Maximizing Vein Conduit for Autogenous Bypass
Gregory J. Landry
DEFINITION
Autogenous conduit is preferred for all lower extremity bypasses when available. The greater saphenous vein (GSV) is the most frequently used conduit. Other options for native conduit include the short saphenous vein, arm vein (basilic, cephalic, brachial), and femoral vein.
DIFFERENTIAL DIAGNOSIS
The majority of patients for whom autogenous vein bypass is necessary will have atherosclerotic peripheral vascular disease.
Other conditions for which autogenous vein bypass may be necessary include aneurysms (e.g., femoral, popliteal), trauma, and vasculitis.
PATIENT HISTORY AND PHYSICAL FINDINGS
A history of cardiovascular risk factors should be elicited in all patients undergoing lower extremity bypass, including smoking history and history of cardiac and cerebrovascular disease and history of diabetes, chronic kidney disease, hyperlipidemia, and chronic obstructive pulmonary disease.
Upper and lower extremity pulse exam should be performed. Because atherosclerosis is a systemic disorder, the following pulses should be assessed bilaterally: carotid, brachial, radial, femoral, popliteal, dorsalis pedis, and posterior tibial. Both the presence and strength of pulses should be recorded.
If lower extremity pulses are absent, which is usually the case in patients undergoing surgery for peripheral vascular disease, ankle-brachial indices should be measured. The highest ankle pressure is divided by the highest brachial pressure.
Lower extremities should be evaluated for the presence of ulcerations or gangrene.
A history of prior vein use or removal should be elicited. Veins may have previously been used for prior lower extremity or coronary artery bypass. Patients with varicose veins may have undergone prior vein stripping or ablation. Patients with chronic kidney disease may have had prior upper extremity arteriovenous fistula placement. In dialysis-dependent patients, upper extremity veins should be used judiciously as they may be necessary for future arteriovenous access.
IMAGING AND OTHER DIAGNOSTIC STUDIES
All patients considered for lower extremity bypass should undergo arteriography to define the proximal (inflow) and distal (outflow) targets.
Digital subtraction angiography remains the gold standard and provides the greatest anatomic detail for operative planning.
Alternative imaging modalities include computed tomography (CT) and magnetic resonance (MR) angiography or duplex ultrasonography.
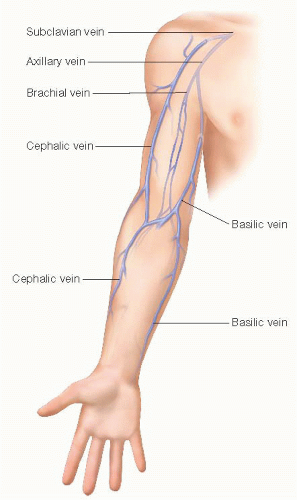
Duplex ultrasonography should be used for preoperative vein mapping to identify suitable autogenous conduit (FIG 1). If the patient has good-quality GSV, no further vein mapping is typically necessary. If the GSV is of poor quality or absent, small saphenous vein and arm vein should be mapped (FIG 2).
Ideal conduit diameter is 3.5 mm or greater.
Vein should be easily compressible. Thick-walled or noncompressible vein indicates prior superficial venous thrombosis and vein is likely not suitable for bypass.
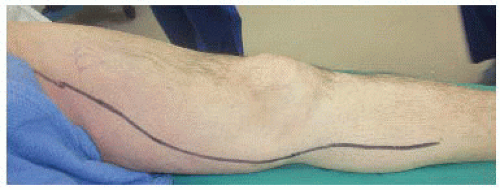
Mapping should ideally immediately precede surgery with vein course marked with an indelible marker on the skin. This allows precise placement of incisions, which avoids the creation of skin and tissue flaps that might impede wound healing.
SURGICAL MANAGEMENT
Preoperative planning
If not previously marked or if marks have faded, it is useful to remark the intended venous conduit with ultrasound guidance prior to surgery (FIGS 3 and 4).
Open foot lesions or gangrene should be covered with sterile adhesive to prevent contamination of sterile incisions.
Prophylactic intravenous antibiotics should be administered to reduce risk of perioperative infection.
If arm vein is to be harvested, it is important to avoid blood draws or intravenous lines in the intended arm(s). If veins from both arms are necessary, central venous access may be necessary.
Positioning
The majority of the procedures are performed with the patient supine. If small saphenous vein is the intended conduit, it is often easier to perform this part of the procedure with the patient prone and then to reprepare and drape with the patient supine.
If arm vein is to be harvested, the arms should be abducted and placed on arm boards.
TECHNIQUES
Open vein harvest: GSV
A longitudinal incision is made directly over the marked vein. Either a single incision or multiple skip incisions can be used, with some evidence of fewer wound infections with the latter approach (FIG 5).
The necessary length of vein is unroofed. Using blunt and sharp dissection with Metzenbaum scissors, the vein is freed from surrounding structures. Side branches are ligated and divided with silk ligatures and hemoclips.
The GSV is divided proximally at the saphenofemoral junction (FIG 6), distally according to the length of vein needed.
It is helpful distally to identify a branch point in the vein that can subsequently be used for the proximal anastomosis if the graft is placed in reversed configuration (FIG 7A,B).
Open vein harvest: small saphenous vein
The same technique is used as for the GSV, except typically with the patient prone.
Proximally, the vein is typically divided at the saphenopopliteal junction. Some patients will have continuation of the small saphenous vein in the thigh (Giacomini vein) which allows harvesting additional length of vein in the thigh.
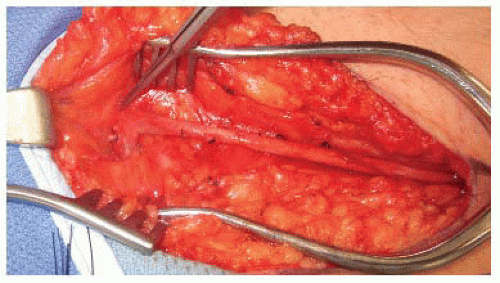
FIG 6 • GSV mobilized proximally to saphenofemoral junction. Side branches ligated with silk ligatures.
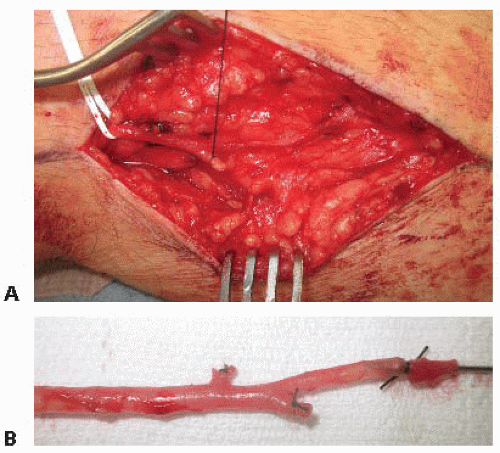
FIG 7 • A,B. Distal GSV divided at branch point to provide starting spot for proximal anastomosis of reversed vein graft.
Open vein harvest: arm vein
Both the cephalic and basilic veins can be harvested through longitudinal arm incisions. The same technique is used as for leg vein; however, care must be taken as the arm veins tend to be more thin walled and fragile than leg vein.
The cephalic vein can frequently be harvested as a single conduit from the wrist to the deltopectoral groove (FIG 8A-C). A single segment is frequently adequate for a femoral-popliteal or femoral to proximal tibial bypass.
The basilic vein tends to be larger in diameter than the cephalic vein, although often, only a short segment in the upper arm is available. The basilic vein is well suited for use as an extension graft when revision of a previously placed bypass is necessary. When used as a new bypass, a composite graft composed of two or more vein segments is frequently necessary.
The basilic vein often has large branches that communicate medially with the brachial vein. These branches are often broad based and are better ligated with a running monofilament suture than simple ligation.
The median antebrachial cutaneous nerve frequently interdigitates with the basilic vein. With meticulous dissection, this nerve can be preserved (FIG 9).
Brachial vein is intimately associated with both the brachial artery and median nerve. This vein can also be harvested as conduit, but great care needs to be taken to avoid injury to adjacent structures (FIG 10).
Open harvest: femoral vein
Although typically used for larger vessel reconstruction, femoral vein can be used for autogenous lower extremity bypass if necessary.
Proximal femoral vein is harvested medial to Sartorius muscle. Vein is adjacent to superficial femoral artery. Vein can be harvested proximally up to the profunda femoral vein.
Distally, the femoral vein is easier to harvest with the Sartorius muscle reflected posteriorly. The vein can easily be harvested as far as the adductor canal.
If a longer segment is needed, the vein can be further harvested caudal to the adductor tendon into the popliteal fossa.
Endoscopic harvest: GSV
Endoscopic harvest works best for veins within the saphenous fascial envelope (FIG 11A). It is technically more difficult in cases where the vein leaves this fascial envelope and is situated more
superficially or in the subcutaneous fatty tissue (FIG 11B).
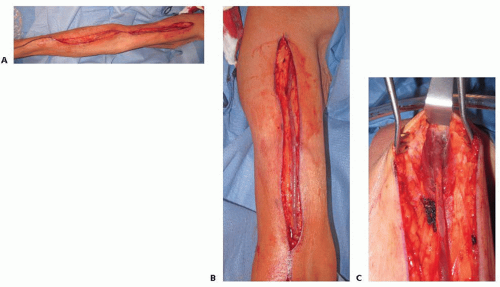
FIG 8 • A. Cephalic vein harvested the full length of the arm with skin bridge at antecubital fossa. B. Upper arm cephalic vein. C. Cephalic vein harvested medially to deltopectoral groove.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access