (RPR) test.
c. It has the highest sensitivity for primary syphilis.
d. It is a nontreponemal assay that requires microscopic examination.
e. All of the above are correct statements.
View Answer
14. d. The VDRL test is a nontreponemal serologic assay that detects reaginic antibodies that flocculate with cardiolipin for measuring a host response to Treponema pallidum, the organism that causes syphilis. The VDRL test is read with a microscope. The RPR test is another example of a nontreponemal assay; this test can be read by eye. The nontreponemal assays are usually used as screening assays. They lack sensitivity for primary and late syphilis, however. Positive nontreponemal tests are confirmed with specific treponemal serologic assays such as the FTA-ABS (fluorescent treponemal antibody absorption) test or the TP-PA (T. pallidum particle agglutination) test.
15. An acid-fast bacillus is observed in a tissue specimen from a patient with a postoperative leg wound infection. The organism grows in 4 days on a Lowenstein-Jensen agar slant and colonies are buff colored in both light and dark conditions (Fig. 14.9). This growth pattern is most typical of which of the following organisms?
a. Mycobacterium marinum
b. Mycobacterium chelonae
c. Mycobacterium gordonae
d. Mycobacterium ulcerans
e. Mycobacterium kansasii
View Answer
15. b. Mycobacterium chelonae is one of the rapid-growing mycobacteria, and it is usually nonpigmented. Rapid-growing mycobacteria are those in which colonies appear in less than 7 days on solid media. The slow-growing mycobacteria take longer than 7 days to form colonies on solid media. Both M. kansasii and M. marinum are slow growers that are further classified as photochromogens—that is, their colonies become pigmented when exposed to light. M. gordonae is usually thought of as a nonpathogen, and is a slow grower classified as a scotochromogen. Scotochromogen colonies are pigmented in both light and dark conditions. Last, M. ulcerans is a nonphotochromogen (is not pigmented in either the light or the dark) that is also a slow grower.
16. A young man develops a macular skin rash on his abdomen and chest a few days after sitting in a hot tub. A culture of one of the lesions reveals thin gram- negative rods. The isolate grows readily on standard bacteriologic media, is oxidase positive, motile, non fermentative, and grows at 42°C. Figure 14.10A shows the isolate on MacConkey agar and Figure 14.10B shows the isolate on Mueller-Hinton agar. What is the likely identity of the isolate?
a. Stenotrophomonas maltophilia
b. Acinetobacter baumanii
c. Pseudomonas aeruginosa
d. Escherichia coli
View Answer
16. c. The patient has Pseudomonas dermatitis, which is often acquired from whirlpools, hot tubs, etc. P. aeruginosa is readily identified as an oxidase-positive, nonfermentative (Fig. 14.10A), motile gram-negative rod that grows well at 42°C. In addition, it produces the bluish green pigment pyocyanin (Fig. 14.10B), and may form other pigments as well. P. fluorescens has rarely been implicated in disease, and, like most Pseudomonas species except P. aeruginosa, does not grow at 42°C. Escherichia coli is a fermenter and is oxidase negative. Both Stenotrophomonas maltophilia and Acinetobacter baumannii are oxidase negative; S. maltophilia is motile while A. baumannii is not.
17. On which of the following media does Gardnerella vaginalis produce β-hemolytic colonies?
a. Human blood bilayer Tween (HBT) agar
b. Trypticase soy agar with 5% sheep blood
c. Cystine-tellurite blood agar
d. Columbia colistin-nalidixic acid (CNA) agar with 5% sheep blood
e. All of the above
View Answer
17. a. Gardnerella vaginalis, which may be involved in bacterial vaginosis, is a Gram-positive rod that often stains gram variable. Colonies of G. vaginalis are nonhemolytic on standard sheep blood agar and on CNA. However, on human blood bilayer Tween (HBT) agar, G. vaginalis produces softly β-hemolytic colonies, and is usually the medium of choice for this organism.
18. Figure 14.11 shows an organism isolated on sheep blood agar from a clean catch urine specimen from a young woman with a suspected urinary tract infection. A portion of the organism is scraped off of the agar plate to illustrate the growth of the organism. A Gram stain of the organism reveals short Gram-negative rods that stain thicker on both ends of the cells. The isolate is oxidase negative and indole positive. What is the likely identification of the isolate?
a. Escherichia coli
b. Proteus mirabilis
d. Proteus vulgaris
e. Klebsiella pneumoniae
View Answer
18. d. The urinary tract isolate is exhibiting swarming on sheep blood agar, a characteristic that is common for Proteus species. The two most commonly isolated Proteus species, P. mirabilis and P. vulgaris, can be differentiated by the indole test. P. vulgaris is indole positive, while P. mirabilis is indole negative. Escherichia coli and Klebsiella oxytoca are also indole positive but do not swarm. K. pneumoniae is indole negative and does not swarm. Proteus swarming is best observed on sheep blood agar or on chocolate agar. Swarming is not observed on MacConkey agar, due to a higher percentage of agar in the medium.
19. Which of the following is NOT a characteristic of Bacillus anthracis?
a. Nonmotile
b. Nonhemolytic on sheep blood agar
c. Catalase positive
d. Spores are present.
e. Motile
View Answer
19. e. All Bacillus species are catalase-positive, spore-forming Gram-positive rods. B. anthracis, one of the most important human pathogens and a potential bioterrorism agent, is recognized by its lack of motility and hemolysis. Any spore-forming Gram-positive rod that is nonmotile and nonhemolytic should be referred to the appropriate public health agency to rule out B. anthracis.
20. A young boy is bitten by his pet rat and within a few days develops fever, chills, vomiting, and severe joint pains. A rash soon develops on his palms and soles. Gram-negative rods are isolated from the blood in broth media without the supplement sodium polyanethol sulfonate (SPS). The rods are extremely pleomorphic and filamentous, and are oxidase- and catalase negative. What is the likely identity of the isolate?
a. Pasteurella multocida
b. Leptospira interrogans
c. Eikenella corrodens
d. Streptobacillus moniliformis
e. Cardiobacterium hominis
View Answer
20. d. Streptobacillus moniliformis is the agent of rat bite fever. The organism is naturally found in the upper respiratory tract of wild, laboratory, and pet rats. Humans can get infected by S. moniliformis by bites, or by ingesting contaminated food, milk, or water. When the organism is acquired by ingestion, the disease is called Haverhill fever. S. moniliformis is a Gram-negative rod that is very pleomorphic and often forms long filaments. The organism is inhibited by sodium polyanethol sulfonate (SPS), a supplement that is found in most blood culture media. Thus, if S. moniliformis is suspected, media without SPS must be used for isolation. In general, it is a nonreactive bacterium for most commonly used biochemical tests. Pasteurella multocida, Eikenella corrodens, and Cardiobacterium hominis are all oxidase positive, and will all grow in standard blood culture media. Leptospira interrogans is a spirochete. A similar disease to rat-bite fever called sodoku is caused by the spirochete Spirillum minus. sodoku is also spread by rat bites, but occurs most often in Asia.
21. A week after he removed an embedded tick, a 38-year-old male hunter from Arkansas presents with a fever, chills, myalgia, malaise, an intense headache, nausea, and vomiting. No rash is present. The patient is thrombocytopenic (18,000 platelets/µL), has mildly elevated liver function tests, and is mildly leukopenic (neutropenia). Intracellular inclusions are observed in monocytes in a buffy coat preparation from a peripheral blood smear. What is the likely identity of this organism?
a. Ehrlichia chaffeensis
b. Anaplasma phagocytophilum
c. Rickettsia rickettsii
d. Orientia tsutsugamushi
e. Rickettsia typhi
View Answer
21. a. Ehrlichia chaffeensis is an obligate intracellular pathogen that tends to infect monocytes and macrophages. It is the causative agent of human monocytotropic ehrlichiosis (HME). The organisms can be observed in cytoplasmic inclusions in monocytes and macrophages called morulae, although it is rare to find them. The clinical manifestations are similar to Rocky Mountain spotted fever (RMSF) caused by Rickettsia rickettsii; however, approximately 90% of patients with RMSF will have a rash, while a rash is present in <50% of cases of HME. In addition, morulae are not observed in patients with RMSF. Anaplasma phagocytophilum is the agent of human granulocytotropic anaplasmosis (HGA), and also causes a similar disease. A. phagocytophilum tends to infect neutrophils, not monocytes, and can be observed as morulae as well. The agents of HME, HGA, and RMSF are all transmitted by the bites of ticks. Orientia tsutsugamushi, the agent of scrub typhus, is transmitted by chigger bites, and is not endemic in the United States. Rickettsia typhi is the agent of murine typhus, and is transmitted by flea bites. It does occur in the United States. Diagnosis of many of these intracellular pathogens is usually made by epidemiology factors, clinical manifestations, and serology.
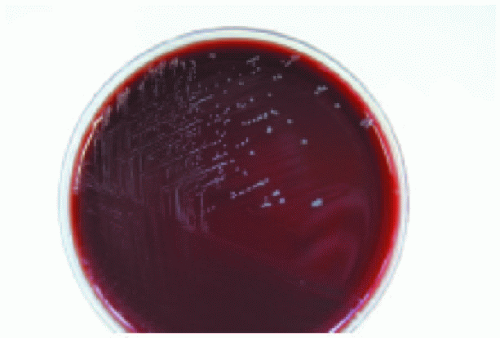
22. The isolate shown on the sheep blood agar plate in Figure 14.12 grew only in an anaerobic atmosphere and
stained as large, boxcar-shaped Gram-positive rods. No spores were present on the Gram stain. The isolate is from a case of myonecrosis. What is the most likely identification of this isolate?
stained as large, boxcar-shaped Gram-positive rods. No spores were present on the Gram stain. The isolate is from a case of myonecrosis. What is the most likely identification of this isolate?
a. Clostridium tetani
b. Clostridium botulinum
c. Bacillus cereus
d. Clostridium perfringens
e. Bacillus anthracis
View Answer
22. d. Clostridium perfringens is the most frequent clostridial species isolated from clinical specimens. It is well known as an agent of food poisoning, gas gangrene (myonecrosis), pulmonary infections, and soft tissue infections. C. perfringens characteristically produces a double zone of hemolysis on blood agar, as illustrated in Figure 14.12. A Gram stain of C. perfringens typically shows large, boxcar-shaped Gram-positive rods that may stain gram variable. While all clostridia form endospores, they are rarely observed in C. perfringens isolates. Bacillus cereus and B. anthracis will grow in both aerobic and anaerobic atmospheres. C. tetani and C. botulinum are not beta-hemolytic on sheep blood agar.
23. A patient has an oral abscess drained. A yellow, grainy substance resembling sulfur granules is expressed from the abscess. A Gram stain of the material reveals pleomorphic Gram-positive rods that have rudimentary branches, as shown in Figure 14.13. The organisms were modified acid-fast stain negative, grew better in an anaerobic atmosphere than in aerobic conditions, and were catalase negative. What is the likely identification of the isolate?
a. Corynebacterium jeikeium
b. Actinomyces israelii
c. Nocardia farcinica
d. Nocardia asteroides
e. Corynebacterium xerosis
View Answer
23. b. Actinomyces israelii has been isolated from various oral infections, wound infections, and intrauterine-device-associated infections from the female genital tract. There are many Actinomyces species that have been implicated in human infections. While Actinomyces species are usually thought of as anaerobes, most will grow in aerobic conditions, although they tend to grow better anaerobically. The majority of Actinomyces species are catalase-negative, pleomorphic Gram-positive rods that may form rudimentary branches. They do not stain with the modified acid-fast stain, unlike Nocardia species. Nocardia species, which are often roughly classified as “aerobic actinomycetes,” grow best in aerobic conditions and are catalase positive. Corynebacterium species are also catalase positive, also tend to be aerobes, and do not stain with the modified acid-fast stain.
24. A 37-year-old woman presents to her physician with fever, chills, headache, and a nonproductive cough. Pharyngeal erythema is noted on examination. A chest x-ray reveals consolidation in her left lower lobe. Her history is significant in that she keeps budgerigars and parrots at home. Sputum is obtained, but no organisms are observed from a direct Gram stain and no growth occurs on artificial culture media. Given these results and the patient’s history, what is the most probable causative agent?
a. Legionella pneumophila
b. Streptococcus pneumoniae
c. Chlamydophila pneumoniae
d. Mycobacterium tuberculosis
e. Chlamydophila psittaci
View Answer
24. e.Most cases of psittacosis, caused by Chlamydophila psittaci, involve individuals who have had contact with birds. People at risk include poultry farmers, pet store employees, abattoir workers, veterinarians, and pet owners. The organism is usually spread to humans via the respiratory route. Psittacosis can take many forms, including a subclinical infection, a typhoidal manifestation, and an atypical pneumonia. Like other organisms in the family Chlamydiaceae, C. psittaci is an obligate intracellular pathogen with a unique biphasic life cycle; the organism does not stain with the Gram stain and will not grow on artificial bacteriologic media. The transmissible form of C. psittaci and other Chlamydiaceae is the elementary body that attaches to host cells. Elementary bodies are internalized after attachment and transform into reticulate bodies. The reticulate bodies replicate and form a cytoplasmic inclusion. The reticulate bodies then transform back into elementary bodies and are released from the host cell. Identification of C. psittaci is often made using serologic methods such as complement fixation or microimmunofluorescence, although cell culture and the polymerase chain reaction are useful also. Chlamydophila pneumoniae is a common cause of community-acquired pneumonia, but it is not normally associated with exposure to birds. Legionella pneumophila, Mycobacterium tuberculosis, and Streptococcus pneumoniae can all be cultured on artificial media.
25. A 3-year-old child is brought to the emergency department by his parents. The child has a fever, rash, and nuchal rigidity. A lumbar puncture is performed. The following results are obtained from the CSF: glucose <20, protein 244, slightly cloudy, and 98% polymorphonuclear cells. A gram stain reveals many white blood cells and many Gram-negative diplococci as shown in Figure 14.14. The following day, there were many colorless colonies on chocolate agar. The isolate was oxidase positive and catalase positive. In addition, it produced acid from glucose and maltose. What is the identity of the isolate?
a. Moraxella catarrhalis
b. Streptococcus pneumoniae
c. Haemophilus influenzae
d. Neisseria meningitidis
e. Neisseria gonorrhoeae
View Answer
25. d. The clinical presentation of the child is fairly typical of meningitis caused by Neisseria meningitidis. N. meningitidis is carried in the nasopharynx in about 15% to 20% of the population, and can cause bacteremia, meningoencephalitis, urethritis, and pneumonia in addition to meningitis. There are 13 serogroups, but most infections are caused by the A, B, C, Y, and W-135 serogroups. There is a vaccine for N. meningitidis that covers serogroups A, C, Y, and W-135. N. meningitidis is a Gram-negative diplococcus, like many members of the genus Neisseria. All Neisseria species are oxidase positive, and most are catalase positive. Neisseria species can be differentiated from each other by their ability to produce acid from the carbohydrates glucose, maltose, lactose, sucrose, and fructose. N. meningitidis produces acid from both glucose and maltose, while N. gonorrhoeae produces acid only from glucose. Moraxella catarrhalis is also an oxidase-positive, Gram-negative diplococcus, but it does not produce acid from carbohydrates. Nither N. gonorrhoeae nor M. catarrhalis would be expected to cause meningitis. Streptococcus pneumoniae is an agent of meningitis, but it is a Gram-positive, catalase-negative diplococcus. Haemophilus influenzae may also cause meningitis, but it is a Gram-negative coccobacillus or short rod and requires X and V factors for growth.
26. MacConkey-sorbitol agar is used to isolate:
a. Shigella species
b. Escherichia coli O157:H7
c. Non-O157:H7 Escherichia coli strains
d. Salmonella serotypes
e. Yersinia enterocolitica
View Answer
26. b. MacConkey agar with sorbitol (often referred to as SMAC) is both a selective and differential medium for O157 Shiga toxin-producing Escherichia coli strains. Sorbitol is the only carbohydrate in SMAC, instead of lactose, which is in standard MacConkey agar. There are many Shiga toxin-producing E. coli serotypes. All of the Shiga toxin-producing strains are capable of causing illness such as bloody diarrhea and hemolytic uremic syndrome (HUS). O157 strains account for about 80% of all cases of HUS in the United States. The O157 strains are unique among other E. coli strains (including non-O157 Shiga toxin-producing strains) in that they do not ferment sorbitol. E. coli O157 strains appear as colorless colonies on SMAC since they do not ferment sorbitol, while all other E. coli strains appear dark pink, since they ferment sorbitol. Yersinia enterocolitica and most Salmonella species/serotypes ferment sorbitol. About 30% to 40% of Shigella isolates ferment sorbitol, but media such as Hektoen enteric agar or xylose lysine deoxycholate (XLD) agar is usually used to isolate Salmonella and Shigella.
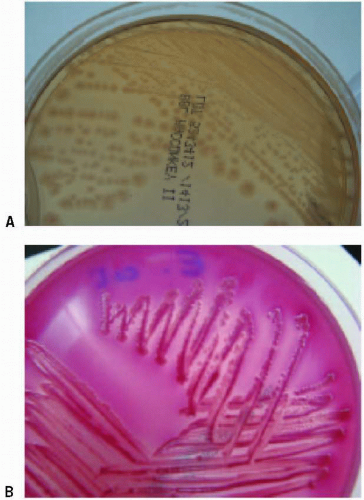
27. A Gram-negative coccobacillus is isolated on Bordet-Gengou agar (Fig. 14.15) from a 3-year-old child with a 1-week history of a mild cough and a runny nose. The child has received no immunizations. The isolate is oxidase positive, nonmotile, nitrate-reduction negative, and urease negative. In addition, it did not grow on either sheep blood agar or MacConkey agar. What is the likely identification of the isolate?
a. Bordetella bronchiseptica
b. Legionella pneumophila
c. Bordetella pertussis
d. Bordetella parapertussis
e. Brucella melitensis
View Answer
27. c. Bordet-Gengou agar is one example of a medium that is used to isolate the fastidious Gram-negative coccobacillus Bordetella pertussis, the agent of pertussis or whooping cough, from clinical specimens. Bordet-Gengou medium has a short shelf-life, so Regan-Lowe medium is used more often for the isolation of B. pertussis. B. parapertussis also may cause a pertussis-like respiratory syndrome; B. bronchiseptica has been associated with a few cases of respiratory diseases as well. Both of these organisms will grow on standard bacteriology media such as sheep blood agar and MacConkey agar, although recovery of B. parapertussis is enhanced by using Bordet-Gengou agar or Regan-Lowe agar. Both B. pertussis and B. bronchiseptica are oxidase positive, but B. parapertussis is oxidase negative. In addition, B. pertussis does not reduce nitrate, does not produce urease, and is nonmotile. B. parapertussis produces urease in 24 hours, and B. bronchiseptica usually produces urease in 4 hours or less. B. bronchiseptica also reduces nitrate and is motile; B. parapertussis is negative for both of these characteristics. Legionella pneumophila is an agent of pneumonia, but is usually cultured on buffered charcoal yeast extract (BCYE) agar, and is a very nonreactive organism biochemically. Brucella melitensis is one of the Brucella species that causes brucellosis, a zoonotic, systemic disease. It is oxidase positive and will usually grow on chocolate agar. In addition, B. melitensis reduces nitrate, is nonmotile, and is urease positive.
28. An individual eats fried rice from an Asian restaurant and within two hours is ill with vomiting and nausea. What is the most likely explanation for this individual’s illness?
a. The individual ingested food contaminated with enterohemorrhagic Escherichia coli.
b. The individual ingested food contaminated with Campylobacter jejuni.
c. The individual ingested food contaminated with preformed Bacillus cereus emetic toxin.
d. The individual ingested food contaminated with Salmonella species.
e. The individual ingested food contaminated with preformed Clostridium perfringens enterotoxin.
View Answer
28. c. The most likely explanation for the patient’s illness is ingestion of a preformed enterotoxin in the fried rice that he ate. One of the most rapid-acting enterotoxins is the Bacillus cereus emetic toxin. This toxin typically acts within 1-6 hours of ingestion and usually causes vomiting, nausea, and abdominal cramps. Some patients get diarrhea as well. Foods associated with B. cereus emetic toxin include fried rice and various meat products. B. cereus may also produce a diarrheal toxin that takes 10-16 hours before symptoms of diarrhea, vomiting, and abdominal cramps appear. Another very fast acting bacterial toxin is staphylococcal enterotoxin, produced by Staphylococcus aureus; this toxin, like the B. cereus emetic toxin, acts about 1-6 hours after ingestion. The Clostridium perfringens enterotoxin is also fast-acting, causing symptoms of watery diarrhea, abdominal cramps, nausea, and sometimes vomiting about 8-16 hours after ingestion. Salmonella species, Campylobacter jejuni, and enterohemorrhagic Escherichia coli all may cause gastroenteritis. All three organisms must be ingested to cause disease; disease caused by Salmonella and Campylobacter is not toxinrelated, but is instead associated with invasion. Nontyphoidal Salmonella strains usually cause symptoms of diarrhea, abdominal cramps, and nausea in 1-3 days after ingestion. C. jejuni and other Campylobacter species cause bloody diarrhea, fever, vomiting, and abdominal cramping 2-5 days after ingestion. Enterohemorrhagic E. coli strains, such as O157 isolates, produce the Shiga toxin. Symptoms are usually produced 1-8 days after ingestion and include bloody diarrhea, vomiting, and abdominal cramping.
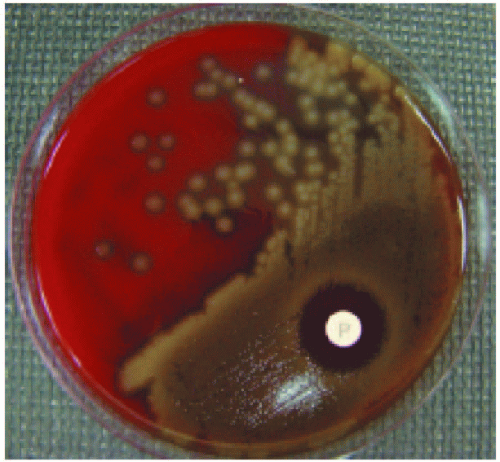
29. The organism shown in Figure 14.16 was isolated from the blood from a patient hospitalized with pneumonia. The organism is a lancet-shaped Gram-positive coccus in pairs and short chains, is catalase negative, and is bile sensitive. An optochin disk (P disk) was placed on the first quadrant of the sheep blood agar plate in Figure 14.16. Based on these results and the patient’s illness, what is the most likely identity of the isolate?
a. Viridans streptococci
b. Streptococcus pneumoniae
c. Streptococcus pyogenes
d. Streptococcus agalactiae
e. Enterococcus faecalis
View Answer
29. b. Streptococcus pneumoniae is classically alpha-hemolytic on sheep blood agar and sensitive to optochin (P disk) (Fig. 14.16). Streptococci are catalase negative, and S. pneumoniae often appears as lancet-shaped Gram-positive cocci in pairs or short chains. The gram stain reaction, alpha-hemolysis and optochin sensitivity are initial clues that an isolate is S. pneumoniae; many labs will perform a bile test to confirm the organism. S. pneumoniae is bile sensitive. In addition, S. pneumonia colonies often have a central depression, and may look “donut shaped,” and many isolates are also mucoid. The viridans group streptococci are also alpha-hemolytic, but usually appear as Gram-positive cocci in chains and are resistant to optochin as a group. Both S. pyogenes and S. agalactiae are beta-hemolytic on sheep blood agar, and both also appear as Grampositive cocci in chains. Enterococci such as E. faecalis may appear similar to S. pneumoniae on gram stain—that is, as lancet-shaped Gram-positive cocci in pairs and short chains—but they are usually nonhemolytic. S. pneumoniae is well known as an agent of community-acquired pneumonia, meningitis, otitis media, and other infections such as bacteremia, endocarditis, and sinusitis.
30. An Enterococcus faecium isolate is cultured from the blood of a patient with endocarditis. The isolate is vancomycin resistant. Which of the following is NOT true regarding this isolate?
a. Vancomycin resistance is due to an alteration of the target in enterococci.
b. E. faecium is naturally resistant to vancomycin.
c. E. faecium is part of the normal gastrointestinal flora of most humans.
d. E. faecium isolates are nearly always resistant to ampicillin and penicillin.
e. Vancomycin resistance is acquired by E. faecium isolates.
View Answer
30. b. Enterococci are catalase-negative Gram-positive cocci that often appear as pairs or short chains. Most of the enterococci hydrolyze esculin and grow in the presence of bile and 6.5% sodium chloride. Members of this genus are widespread in nature. In humans, they are usually found in the gastrointestinal tract. Enterococcus faecalis is probably the most prevalent of the enterococci found in the human gastrointestinal tract, followed by E. faecium and other species. Enterococci tend to cause opportunistic infections in immunocompromised patients, the elderly, and patients who have been hospitalized for long periods. Enterococci may cause urinary tract infections, wound infections, bacteremia, and endocarditis. E. faecalis is the most common of the enterococci isolated in clinical specimens, followed by E. faecium. An important problem now in hospitals is the emergence of vancomycin-resistant enterococci (VRE). E. faecalis and E. faecium acquire vancomycin-resistance. There are a number of vancomycin- resistance phenotypes, but the most common in E. faecalis and E. faecium are the VanA and VanB phenotypes, encoded by the vanA and vanB genes, respectively. Of the VRE strains that are isolated in the United States, most are E. faecium. Resistance caused by VanA and VanB is the result of an alteration of the cell wall target of vancomycin. Intrinsically, most enterococci are resistant to several antimicrobial agents, such as trimethoprim-sulfamethoxazole and low levels of aminoglycosides. In particular, most E. faecium isolates are intrinsically resistant to ampicillin and penicillin, making E. faecium a difficult organism to treat, especially if a given isolate is found to be a VRE.
31. A 47-year-old man from California presents to the Emergency Department with fever, headache, back pain, malaise, and hepatosplenomegaly. The patient revealed that he had consumed unpasteurized goat milk that had been imported from Mexico. In 3 days, Gram-negative coccobacilli are isolated from blood culture specimens. The isolate is urease positive in about 2 hours. Given the patient’s history and illness, what is the most likely identification of the isolate?
a. Brucella canis
b. Brucella abortus
c. Francisella tularensis
d. Brucella suis
e. Brucella melitensis
View Answer
31. e. The clinical manifestations are consistent with brucellosis, a zoonotic disease that occurs worldwide. Brucellosis is not common in the United States, but cases occur in Texas and California due to people consuming unpasteurized goat milk products imported from Mexico. Brucella melitensis is associated with goats and sheep; B. abortus is found in cattle and buffalo; B. suis is found in swine (although B. suis biovar 4 is found in reindeer and caribou); and B. canis occurs in dogs. Brucella species are catalase-positive Gram-negative coccobacilli. Most are oxidase positive, and a key characteristic of B. melitensis, B. abortus, B. suis, and B. canis is their ability to hydrolyze urea. Most strains of B. suis and B. canis are urease positive in less than 5 minutes, while most strains of B. melitensis and B. abortus take longer than 5 minutes. Francisella tularensis is also a zoonotic Gram-negative coccobacillus. Humans often acquire F. tularensis through vector bites, such as from ticks and deer flies. Some people also get F. tularensis after exposure to infected animals such as rabbits, prairie dogs, and zoo animals. F. tularensis strains are weakly catalase positive, are oxidase positive, and do not hydrolyze urea.
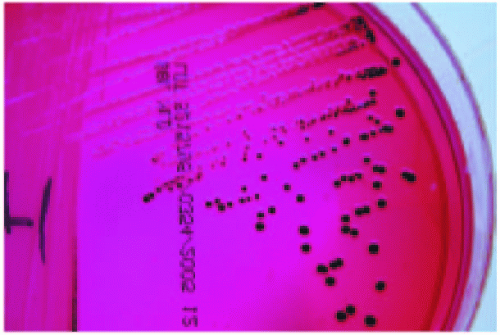
32. A 23-year-old man presents to the Emergency Department with vomiting, diarrhea, abdominal cramps, and fever. The patient says that about a day ago he ate chicken cooked on a grill at a barbecue. A sample of the patient’s diarrhea is submitted for stool culture, and the organism observed on the xylose lysine deoxycholate (XLD) agar plate shown in Figure 14.17 is isolated in aerobic conditions. What is the most likely identification of the isolate?
a. Shigella sonnei
b. Shigella dysenteriae
c. Campylobacter jejuni
d. Salmonella subspecies Enteritidis
e. Escherichia coli O157:H7
View Answer
32. d. Nontyphoidal Salmonella species cause gastroenteritis with symptoms of diarrhea, abdominal cramps, and often fever. The incubation period for Salmonella species is about 1-3 days after consuming contaminated food or water. People typically acquire Salmonella after eating contaminated poultry, raw fruits and vegetables, cheese, eggs, meat products, or drinking contaminated milk or water. In addition, some people acquire Salmonella from pet turtles. Salmonella are oxidase-negative Gram-negative rods in the family Enterobacteriaceae. The taxonomy of Salmonella is somewhat confusing. At the time of this writing, there are two Salmonella species: S. enterica and S. bongori. S. enterica is divided into six subspecies; S. enterica subsp. enterica is subspecies type I, and is the subspecies most often isolated from humans and other warm-blooded animals. Furthermore, Salmonella strains are serotyped at public health laboratories based on the O antigen (the outermost part of the lipopolysaccharide layer of the cell wall), the H antigen (the flagella), and the Vi antigen (a capsular polysaccharide, not found in all serotypes). There are many Salmonella serotypes. The most common serotypes isolated from human infections in the United States are S. enterica subsp. enterica serotype Enteritidis, abbreviated Salmonella serotype Enteritidis (or just S. Enteritidis) and Salmonella serotype Typhimurium. Since Salmonella and Shigella species are common agents of gastroenteritis, media used for stool cultures are designed to select and differentiate these two genera. There are many media available, and most laboratories use MacConkey agar and either Hektoen enteric (HE) agar or xylose lysine deoxycholate (XLD) agar for Salmonella and Shigella. XLD agar is a red-colored medium that contains xylose, lactose, and sucrose as carbohydrates, lysine to identify bacteria that have the lysine decarboxylase enzyme, phenol red as the color indicator, and ammonium citrate and sodium thiosulfate to determine whether organisms produce H2S. Shigella does not ferment any of the carbohydrates, so colonies appear colorless. Salmonella serotypes do not ferment lactose or sucrose, but most serotypes do ferment xylose, and would ordinarily have yellow colonies based on acid production; however, Salmonella serotypes use lysine in the medium with the enzyme lysine decarboxylase which produces an alkaline product. This alkalinity counters the acid production, and so Salmonella colonies also appear colorless on XLD agar. Salmonella species, though, also produce H2S, so the colonies will have black centers, and this differentiates them from Shigella species which are H2S negative. Escherichia coli strains, including E. coli O157:H7, produce yellow colonies since they ferment lactose and are lysine decarboxylase negative. Campylobacter jejuni does not grow on stool culture media used to select Shigella and Salmonella, so it requires specialized media—Campylobacter blood agar is used in most laboratories—and microaerophilic growth conditions.
33. An individual who handles fish presents with a welldefined, violaceous lesion on his right index finger. The lesion is painful, and the finger has swelled.
A biopsy specimen is sent for culture and in 24 hours nonhemolytic, pleomorphic Gram-positive rods are isolated on sheep blood agar and chocolate agar. The isolate is catalase negative. It was inoculated into a triple sugar iron (TSI) agar slant, and the result is shown in Figure 14.18 (left slant shows an uninoculated control, right slant is the isolate). What is the identity of the isolate?
A biopsy specimen is sent for culture and in 24 hours nonhemolytic, pleomorphic Gram-positive rods are isolated on sheep blood agar and chocolate agar. The isolate is catalase negative. It was inoculated into a triple sugar iron (TSI) agar slant, and the result is shown in Figure 14.18 (left slant shows an uninoculated control, right slant is the isolate). What is the identity of the isolate?
a. Listeria monocytogenes
b. Erysipelothrix rhusiopathiae
c. Arcanobacterium haemolyticum
d. Corynebacterium ulcerans
e. Bacillus anthracis
View Answer
33. b. Erysipelothrix rhusiopathiae is a zoonotic organism that is associated with a wide variety of animals, including pigs, fish, and birds. The organism causes erysipeloid, a localized cellulitis with a violaceous, painful lesion, and also causes bacteremia with or without endocarditis. Humans typically acquire E. rhusiopathiae by handling infected animals or animal products, so disease caused by the organism is usually occupational. The organism gets into breaks in the skin to cause erysipeloid. E. rhusiopathiae is gram-positive rod that may form chains. It may take 1-3 days for colonies to appear on media. On sheep blood agar, colonies are usually nonhemolytic and pinpoint after 24 hours of incubation. After 48 hours of incubation, colonies are larger and may appear alpha-hemolytic. E. rhusiopathiae is the only clinically relevant grampositive rod that produces H2S in triple sugar iron (TSI) agar (Fig. 14.18). In addition, E. rhusiopathiae is catalase negative and does not form spores. Listeria monocytogenes is catalase positive, H2S negative, and beta hemolytic on sheep blood agar. Corynebacterium species are catalase positive and H2S negative. Bacillus anthracis is catalase positive, forms spores, and is also H2S negative. Arcanobacterium haemolyticum is catalase negative, is beta hemolytic on sheep blood agar, and is H2S negative.
34. Which statement concerning the MacConkey agar plate shown in Figure 14.19A is incorrect?
a. The organism is a nonlactose fermenter.
b. The organism is a lactose fermenter.
c. The organism may be a Salmonella species.
d. The organism may be a Shigella species.
e. The organism may be a Proteus species.
View Answer
34. b. MacConkey agar is a pink-colored medium used for most types of cultures in the bacteriology laboratory. It is a selective and differential medium used to isolate Gram-negative bacteria. MacConkey agar contains lactose as the only carbohydrate, peptones, bile and crystal violet to inhibit Gram-positive organisms, and neutral red as the pH indicator. Lactose fermentation results in the production of acid, which drops the pH of the medium. Lactose fermenters appear dark red on MacConkey agar, often with a darkish red precipitate around the colonies as well. The primary lactose fermenters include Escherichia coli, Klebsiella species, and some Enterobacter and Citrobacter species; Fig. 14.19B shows a lactose-fermenting E. coli isolate on MacConkey agar. Non-lactose fermenters, on the other hand, utilize the peptones in the medium, which produces alkaline by-products. Under alkaline conditions, the medium turns colorless, and colonies appear colorless as well (Fig. 14.19A). Shigella, Salmonella, and Yersinia enterocolitica are the primary stool pathogens that do not ferment lactose. However, many members of the Enterobacteriaceae do not ferment lactose, such as Proteus species. Thus, MacConkey agar does not differentiate between non-lactose-fermenters, but does select for non-lactose-fermenting Gram-negative bacteria.
35. An acid-fast bacillus is cultured from a patient with chronic pulmonary disease. The isolate took about 30 days to grow, and Figure 14.20 shows the organism grown in the dark (left slant) and when exposed to light (right slant). What is the most likely identity of the isolate?
a. Mycobacterium kansasii
b. Mycobacterium avium-intracellulare
c. Mycobacterium tuberculosis
d. Mycobacterium gordonae
e. Mycobacterium abscessus
View Answer
35. a. Figure 14.20 shows two Lowenstein-Jensen agar slants inoculated with the same slow-growing acid-fast bacillus. Buff-colored (nonpigmented) bacteria are evident on the left slant that was incubated in dark conditions. Yellow-pigmented bacteria are visible on the right slant that was exposed to light. This is typical of certain mycobacteria called photochromogens. In general, mycobacteria are often divided into two groups, the Mycobacterium tuberculosis complex and the nontuberculous mycobacteria (NTMs). The NTMs may be further divided into four groups: the photochromogens (develop pigment after exposure to light), the scotochromogens (develop pigment in both the light and the dark), the nonphotochromogens (nonpigmented regardless of the light conditions) and the rapid growers. The photochromogens, scotochromogens, and nonphotochromogens are all slow-growing mycobacteria—they take longer than 7 days to grow on solid media. Mycobacteria that grow faster than 7 days on solid media are the rapid growers. M. kansasii is a photochromogen that is associated with chronic pulmonary infections and occasional extrapulmonary infections such as cervical lymphadenitis and cutaneous infections. M. avium-intracellulare causes chronic pulmonary disease, extrapulmonary infections, and disseminated disease, particularly in immunocompromised patients, and is nearly always nonpigmented. M. tuberculosis is a nonpigmented, slow-growing organism, and M. gordonae is a scotochromogen and is rarely, if ever, considered a pathogen. M. abscessus is a rapid-growing species that causes pulmonary infections, disseminated disease, and skin and soft tissue infections.
36. A 5-year-old boy is bitten on the arm by a 6-month-old kitten and develops cellulitis. An oxidase-positive, catalase-positive, Gram-negative coccobacillus is isolated from purulence from the wound. The isolate, shown in Figure 14.21, grows well in aerobic conditions on sheep blood and chocolate agars in 24 hours, does not grow on MacConkey agar, and is indole positive. What is the most likely identity of the isolate?
a. Eikenella corrodens
b. Haemophilus influenzae
c. Pasteurella multocida
d. Bartonella henselae
e. Pseudomonas aeruginosa
View Answer
36. c. Pasteurella multocida is a commensal found in the nasopharynx and oral cavity of animals, particularly dogs and cats. Humans usually become infected with P. multocida after bites or scratches. Some people get infected when pets lick skin lesions or sores. The organism usually causes cellulitis at the site of infection, but may also cause meningitis, arthritis, endocarditis, osteomyelitis, septicemia, and respiratory infections. P. multocida is an oxidase-positive, catalase-positive, Gram-negative coccobacillus. It grows well on solid media, although it does not grow on MacConkey agar, and is indole positive. Thus, a Gram-negative isolate from a bite wound that grows well on blood agar but not on MacConkey agar should be suspicious for P. multocida. Eikenella corrodens is a member of the human oral flora, and also in some animals. It is associated with human bite wounds, clenched fist injuries, oral infections, and endocarditis. It is oxidase positive, does not grow on MacConkey agar, and is catalase- and indole negative. Haemophilus influenzae is more fastidious than P. multocida, and does not grow on sheep blood agar or on MacConkey agar. It is not associated with animal bite wounds, but instead causes meningitis, pneumonia, epiglottitis, and many other infections. Bartonella henselae is associated with cat-scratch disease, bacillary angiomatosis, and bacillary peliosis, but is a slow-growing, fastidious organism that is difficult to culture. B. henselae will grow on blood agar, but requires incubation for 4 weeks. Pseudomonas aeruginosa is not fastidious, and will grow well on MacConkey agar. It is oxidase positive, but is indole negative.
37. A 26-year-old man from rural Massachusetts is seen by his physician with symptoms of fatigue, chills, fever, headache, and malaise. The patient has a small red lesion with an annular rash at the site of a previous tick bite on his trunk. The patient reports that he pulled a small tick from the site of the lesion a few weeks ago. What is the most likely agent of the patient’s disease?
a. Rickettsia rickettsii
b. Borrelia burgdorferi
c. Borrelia recurrentis
d. Leptospira interrogans
e. Francisella tularensis
View Answer
37. b. The nonspecific symptoms with an annular rash, the tick bite history of the patient, and the geographical area of the patient are characteristic of infection with Borrelia burgdorferi, the agent of Lyme borreliosis or Lyme disease. B. burgdorferi is a Gram-negative spirochete that is now divided into three species: B. burgdorferi sensu stricto, B. afzelii, and B. garinii. B. burgdorferi sensu stricto is the only species of the group that has been isolated from humans in North America, while all three species have been isolated from humans in Europe. The organisms are transmitted to humans by the bite of Ixodes ticks. Lyme borreliosis is characterized by an annular-shaped lesion called erythema migrans (EM). EM is present in 60% to 90% of patients at the bite site of the tick. In many patients, the central portion of the lesion fades so that it has a bull’s eye appearance. Other symptoms of Lyme borreliosis include headache, fever, fatigue, malaise, arthralgia, and myalgia. Untreated patients can develop neurologic and cardiac complications. Borrelia recurrentis is an agent of relapsing fever, and is spread by the human body louse (Pediculus humanus humanus). Leptospira interrogans is a zoonotic spirochete that is transmitted to humans after contact with urine from infected animals. It causes disease worldwide, with symptoms of fever, chills, headache, abdominal pain, and conjunctival suffusion. Some patients develop icteric disease (Weil disease) and renal failure. Rickettsia rickettsii is an obligate intracellular pathogen that is transmitted to humans by tick bites, and does occur on the eastern seaboard. It is more common in the southeastern part of the United States, such as North Carolina, South Carolina, and Virginia. It is not characterized by an EM-like rash, but instead by a petechial rash that often appears on the palms and soles. Francisella tularensis can also be spread to humans via tick bites and deer fly bites. It is a gram-negative coccobacillus, and disease is not characterized by an EM-like rash.
38. A 28-year-old woman presents to the Emergency Department with fever, vomiting, bloody diarrhea, and abdominal pain. She says that she may have eaten undercooked chicken a few days ago at a party. A curved, faintly staining Gram-negative rod (Fig. 14.22) was isolated on specialized blood agar from a stool sample submitted to the lab. The isolate is oxidase positive and grew in a microaerophilic atmosphere at 42°C. The isolate did not grow on either MacConkey agar or Hektoen enteric agar in an aerobic atmosphere. In addition, leukocytes were observed in a methylene blue stain of the stool. Based on this evidence, what is the likely identity of this food poisoning agent?
a. Vibrio cholerae
b. Escherichia coli O157:H7
c. Salmonella serotype Typhi
d. Campylobacter jejuni
e. Shigella sonnei
View Answer
38. d. Campylobacter jejuni causes gastroenteritis characterized by abdominal cramping, fever, and diarrhea, which is often bloody. Fecal white blood cells may be present in stool specimens of patients with C. jejuni gastroenteritis. C. jejuni infections most commonly occur in the summer months, and people usually acquire the organism by eating contaminated or improperly cooked food. The organism requires specialized media for isolation. A commonly used medium is Campylobacter blood agar, which is brucella agar with sheep blood and antimicrobial agents to inhibit normal stool flora. It does not grow on other media used in stool cultures, such as MacConkey agar, Hektoen enteric agar, or xylose lysine deoxycholate (XLD) agar. Thus, a Campylobacter blood agar plate is included in the standard media package used when a stool culture is ordered. In addition, C. jejuni requires a microaerophilic atmosphere (5% O2, 10% CO2, 85% N2) and is usually cultured at 42°C. It is a curved or S-shaped Gram-negative rod that tends to stain faintly (Fig. 14.22). C. jejuni is oxidase positive, catalase positive, and hippurate hydrolysis positive; these characteristics, along with growth at 42°C, serve to differentiate it from other Campylobacter species. Vibrio cholerae is also an oxidase positive, curved gram-negative rod that causes gastroenteritis. V. cholerae strains usually do not cause bloody diarrhea, and they grow aerobically in culture. Thiosulfate citrate bile salts sucrose (TCBS) agar is the selective medium usually used for Vibrio species. Escherichia coli O157:H7 causes gastroenteritis that is sometimes characterized by bloody stools, abdominal cramping, and low-grade fever. Like other E. coli strains, E. coli O157 isolates are oxidase negative and will grow in aerobic conditions. MacConkey agar with sorbitol is the medium usually used to select for E. coli O157. Salmonella serotype Typhi causes typhoid fever, a disease that presents with a diarrheal phase followed by a febrile illness. The incubation period for S. serotype Typhi is 7-14 days on average. The organism grows well on most media, but is usually isolated best from blood cultures or bone marrow cultures. It does not require a special atmosphere for growth, is oxidase negative, and is not curved on Gram stain. Shigella sonnei is one of the four different Shigella species. Shigella species cause bacillary dysentery, and symptoms may include bloody diarrhea, fever, tenesmus, and abdominal cramping. Fecal white blood cells are often found in stool specimens. Shigella species do not require a special atmosphere for isolation, are oxidase negative, and are not curved on Gram stain. MacConkey agar and Hektoen enteric agar or XLD agar would be excellent media choices to select for Shigella species such as S. sonnei.
39. Figure 14.23 depicts a disk diffusion test with a Klebsiella pneumoniae isolate. The isolate is resistant to ceftazidime (zone size 12 mm); the zone size for ceftazidime-clavulanic acid is 22 mm. Which of the following is true for this scenario?
a. The isolate is confirmed to be an extended spectrum β-lactamase (ESBL) producer.
b. The disk diffusion test shown in Figure 14.23 is an ESBL screening test, not a confirmatory test.
c. This is a typical pattern of antibiotic resistance for Escherichia coli.
d. The disk diffusion test shown in Figure 14.23 is invalid because the zone size for ceftazidime-clavulanic acid should be less than the ceftazidime zone size to confirm an ESBL.
e. The isolate is confirmed to be an AmpC hyperproducer.
View Answer
39. a. There are various methods that can be used to confirm the presence of an extended spectrum beta-lactamase (ESBL) in certain Gram-negative bacteria. Currently, according to the Clinical and Laboratory Standards Institute (CLSI), ESBL testing should be performed only for Klebsiella pneumoniae, Klebsiella oxytoca, Escherichia coli, or Proteus mirabilis isolates. In these organisms, ESBLs are important acquired enzymes. Organisms with ESBLs cannot be effectively treated with the penicillins, cephalosporins, or aztreonam. In E. coli, K. pneumoniae, and K. oxytoca, the following antibiotics can be used to screen for the presence of an ESBL: ceftazidime, ceftriaxone, cefotaxime, cefpodoxime, or aztreonam. Ceftazidime, cefotaxime, or cefpodoxime can be used to screen for ESBLs in P. mirabilis. These organisms are not normally resistant to these antibiotics, thus they are good screening agents. Confirmatory testing can be performed by either disc diffusion or by broth microdilution. Figure 14.23 shows an example of a disk diffusion confirmatory test for an ESBL-producing K. pneumoniae. By either disk diffusion or broth microdilution, the following combinations are tested: ceftazidime compared to ceftazidime with the beta-lactamase inhibitor clavulanic acid and cefotaxime compared to cefotaxime with clavulanic acid. If an ESBL is present, the zone size in disk diffusion will be at least 5 mm larger around the antibiotic with clavulanic acid inhibitor compared to the antibiotic alone. This is due to the inhibition effect of the clavulanic acid. For example, if the ceftazidime zone size is 16 mm, the ceftazidime with clavulanic acid zone size must be 21 mm or greater to confirm the presence of an ESBL. An ESBL is confirmed if this zone size difference is noted for either of the pairs of disks. For the broth microdilution confirmatory method, a ≥3 twofold concentration decrease must be noted with one of the tested pairs of antibiotics compared to the antibiotic/clavulanic acid counterpart. For example, if the MIC for ceftazidime is 8 µg/ml, the ceftazidime/clavulanic acid MIC must be 1 µg/ml to confirm the presence of an ESBL. In contrast, potential AmpC hyperproducing organisms include Serratia marcescens, Pseudomonas aeruginosa, Providencia species, Citrobacter freundii, Enterobacter cloacae, Enterobacter aerogenes, and Morganella morganii (the so-called “SPiCEM” organisms). The AmpC gene for these organisms is chromosomal, and may be induced by low levels of various β-lactam antibiotics. Mutations in the induction pathway may result in AmpC hyperproduction. In addition, there are also plasmid-mediated AmpCs. AmpC hyperproducers are very resistant to β-lactam antibiotics. A good screening test for AmpC hyperproduction is cefoxitin. The AmpC enzymes are resistant to beta-lactamase inhibitors such as clavulanic acid, so the confirmatory tests used for ESBLs cannot be used to confirm AmpC hyperproduction. Currently, there are no CLSI-recommended tests for AmpC confirmation.
40. A 35-year-old man from Virginia is brought to the Emergency Department by his wife with a rash, fever, nausea, vomiting, diarrhea, and abdominal pain. His illness began 3 days ago with a fever, headache, and myalgias. The rash started on the trunk but has since spread to the patient’s palms and soles. A week ago he went hunting and pulled a deeply embedded tick off of his trunk after he got home. Given the patient’s history and symptoms, what is the most likely etiologic agent?
a. Coxiella burnetii
b. Rickettsia prowazekii
c. Anaplasma phagocytophilum
d. Borrelia burgdorferi
e. Rickettsia rickettsii
View Answer
40. e. Rickettsia rickettsii is an obligate intracellular pathogen. It is transferred to humans by tick bites; the usual vector in the United States is Dermacentor species (D. variabilis in the east and D. andersoni in the west). R. rickettsii is the etiologic agent of Rocky Mountain spotted fever (RMSF). The incubation period for RMSF averages about 7 days. The disease is initially characterized most often by fever, headache, and myalgia. Some individuals also present with nausea, abdominal pain, vomiting, and diarrhea. The major clinical manifestation, though, is a petechial rash that usually begins 3-5 days after the onset of fever and is present in 90% of all patients. The rash often begins on the wrists and ankles, but may also occur on the trunk. Eventually, the rash spreads to the palms and soles in most patients. RMSF is most common in the southeastern and south central United States. Rickettsia prowazekii is the agent of louse-borne or epidemic typhus. It is spread to humans by the human body louse (Pediculus humanus corporis). The symptoms may be similar to RMSF, although the rash caused by R. prowazekii infection does not normally include the palms and soles. Epidemic typhus is endemic in Mexico, Central and South America, parts of Africa, and in Asia. In the United States, R. prowazekii persists in Southern flying squirrels, and humans may acquire the organism via flying squirrel fleas, although it is not a common disease. Coxiella burnetii is the causative agent of Q fever. Q fever is a zoonosis that occurs worldwide. Humans are usually infected by inhaling contaminated aerosols when organisms are shed in urine, feces, milk, and in animal birth products. Q fever is usually an occupational disease, and there are several different clinical manifestations, including a febrile illness, pneumonia, endocarditis, hepatitis, osteomyelitis, and neurologic manifestations. Anaplasma phagocytophilum causes human granulocytotropic anaplasmosis (HGA), a disease that is similar to RMSF and human monocytic ehrlichiosis (HME, caused by Ehrlichia chaffeensis). Like R. rickettsii, A. phagocytophilum is transferred to humans by the bite of ticks. However, patients with HGA rarely present with a rash, and HGA tends to occur in the northeastern and upper Midwestern states. Cases occur in northern California as well. Borrelia burgdorferi is a spirochete that is also transmitted by ticks. The disease it causes, Lyme borreliosis, is characterized by an annular rash (erythema migrans) that often looks like a bull’s eye. The rash of Lyme borreliosis occurs at the bite site of the tick, and does not appear on the palms or soles unless one of those areas is bitten by a tick.
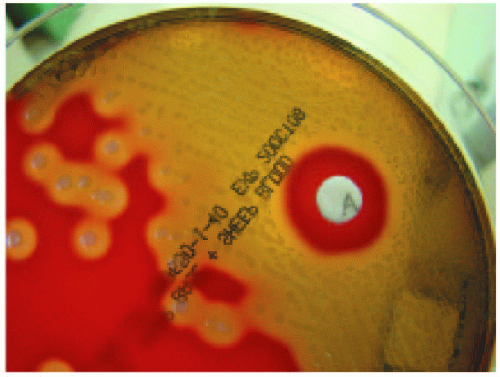
41. A 45-year-old woman injection-drug user presents to the Emergency Department with fever, chills, and malaise. A physical examination of the patient reveals swelling, pain, and erythema at a drug injection site on her left arm. Purulent material is submitted to the lab from the injection site. A Gram stain of the pus reveals many Gram-positive cocci in chains and many white blood cells. In 18 hours, a β-hemolytic, catalase-negative, Gram-positive coccus is isolated. A subculture of the organism on a sheep blood agar plate with a bacitracin disk (A disk) is shown in Figure 14.24. What is the most likely identification of the isolate?
a. Streptococcus agalactiae
b. Staphylococcus aureus
c. Streptococcus pyogenes
d. Enterococcus faecium
e. Streptococcus milleri group
View Answer
41. c. Streptococcus pyogenes is the primary cause of bacterial pharyngitis, and is responsible for many other types of infections, including impetigo, sepsis, soft tissue infections, erysipelas, cellulitis, necrotizing fasciitis, endocarditis, pneumonia, osteomyelitis, and scarlet fever. It is a Gram-positive coccus that appears in chains, is catalase negative like other streptococci, and is susceptible to bacitracin (A disk). S. pyogenes colonies on sheep blood agar are large with large zones of beta hemolysis, as shown in Figure 14.24. The A disk is no longer considered confirmatory for identification of S. pyogenes; some strains of other beta-hemolytic streptococci are also susceptible to bacitracin. Instead, most labs use a rapid kit to determine the presence of the Lancefield group A antigen present in the cell wall of S. pyogenes strains. Streptococcus agalactiae is a softly beta-hemolytic streptococcus, and has the group B Lancefield antigen. It is resistant to bacitracin and CAMP test positive. It is associated with many infections as well, such as early-onset neonatal disease, late-onset neonatal meningitis, urinary tract infections, soft tissue infections, pneumonia, and osteomyelitis. The Streptococcus milleri group, also known as the Streptococcus anginosus group, consists of the organisms S. anginosus, S. constellatus, and S. intermedius. Strains of these organisms may carry the Lancefield group A, C, F, or G antigens, or may have no Lancefield group antigen. In addition, these organisms are variable in their hemolytic pattern. All are resistant to bacitracin, and their colonies are small in relation to S. pyogenes and S. agalactiae. Organisms in the S. anginosus group cause abscesses in the peritoneal cavity, in the brain, and in the oropharynx. Enterococcus faecium and other enterococci are associated with infections in immunocompromised patients, the elderly, or those who have been hospitalized for long periods. E. faecium is catalase negative, and usually appears as pairs or small chains of Gram-positive cocci. Strains of E. faecium are nonhemolytic or alpha hemolytic on sheep blood agar. Staphylococcus aureus is a significant pathogen, and causes many of the same diseases as S. pyogenes. S. aureus, like other staphylococci, is catalase positive. S. aureus colonies are usually larger than those of S. pyogenes, and are also beta-hemolytic on sheep blood agar.
42. A 4-year-old Native American boy is brought to a clinic with a fever, malaise, and a sore throat. A white membrane is observed on the child’s tonsils. The child has not had all of his immunizations. A throat culture is submitted, and black colonies are observed on cystinetellurite blood agar after 48 hours of growth. On Tinsdale agar, the colonies are black with dark brown halos. A Gram stain of the isolate shows pleomorphic Gram-positive rods. The organism is catalase positive and does not produce urease. What is the probable identity of the isolate?
a. Streptococcus pyogenes
b. Corynebacterium pseudotuberculosis
c. Arcanobacterium haemolyticum
d. Corynebacterium ulcerans
e. Corynebacterium diphtheriae
View Answer
42. e. Corynebacterium diphtheriae is a catalase-positive, pleomorphic, Gram-positive rod that is the causative agent of diphtheria. While rates of diphtheria in the United States have declined dramatically since the introduction of a vaccine, cases still appear in individuals who have not been vaccinated. In the mid-1990s, there was an epidemic of diphtheria in Russia and surrounding countries. Diphtheria may occur as a respiratory disease or as a cutaneous disease. The respiratory disease is characterized by pharyngitis with an associated nasopharyngeal membrane, low-grade fever, adenopathy, and hoarseness. Most of the virulence of C. diphtheriae is the result of diphtheria toxin that is encoded by a bacteriophage that infects the organism. The toxin may cause severe complications, such as kidney damage, myocarditis, and neuritis. Nontoxigenic strains may still cause cutaneous disease or endocarditis. To determine toxin production, the Elek test or the polymerase chain reaction is often performed. If C. diphtheriae is suspected, specialized media are usually used for culture isolation. Samples should be plated on sheep blood agar and a selective medium such as cystine-tellurite blood agar (CTBA) or Tinsdale medium. C. diphtheriae colonies are black on CTBA and black or brown on Tinsdale medium with a brown halo around the colonies. Unfortunately, C. pseudotuberculosis and C. ulcerans also produce the same types of colonies on CTBA and Tinsdale medium. Because they can cause similar respiratory diseases to diphtheria, C. diphtheriae must be differentiated from these two organisms. C. diphtheriae is urease negative, while C. pseudotuberculosis and C. ulcerans are urease positive. Streptococcus pyogenes is the main bacterial cause of pharyngitis, but it is a catalase-negative Gram-positive coccus that appears in chains. Arcanobacterium haemolyticum is also an agent of pharyngitis. It is a beta-hemolytic, Gram-positive rod. Unlike C. diphtheriae, A. haemolyticum is catalase negative.
43. A 57-year-old man is hospitalized with sepsis and two sets of blood cultures are drawn. Gram- positive cocci in chains are observed in all four bottles in one day. Subcultures of the bottles reveal catalase- negative, nonhemolytic Gram-positive cocci. The organism grows on a bile esculin agar slant (Fig. 14.25B; Fig. 14.25A is a negative control) and types with the group D Lancefield antigen. In addition, the isolate does not grow in the presence of 6.5% salt. Further testing is performed on the patient, and it is found that he has colon cancer. Based on this information, what is the most likely identity of the blood culture isolate?
a. Streptococcus bovis
b. Enterococcus faecalis
c. Enterococcus faecium
d. Streptococcus agalactiae
e. Streptococcus dysgalactiae subsp. equisimilis
View Answer
43. a. Streptococcus bovis is an organism that closely resembles enterococci on media and shares similar biochemical characteristics in that it grows in the presence of bile, hydrolyzes esculin, and is catalase negative. The enterococci, though, grow in the presence of 6.5% sodium chloride, while S. bovis does not. In addition, enterococci are pyrrolidonyl arylamidase (PYR) positive, while S. bovis is negative. S. bovis is Lancefield group D antigen positive. S. bovis is an inhabitant of the human gastrointestinal tract. It primarily causes bacteremia and endocarditis, and there is a strong association between S. bovis bacteremia and colon malignancy. All individuals with S. bovis bacteremia should be tested for colon carcinoma. Streptococcus agalactiae, or group B streptococcus, is beta-hemolytic, is esculin hydrolysis negative, and does not grow in the presence of bile. Streptococcus dysgalactiae subsp. equisimilis usually isolates type with either Lancefield group C or G. Most of these isolates are beta-hemolytic on sheep blood agar. S. dysgalactiae subsp. equisimilis are associated with many of the same infections as Streptococcus pyogenes.
44. Which of the following is often used to isolate Mycoplasma pneumoniae?
a. A8 agar
b. SP-4 medium
c. McCoy cells
d. Middlebrook 7H10 agar
e. BACTEC 12B medium
View Answer
44. b. The mycoplasmas are the smallest known free-living bacteria. They do not have a cell wall. Several are significant human pathogens. Mycoplasma pneumoniae causes community-acquired pneumonia and upper respiratory tract infections. Mycoplasma hominis and Ureaplasma urealyticum cause urogenital tract infections, systemic diseases in neonates (such as meningitis and pneumonia), and invasive disease in immunocompromised patients. The mycoplasmas can be cultured on solid and liquid media. SP-4 medium is often used to isolate M. pneumoniae. Cultures should be held for 4 weeks, and most laboratories examine the agar surface every 1-3 days with a microscope to observe colonies. A8 agar medium is used to isolate U. urealyticum and M. hominis. McCoy cells are used to isolate Chlamydia trachomatis. Middlebrook 7H10 agar and BACTEC 12B medium are used to recover Mycobacterium species.
45. A 70-year-old woman with chronic obstructive pulmonary disorder (COPD) developed fever, cough, and purulent sputum. Patchy infiltrates were observed on a chest x-ray, and a sample of her expectorated sputum was sent to the lab for analysis. A Gram stain of the sputum revealed many small, Gram-negative coccobacilli and many white blood cells. On culture, a Gram-negative coccobacillus grows only on chocolate agar after 24 hours in increased CO2 (Fig. 14.26A); the isolate does not grow on either sheep blood agar or MacConkey agar. X and V factor requirements were determined as shown in Figure 14.26B. Furthermore, the isolate was found to be nonhemolytic on rabbit blood agar. Based on these data, what is the most likely identity of the isolate?
a. H. influenzae
b. Haemophilus parainfluenzae
c. Haemophilus haemolyticus
d. Haemophilus paraphrophilus
e. Haemophilus parahaemolyticus
View Answer
45. a. Haemophilus influenzae is a fastidious, gram-negative coccobacillus. It is a significant human pathogen, and some strains are encapsulated. Encapsulated strains are usually the most pathogenic. There are six known H. influenzae capsule types: a, b, c, d, e, and f. Capsule type b was once the most common type involved in serious infections, but there is an effective type B vaccine now. The encapsulated H. influenzae strains are associated with meningitis, epiglottitis, cellulitis, pneumonia, septic arthritis, and bacteremia. Nonencapsulated strains cause otitis media, conjunctivitis, sinusitis, and pneumonia and bacteremia in immunocompromised patients. The Haemophilus species, in general, require hemin (X factor) and NAD (V factor) for growth. A given Haemophilus isolate can be streaked on a plate with both X and V impregnated filter papers to determine which factors are required. If the isolate grows in between the X and V filter papers, then it requires both X and V for growth. H. influenzae requires both X and V factors (Fig. 14.26B). H. haemolyticus also requires both X and V factors for growth; however, it is beta-hemolytic on rabbit blood agar, while H. influenzae is not. Chocolate agar provides both X and V factors, but sheep blood agar provides only hemin. Haemophilus species are usually colorless on chocolate agar (Fig. 14.26A). H. influenzae will also grow as tiny colonies around Staphylococcus aureus streaked on sheep blood agar. This is known as satelliting and occurs because S. aureus produces NAD as a by-product. All of the Haemophilus “para” (H. parahaemolyticus, H. parainfluenzae, H. paraphrophilus) species require only V factor for growth.
46. A 5-year-old girl returns from a trip to India with her family and a week later develops diarrhea that lasts for 4 days. Then, she gradually develops fever, abdominal pain, sore throat, and chills. A physical exam of the girl reveals hepatosplenomegaly. Blood cultures are drawn, and Gram-negative rods are observed in all bottles in 24 hours. The isolate is subcultured to solid media. The organism is oxidase negative, indole negative, urease negative, ornithine decarboxylase negative, and a nonlactose fermenter on MacConkey agar. The isolate was inoculated into a TSI agar slant and is shown in Figure 14.27A. Based on this information and the patient’s history, what is the likely identity of the isolate?
a. Shigella dysenteriae