Management of Injuries to Kidneys, Ureter, or Bladder
This chapter describes techniques that are useful for management of injuries to the urinary system. Many renal injuries are managed nonoperatively; however, when an operative approach is required it is important to have a plan for approach and management as described here. Ureteral injuries are sometimes iatrogenic, but may also result from external trauma. Simple repair is described here and more complex techniques are referenced. Bladder repair is an essential tool for management of colovesical fistula as well as trauma and is described in this chapter.
SCORE™, the Surgical Council on Resident Education, classified repair of renal, ureteral, or bladder injuries as “ESSENTIAL UNCOMMON” procedures.
STEPS IN PROCEDURE—OPERATIVE APPROACH TO RENAL TRAUMA
Preliminary vascular control
Mobilize bowel to expose renal vein and artery in midline
Isolate renal artery and place Silastic loops for rapid control
Isolate renal vein and place Silastic loops for rapid control
Mobilize bowel to expose perinephric hematoma
Enter hematoma and rapidly but atraumatically mobilize kidney
Take care not to strip capsule from renal parenchyma
Occlude renal artery and vein if major hemorrhage is encountered
Identify injury and determine if collecting system has been entered
Simple laceration
Close collecting system with running absorbable suture
Close parenchyma with interrupted sutures, using pledgets
Place drain
Major injury limited to lower or upper pole
Perform partial nephrectomy
Ligate branch of renal artery and vein entering pole
Sharply amputate devascularized portion
Obtain hemostasis in remnant
Close collecting system with running absorbable suture
Close parenchyma with pledgeted sutures
Place drain
HALLMARK ANATOMIC COMPLICATIONS
Urinary leak
Ureteral stricture
LIST OF STRUCTURES
Kidney
Renal artery
Renal vein
Ureter
Adrenal gland
Inferior vena cava
Aorta
Bladder
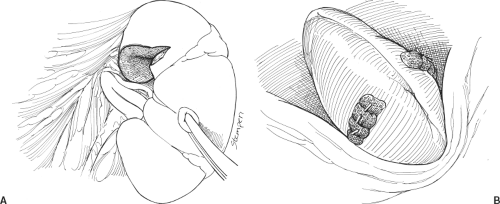
Exposure of Kidney and Suture of Laceration (Fig. 107.1)
Penetrating injuries to the perinephric region require exploration and repair. It is crucial that the initial mobilization be done efficiently with minimal blood loss, and that no additional damage be done to the kidney during mobilization. The capsule is easily stripped from the renal parenchyma. Take care to preserve the capsule, as it is the part that best holds the suture.
Mobilize overlying colon by incising the avascular line and allowing the colon and its mesentery to come to the midline. Carefully inspect the colon and mesentery for injuries as you do this. This should expose the underlying perinephric hematoma.
Decide whether or not to perform preliminary vascular control by isolating the renal artery and renal vein in the midline,
away from the hematoma. Some surgeons routinely obtain preliminary control and others do it selectively. Preliminary vascular control allows the perinephric hematoma to be explored with minimal additional blood loss; however, it may require significant additional time (and associated continued blood loss into the hematoma). Many surgeons use preliminary vascular control selectively, employing it when the nature of the injury or the appearance of the hematoma suggests that major arterial bleeding will be encountered on exploring the injury.
away from the hematoma. Some surgeons routinely obtain preliminary control and others do it selectively. Preliminary vascular control allows the perinephric hematoma to be explored with minimal additional blood loss; however, it may require significant additional time (and associated continued blood loss into the hematoma). Many surgeons use preliminary vascular control selectively, employing it when the nature of the injury or the appearance of the hematoma suggests that major arterial bleeding will be encountered on exploring the injury.
To obtain preliminary vascular control, isolate the renal artery and vein outside the hematoma in the midline. See Chapters 108e and 109 for a discussion of the relevant anatomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree