Mediastinoscopy and Mediastinotomy
Phillip C. Camp
M. Victoria Gerken
The surgeon is frequently called on to evaluate mediastinal lymph nodes. This may be done for diagnosis of an isolated mediastinal mass or significant mediastinal adenopathy. Examples include cases of sarcoidosis (more than 90% of which will show noncaseating granulomas within the hilar or scalene lymph nodes) or with lymphoma (isolated mediastinal disease is more commonly Hodgkin’s). Improved imaging modalities such as helical computed tomography scan, positron emission tomography scanning, magnetic resonance imaging, octreotide-based imaging, and antibody-based imaging have increased the ability to screen the mediastinum. However, no noninvasive test has matched the sensitivity and specificity of lymph node sampling. Lymph nodes from zones II, IV, and VII, as well as from zone V, can be safely sampled using mediastinoscopy.
Steps in Procedure
Mediastinoscopy
Position patient with neck in full extension and shoulders elevated
Incision two fingerbreadths cephalad to suprasternal notch
Dissect to level of strap muscles, ligating any veins that are encountered
Divide connective tissue of midline until trachea is encountered
Pass moistened index finger down into anterior mediastinum, keeping fingernail adjacent to tracheal rings
Introduce saline-moistened mediastinoscope
Keep field dry and bluntly dissect around lymph nodes with long blunt metal suction tip
Carefully isolate and clean node, consider aspiration before biopsy to avoid inadvertent entry into major vascular structure
Expose node sufficiently to perform biopsy under direct vision
Obtain hemostasis and check field under saline for evidence of pleural injury
Close incision in layers
Mediastinotomy
Incise skin over third costal cartilage
Expose and resect segment of costal cartilage and rib
Palpate and expose ascending arch of aorta and window between aorta and pulmonary artery
Insert mediastinoscopy and perform gentle dissection and identification of nodes as previously noted
Perform biopsy
Obtain hemostasis and check for air leak or pleural entry
Close incision in layers
Hallmark Anatomic Complications
Injury to aorta or other major systemic artery
Injury to pulmonary artery
Injury to recurrent laryngeal nerve
Pleural entry
List of Structures
Trachea
Pretracheal fascia
Carina
Thyroid
Sternum
Manubrium
Clavicle
Sternoclavicular joint
Sternocleidomastoid muscle
Right pulmonary artery
Aorta
Brachiocephalic (innominate) artery
Left common carotid artery
Left subclavian artery
Superior Vena Cava
Azygos vein
Anterior Jugular Vein
Inferior thyroid vein
Thymus
Brachiocephalic (innominate) vein
Pleura
Left recurrent laryngeal nerve
Right recurrent laryngeal nerve
Esophagus
Paratracheal lymph nodes
Tracheobronchial lymph nodes
Scalene nodes
Perichondrium
Periosteum
Internal thoracic (mammary) artery
Mediastinoscopy
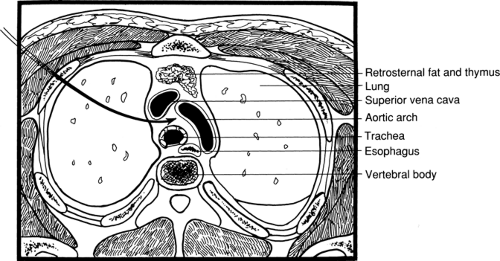
Mediastinoscopy is performed to evaluate pretracheal and paratracheal lymphadenopathy. It involves the creation of a tunnel or a space just anterior to the trachea and posterior to the aortic arch. As such, it does not provide access to the retrosternal space, the subcarinal space, or the left hilum.
The procedure is performed under general anesthesia. In special circumstances, local anesthesia may be used; however, this will significantly increase the difficulty and risk of the operation.
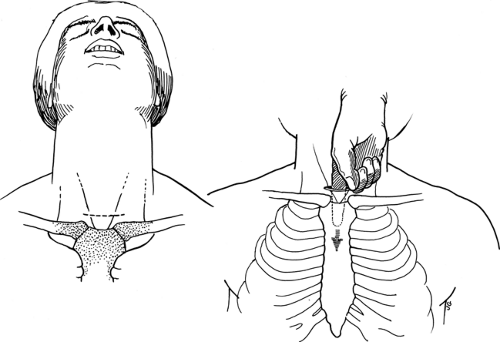
Skin Incision and Exposure of the Pretracheal Fascia (Fig. 20.1)
Technical Points
Good head position allows adequate exposure. The neck should be in full extension with the shoulders elevated. The entire neck and chest should be prepared into the surgical field in case a more extensive exposure is quickly required. As with any neck scar, asymmetry leads to an unaesthetic result, and marking the intended site often results in a more pleasing closure. Make the skin incision about two fingerbreadths cephalad to the suprasternal notch. The incision need only be 2 to 3 cm long, enough to accommodate the mediastinoscope, extending only to the anterior borders of the sternocleidomastoid muscle. Carry the incision down by electrocautery through the subcutaneous tissue to the level of the strap muscles. Sizable veins (anterior jugular veins) can run in this tissue and may require formal ligation with silk ties. Identify the midline as a fine, pale-yellow line. Incise this connective tissue with electrocautery or Metzenbaum scissors superiorly and inferiorly, and retract the strap muscles vertically. Divide the connective tissue of the midline by sharp dissection or electrocautery until the trachea is encountered. Incise the pretracheal fascia to allow access to the correct tissue plane, just anterior to the trachea itself.
Anatomic Points
When making the incision, the trachea will be exposed at about the same location as in tracheostomy, caudal to the thyroid. The inferior thyroid vein can often pass cephalad in the midline and requires careful mobilization and lateral retraction.
As the surgeon’s finger passes under the manubrium, the back of the aortic arch is palpated just as it gives off the brachiocephalic (innominate) artery. Place a pulse oximeter on a finger of the patient’s right hand to monitor compression of this artery during the procedure.
Development of the Mediastinal Tunnel and Passage of the Mediastinoscope (Fig. 20.2)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree