Malignant Melanoma
Brian J. Hall, MD
Key Facts
Clinical Issues
Knowledge of clinical dimensions is of maximum importance
Ensure viewing entirety or most of the lesion before making a benign diagnosis
Can be difficult, especially in cases of giant congenital melanocytic nevus (CMN)
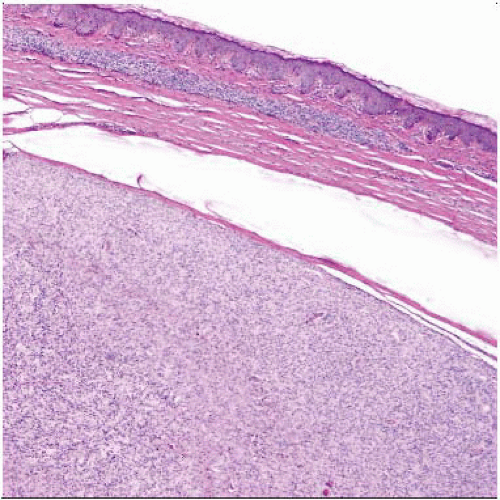
Microscopic Pathology
Asymmetry of lesion
Probably most powerful criterion for diagnosing melanoma
Lack of circumscription
Pagetoid spread of single melanocytes above basal layer, especially at periphery of lesion
Lack of maturation
Lack of dispersion
Deep dermal mitoses
Pigment deep in lesion
Solitary epidermal melanocytes predominating over nests
Reporting Considerations
Breslow thickness, not histologic subtype, is most important prognostic parameter
Presence or absence of ulceration changes stage
Malpractice Considerations
Expert consultation recommended before diagnosing melanoma in any pediatric patient
Due to wide range of histologic features and subtypes of melanomas
Diagnosis of melanoma should be considered when encountering any unusual cutaneous malignancy
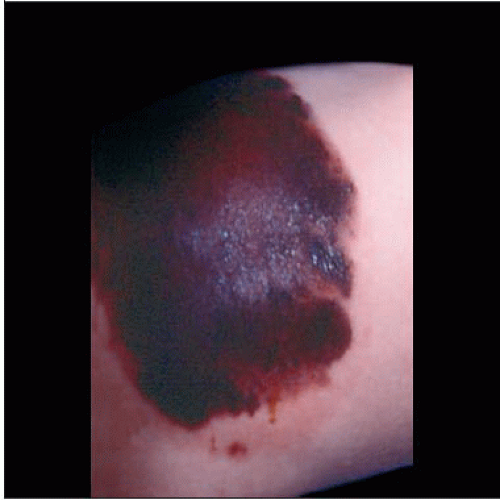 This is a giant congential pigmented nevus on the back of a newborn, in which a melanoma that was ultimately fatal developed. |
TERMINOLOGY
Abbreviations
Malignant melanoma (MM)
Definitions
Malignant cutaneous melanocytic neoplasm
CLINICAL ISSUES
Epidemiology
Incidence
Accounts for 1-3% of all childhood malignancies
7x more frequent in 2nd decade than 1st decade of life
< 1% of all melanomas occur in prepubertal children (< 14 years old)
On the rise in children and teenagers
Accounts for < 0.5% of all melanomas
Age
Prepubescent melanoma
Develop transplacentally, de novo, within a congenital melanocytic nevus (CMN) or in association with another cutaneous lesion
Congenital and infantile melanomas are rare
Postpubescent melanoma
> 14 years of age
Clinical features and prognosis tend to resemble adult counterparts
Gender
Slight female predominance
Site
Can occur anywhere on the skin
Rarely mucous membranes and meninges
Presentation
50% arise in association within preexisting lesion
30% arise within a giant CMN (> 20 cm)
50-70% will arise before puberty
Tend to arise within the dermis
Worse prognosis
20% in association with other cutaneous lesions
Small to medium-sized CMNs
Acquired melanocytic nevi
More likely to occur after puberty
50% arise de novo
May arise with neurocutaneous melanosis
Rare but carries high risk of malignant transformation in children
Median age is 3 years old
Up to 2/3 of patients may develop primary intracranial melanomas
Signs and symptoms may include
Rapid increase in size of lesion, hemorrhage, ulceration, change in color, loss of previously regular borders, pruritus, lymphadenopathy
Important clinical signs (“ABCD”)
Asymmetry
Border irregularity
Color/pigmentation irregularities
Diameter of 6 mm or greater
“ABCD” changes of adult melanomas may be absent in pediatric patients
Risk factors
Fair skin
Giant CMN (bathing trunk nevus)
Risk correlates with size, depth, and number of melanocytes
Occurs in 1 in 20, 000 newborns
≥ 20 cm in largest diameter
Up to 5-7% risk of malignant transformation
Dysplastic nevus syndrome
Numerous acquired melanocytic nevi
Independent risk factor
Sporadic atypical nevi
Independent risk factor
Xeroderma pigmentosum
Albinism
Immunosuppression
Family history of melanoma (familial melanoma)
Occur at younger age
Often multifocal
Germline mutations of CDKN2A tumor suppressor gene
Treatment
Options, risks, complications
Surgical resection with standard margins
Treatment of choice in primary diseases
Potentially curative
May also include sentinel lymph node biopsy or regional lymphadenectomy
Both the National Comprehensive Cancer Network (NCCN) and the American Academy of Dermatology (AAD) publish online guidelines for surgical margins
Chemotherapy of minimal benefit
Experimental immunotherapy of unproven benefit
Treatment protocols based on adult population
Prognosis
Most important prognostic factors
Depth of invasion
Measured by Breslow thickness
Stage at diagnosis
Stage IV 5-year survival rate (34%)
Stage I-II 5-year survival rate (90%)
Other poor prognostic indicators
Previous nonmelanocytic malignancies, nodular histologic type, fusiform or spitzoid cytology, vertical growth phase
High dermal mitotic activity, ulceration, vascular invasion, age > 10 years, and presence of metastases at diagnosis
Overall 5-year survival (79%)
Survival characteristics similar to adult population
MICROSCOPIC PATHOLOGY
Histologic Features
Size usually > 7 mm
May or may not have ulceration
Asymmetry
Probably the most powerful histologic criterion
Nests showing
Variability in size and shape
Haphazard interval and array
Haphazard arrangement of solitary epidermal melanocytes
Solitary epidermal melanocytes predominate over nests
Poor circumscription
Lesion does not start or end in a nest
Difficult to discern where lesion starts and stops
Single melanocytes predominate at edge of lesion
Pagetoid spread of melanocytes
Ascent of single melanocytes above dermoepidermal (DE) junction
Can also be present in Spitz nevi (sometimes full nests) and acral nevi
Should not be in periphery of Spitz or acral nevi
Lack of maturation
Deeper melanocytes as large as superficial ones
Deep dermal mitoses
Pigment present deep in lesion
Atypical melanocytes
Atypical features not always present
May have marked nuclear pleomorphism
Melanocytes may be small and spindled or epithelioid
Confluence of melanocytes
Melanomas arising in giant CMN
When arising in type 1 CMN, usually arises at DE junction
When arising in type 2 CMN, usually arises in dermal component
Inflammatory infiltrate can be helpful especially if asymmetrical
Often seen surrounding invasive component
Cytologic Features
Classification of Pediatric Melanoma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree